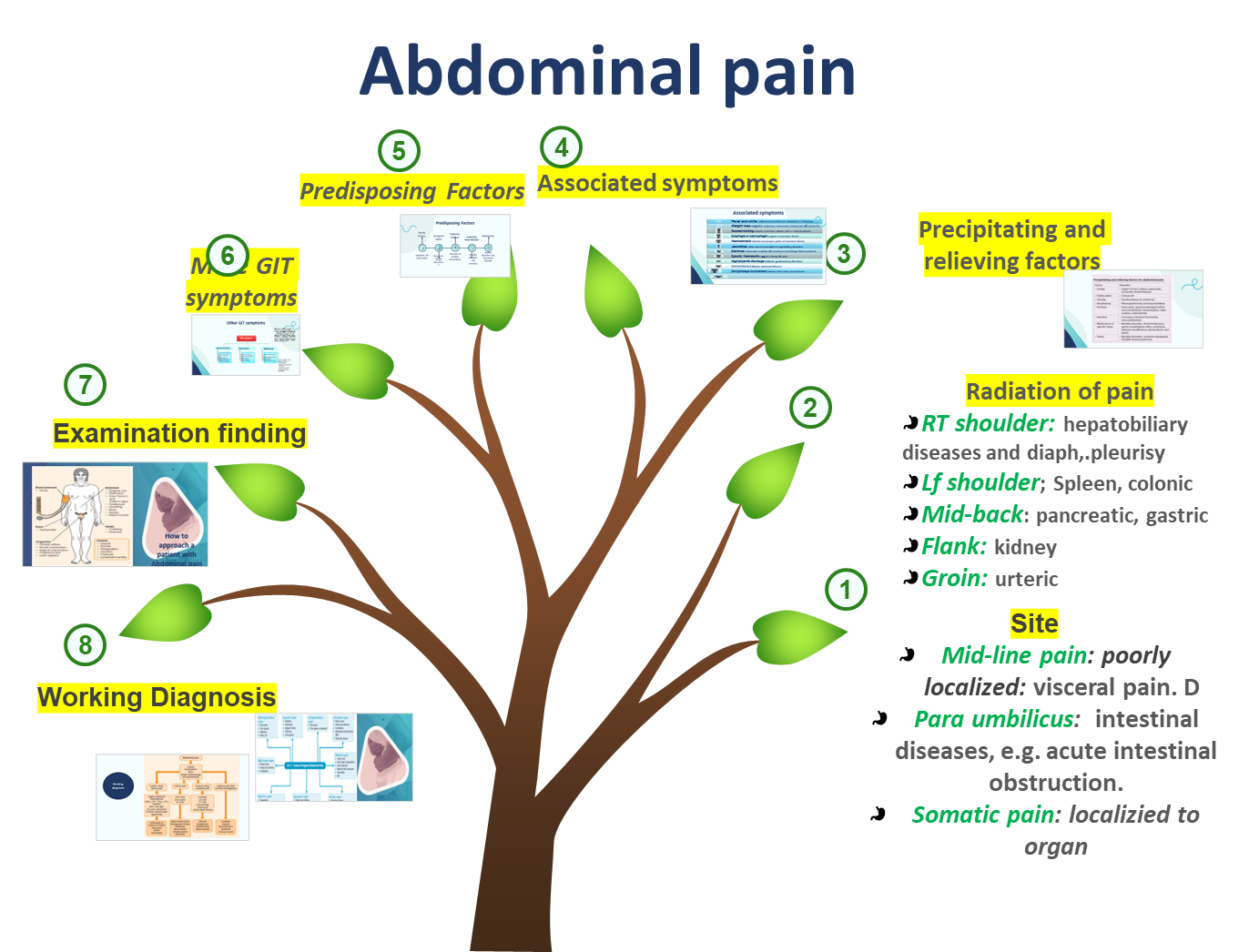
Abdominal Pain - Clinical Assessment
Overview
Abdominal pain is one of the most common presenting complaints in clinical practice, requiring a systematic approach to history taking and physical examination.
History Taking Framework
Associated Symptoms
- Fever and chills: Suggests inflammatory/infective diseases or infarction
- Weight loss: May indicate malignancy, malabsorption, tuberculosis, IBD, or ischemia
- Nausea/vomiting: Indicates obstruction, infection, IBD, or metabolic disease
- Dysphagia or odynophagia: Suggests esophageal disease
- Haematemesis: Indicates esophageal, gastric, and duodenal disease
- Jaundice: Due to hemolytic or hepatobiliary disorders
- Diarrhea: Malabsorption, infection, IBD, secretory tumors (Zollinger-Ellison syndrome)
- Dysuria/haematuria: Suggests urinary diseases
- Vaginal/penile discharge: Indicates genitourinary disorders
- Hematochezia: Indicates colorectal disease
- Skin/joint/eye involvement: Suggests inflammatory bowel disease
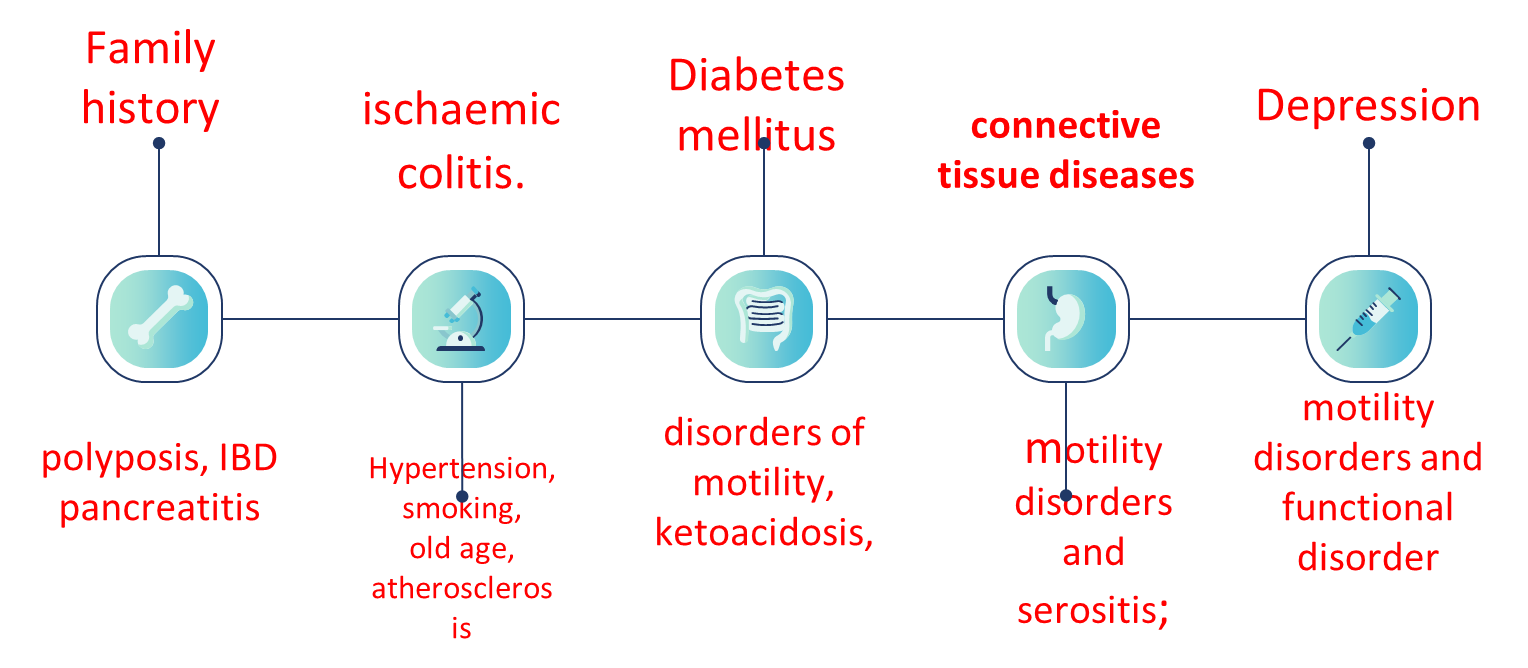
Predisposing Factors
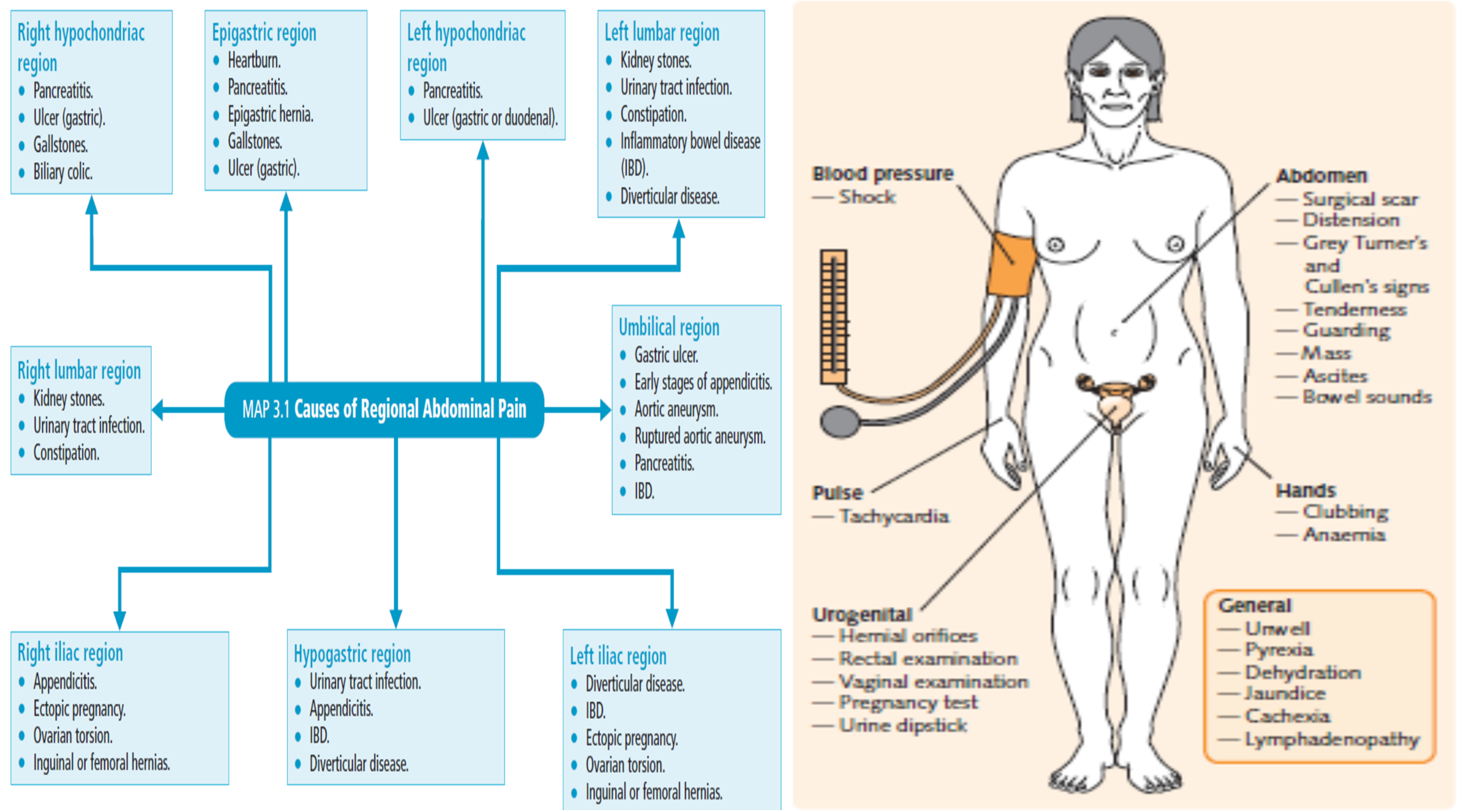
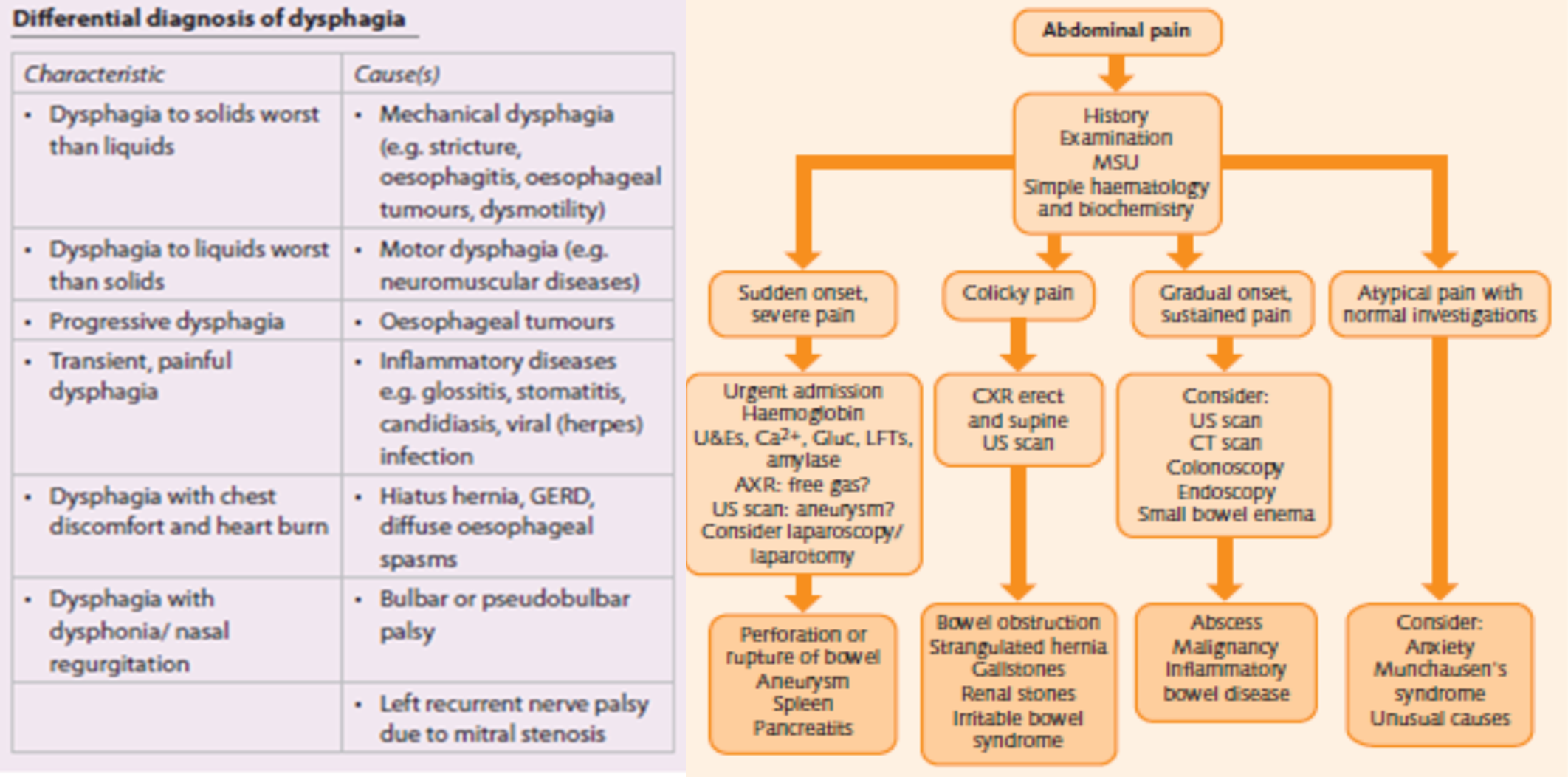
Systematic Approach to Abdominal Pain
Key Questions to Ask
- What is the site of pain?
- How severe is it?
- Is it continuous or intermittent?
- Does it radiate to any site or direction?
- What is duration of pain?
- Are there any pain-free intervals? (If yes, what is their duration?)
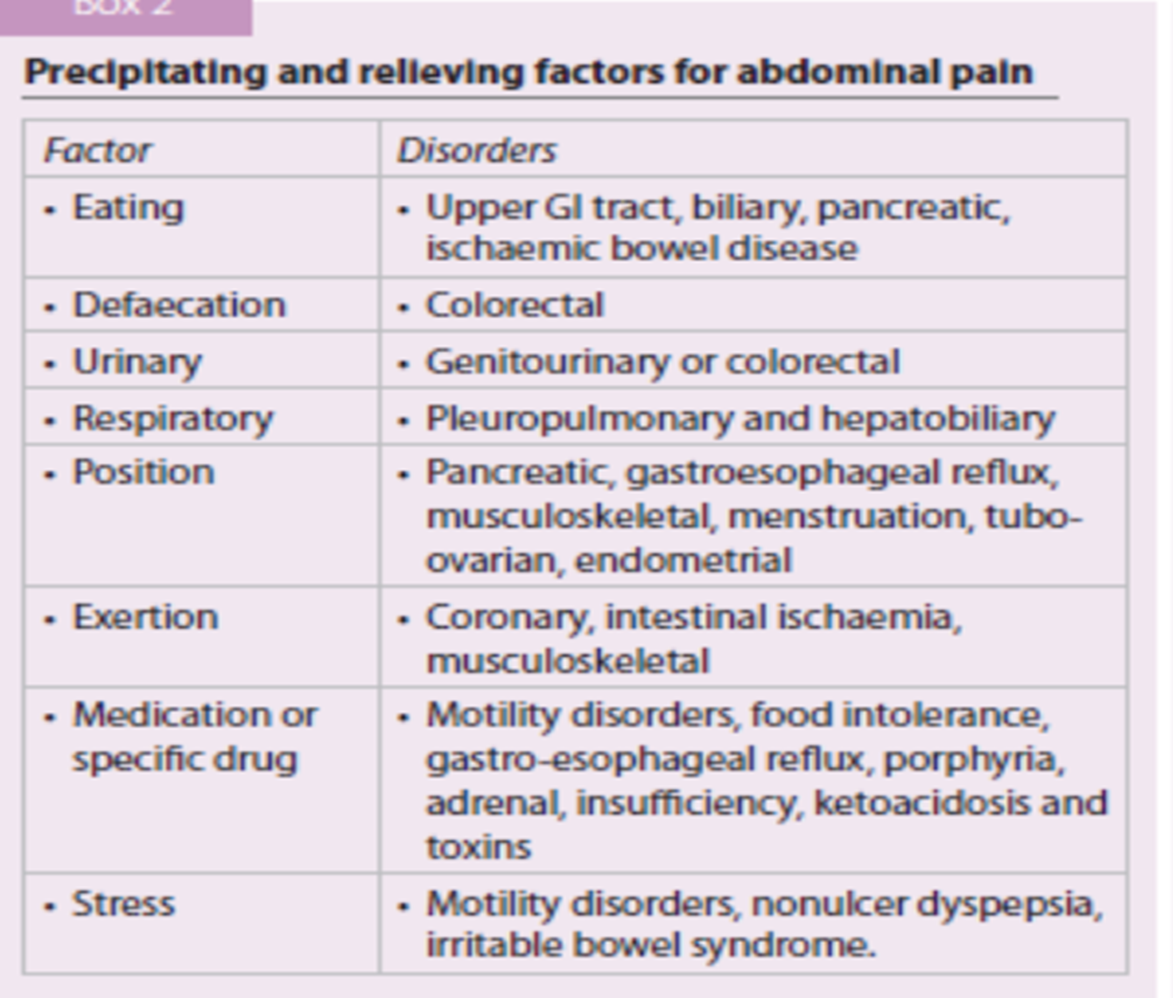
- Is pain related to meals?
- Does it disturb sleep at night?
- What are the aggravating factors?
- What are relieving factors? (e.g., food, vomiting, or antacid)
Appetite Assessment
- Is it increased or decreased?
- If reduced, is appetite poor or the patient afraid of taking food due to pain?
Medical Causes of Abdominal Pain
Hematological Disorders
- Porphyrias: Acute Intermittent Porphyria
- Lead Poisoning
- Polycythemia
- Congenital spherocytosis
- Sickle cell disease
Metabolic and Endocrine Diseases
- Diabetic precoma
- Pheochromocytoma
- Addison disease
- Familiar hyperlipidemia
Cardiovascular Causes
- Inferior MI (may present as epigastric pain)
Working Diagnosis
Related Clinical Skills
- Cs Abdominal pain - Clinical skills examination for abdominal pain
Cross-Reference
For family medicine approach and specific conditions, see: Level 10 Abdominal Pain