Surgery
Portal Hypertension
Definition of portal hypertension when pressure of the portal vein exceeds 5 mm hg.
However, higher pressures (8 to 10 mm Hg) are typically required to begin stimulating the development of portosystemic collateralization.
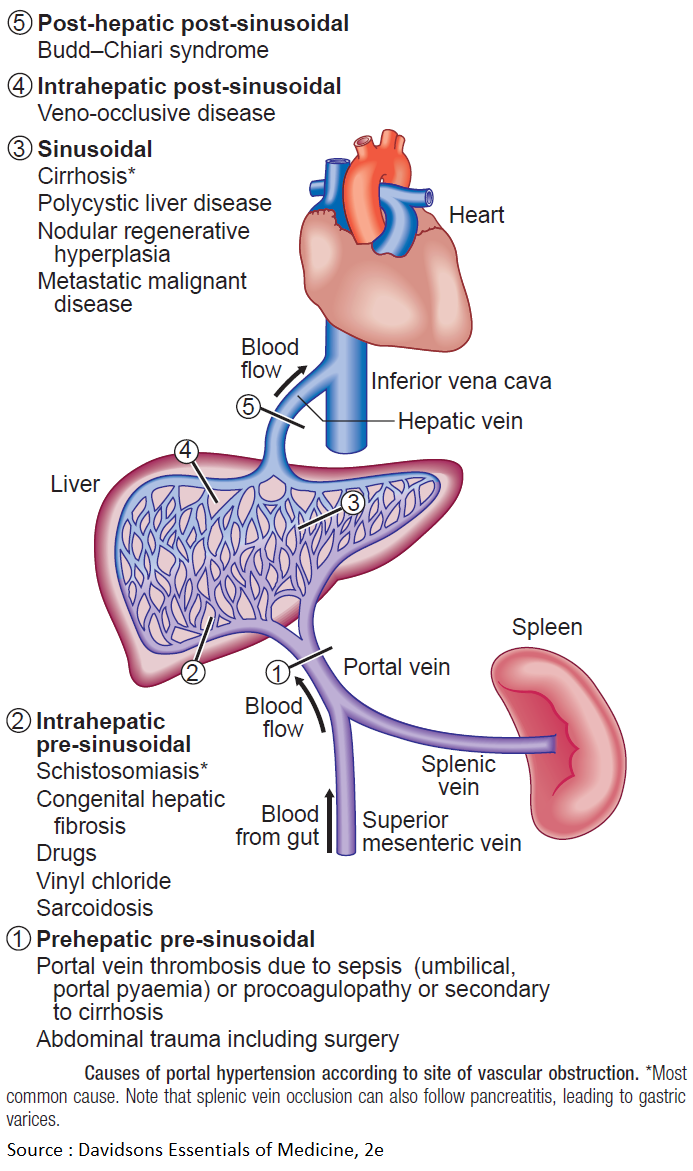
Its causes can be classified to
- Pre-hepatic
- Hepatic
- Post-hepatic
Most common cause is liver cirrhosis (hepatic).
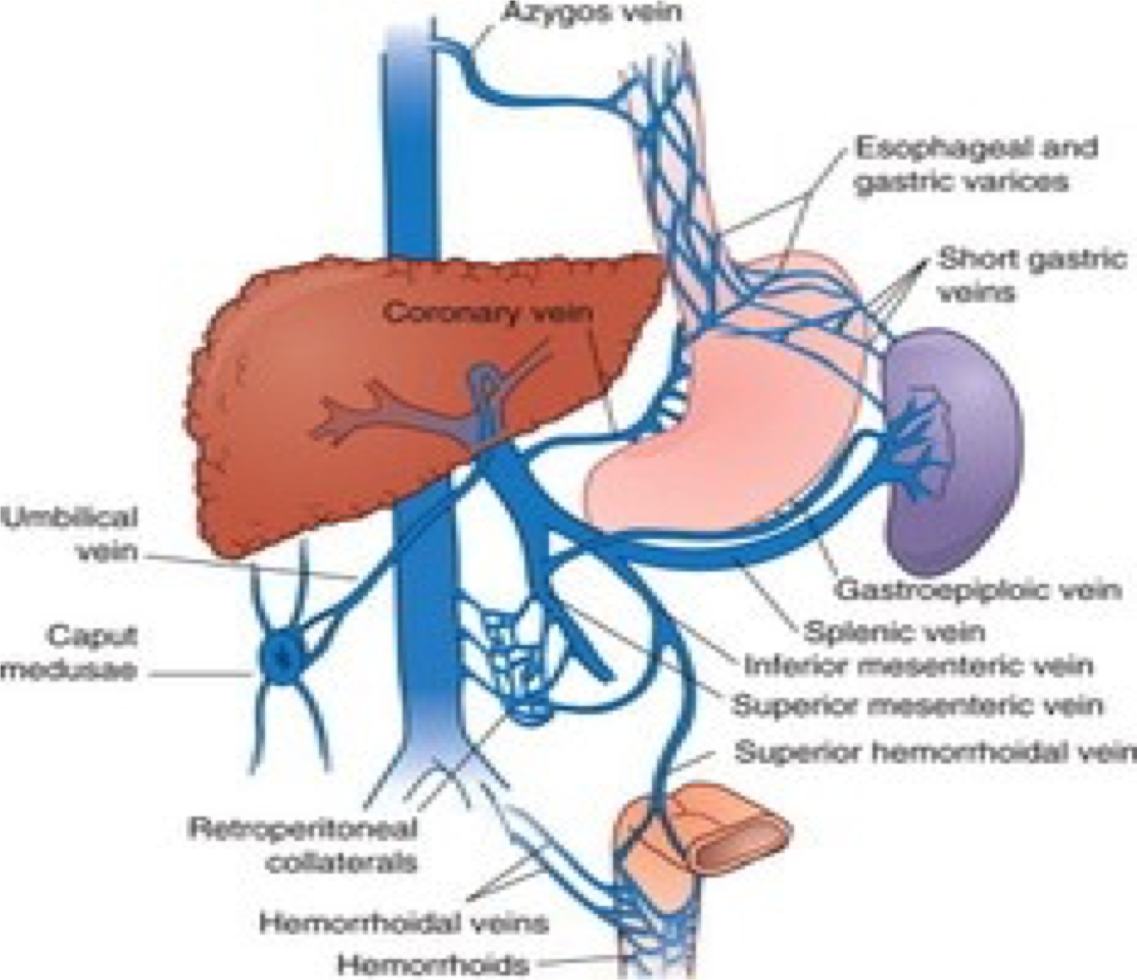
The main issue with hypertension is the development of collaterals to systemic circulation.
No treatment to tackle this process, treatment is targeted to complication and sequalae.
Portal hypertension is caused by increased resistance to portal blood flow. The normal pressure of 5 – 15 cmH2O in the portal vein is consistently exceeded.
Causes of portal hypertension
I- Obstruction to blood flow A. Presinusoidal extra-hepatic 1. Congenital atresia of portal vein 2. Portal vein thrombosis 3. Extrinsic compression of portal vein B. Presinusoidal intra-hepatic (schistosomiasis) C. Sinusoidal (cirrhosis) D. Postsinusoidal (Budd-Chiari syndrome, constrictive pericarditis)
II- Increased blood flow (Arterio-venous fistula)
Effect of portal hypertension
-
Formation of Porto-systemic shunting at three principal sites: a) Gastro-esophageal varices that may cause severe upper gastrointestinal bleeding b) Retroperitoneal and periumbilical collaterals “Caput medusa” that may cause excessive bleeding during surgery at these sites c) Anorectal varices that may cause lower gastrointestinal bleeding
-
Splenomegaly and related hypersplenism with pancytopenia
-
Ascites that my be complicated by primary peritonitis and respiratory compromise.
-
Encephalopathy due to increase level of toxins such as ammonia in the systemic circulation
Clinical features
- Patients with cirrhosis frequently develop anorexia, generalized malaise and weight loss.
- Clinical manifestations include jaundice, spider naevi, ascites and hepatosplenomegaly.
- Slurring of speech, a flapping tremor or dysarthria may point to encephalopathy.
Investigations
Laboratory tests: may show elevated bilirubin, with depressed serum albumin. Anemia may be present. The prothrombin time and other indices of clotting may be abnormal. Serology tests for hepatitis B, C may be positive as underlying cause for liver cirrhosis.
Assessment of patients with portal hypertension using Child-Turcott-Pugh system Y
| Criterion | 1 | 2 | 3 |
|---|---|---|---|
| Encephalopathy | None | minimal | marked |
| Ascites | none | Easily controlled | intractable |
| Bilirubin(µmol/l) | <35 | 35-50 | > 50 |
| Albumin(g/l) | > 35 | 28-35 | < 28 |
| Prothrombin ratio | < 1.7 | 1.7 – 2.3 | > 2.3 |
Grade A = 5-6 points , Grade B = 7-9 , Grade C = 10 -15
3 lab (Bilirubin, Albumin, Prothrombin) - 2 clinical (encephalopathy & Ascites) #Z
albumin is protein only produced by the liver
Child-Pugh Scoring System
| Points | 1 | 2 | 3 |
|---|---|---|---|
| Encephalopathy (grade) | None | 1-2 | 3-4 |
| Ascites | None | Slight | Moderate |
| Albumin (g/dL) | >3.5 | 2.8-3.5 | <2.8 |
| Prothrombin time prolonged (sec) | 1-4 | 4-6 | >6 |
| Bilirubin (mg/dL) | 1-2 | 2-3 | >3 |
| For primary biliary cirrhosis | 1-4 | 4-10 | >10 |
Class A = 5-6 points; Class B = 7-9 points; Class C = 10-15 points.
Treatment
-
Acute bleeding Gastroesophageal varices: Endoscopic banding or sclerotherapy injection. Uncontrolled bleeding may need surgical intervention.
-
Ascites: can be treated by restriction of water and salt intake followed by diuretics. In advanced cases may need portosystemic shunting.
-
Advanced cases of liver cirrhosis (child C) may need liver transplant as definitive treatment for the liver cirrhosis, portal hypertension and its complications.
Sites of Porto-systemic anastomosis in portal hypertension
IMAGING
Effects of Portal hypertension: Z
- Varices: Esophageal varices, piles.
- Splenomegaly due to splenic congestion.
- Ascites which is accumulation of transudate in the peritoneal cavity.
Definition:
elevation of hydrostatic pressure within portal vein or its tributaries (normally =5 mmHg so, if portal hypertension = 7 mmHg or 30 CM water)
Anatomy:
Union of superior mesenteric vein and splenic vein behind head of pancreas.
Causes:
*hepatic (cirrhosis)
Clinical picture:
1- congestion: *gastric: leading to dyspepsia
- intestinal : leading to constipation and diarrhea *spleen: enlarged spleen (left hypochondreal pain) hepatosplenomegally
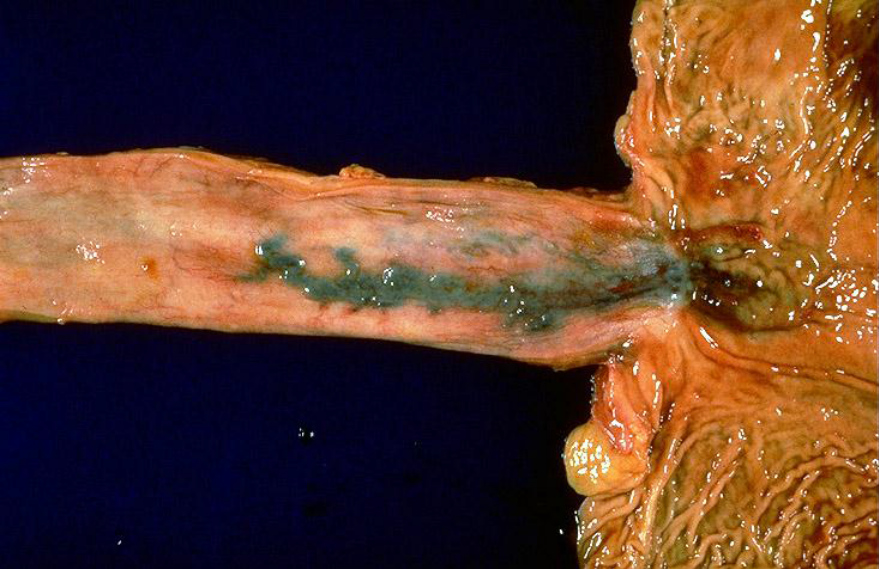
2-rupture Esophageal varices: *dilated elongated tortuous veins in the upper stomach , lower esophageus manifested by haematemesis and melena.
Prominent abdominal veins.

Esophageal Varices