BIRTH INJURIES
Prepared by:
*Dr. Salma Elgazzar *
Learning Objectives
- Recognize causes and pathogenesis of birth injuries.
- Recognize clinical presentation and differential diagnosis of birth injuries.
- Recognize management of birth injuries.
Definition
These are the injuries that occur during delivery. It is defined as an impairment of the neonate’s body function or structure due to an adverse event that occurred at birth like mechanical forces (i.e., compression, traction).
Incidence
- Significant birth injury accounts for fewer than 2% of neonatal deaths and stillbirths in the United States.
- It still occurs occasionally and unavoidably, with an average of 6-8 injuries per 1000 live births.
- Most birth traumas are self-limiting and have a favorable outcome.
- Nearly one-half are potentially avoidable with recognition and anticipation of obstetric risk factors.
Risk Factors
- Large babies: In general, larger infants are more susceptible to birth trauma. Higher rates are reported for infants who weigh more than 4500g.
- Maternal obesity.
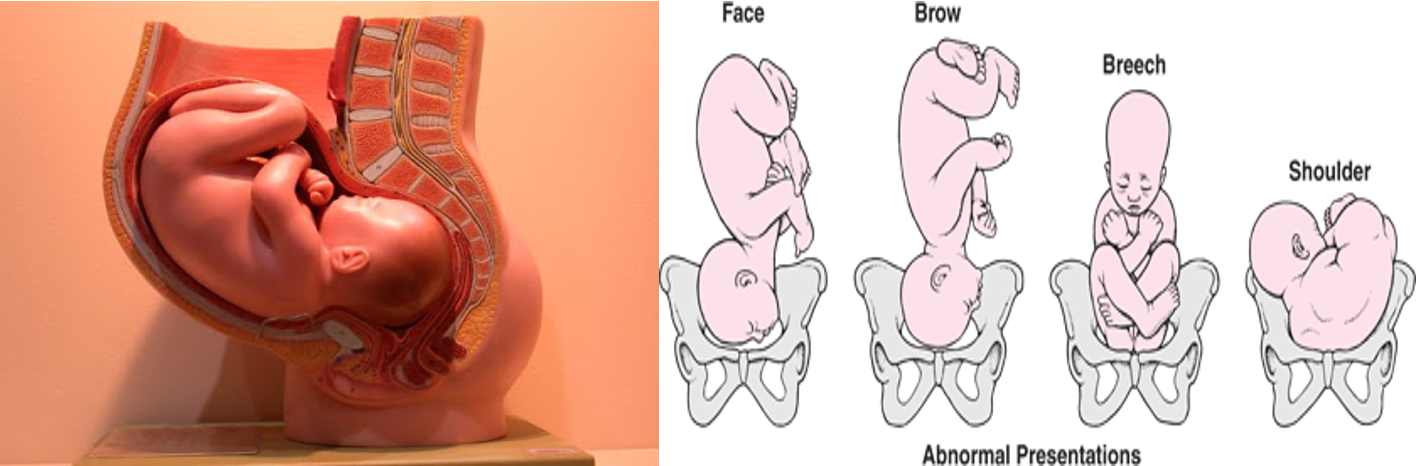
- Abnormal fetal presentation (fetal presentation other than a vertex position), particularly breech presentation.
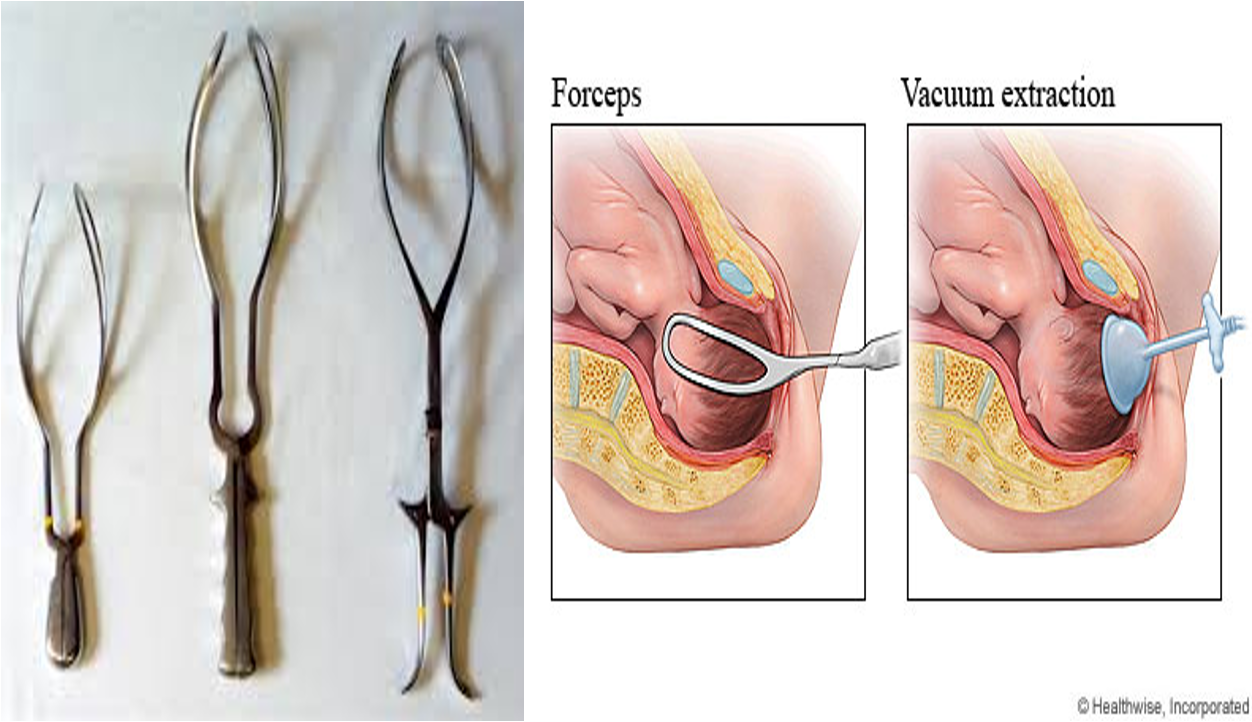
- Instrumental delivery (Forceps blades or at ventouse (vacuum) deliveries).
Other factors:
- Very small premature babies.
- Small maternal stature.
- Cephalopelvic disproportion (too large head for the pelvic outlet).
- Prolonged labor.
- Primiparous.
- Maternal pelvic anomalies.
Classification
-
A. Soft tissue injuries
-
B. Cranial injuries
-
C. Nerve injuries
-
D. Facial injuries
-
E. Visceral injuries
-
F. Fractures
-
G. Dislocation
Summary
-
Factors that increase the risk of birth injuries include macrosomia (fetal weight greater than 4000 g), maternal obesity, breech presentation, operative vaginal delivery (i.e., the use of forceps or vacuum during delivery), small maternal size, and the presence of maternal pelvic anomalies.
-
The most common form of traumatic birth injuries are soft-tissue injuries including bruising, petechiae, subcutaneous fat necrosis, and lacerations. Lacerations are the most common injury associated with cesarean delivery and are generally mild, requiring repair only with sterile strips. The other three conditions are generally self-limited and resolve without any intervention.
-
The extracranial injuries of caput succedaneum (edema of the scalp) and cephalohematoma (subperiosteal collection of blood) usually resolve spontaneously without any intervention.
-
Neurologic injury includes injury to peripheral nerves including the brachial plexus and facial, phrenic.
-
Facial injuries include nasal septal dislocation, which requires reduction by three days of life to avoid nasal septal deformity, and ocular injuries, which are usually mild and resolve without any intervention.
-
Intra-abdominal injuries due to birth trauma are rare and primarily due to rupture and subcapsular hemorrhage into the liver, spleen, and adrenal gland.
-
Fractures due to birth trauma include clavicular, humeral, femoral, and skull fractures. Since most clavicular and skull fractures resolve spontaneously, they are managed conservatively with observation alone.