IM
Dr Waqar
DEFINITION
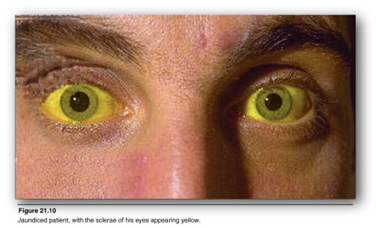
Yellow discoloration of sclera and mucous membranes due to bilirubin deposition is called jaundice.
ETIOLOGIES OF JAUNDICE
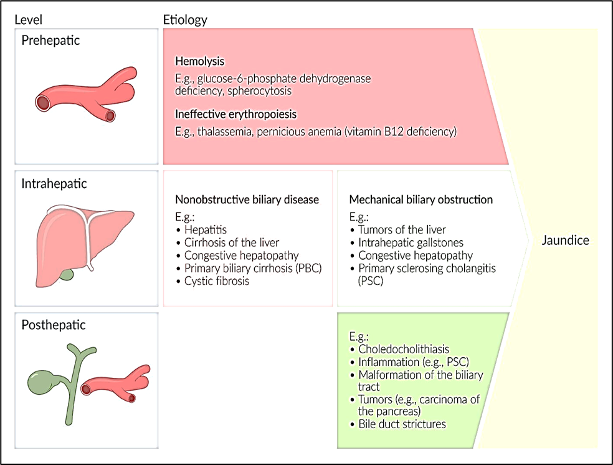
Etiologies
- Pre hepatic
- Hepatic
- Post hepatic
PREHEPATIC CAUSES
All hemolytic anemias (e.g., sickle cell disease, hereditary spherocytosis, etc.) So, ask about the history of any hemolytic anemia in the patient or in the family. Ask drug history (many drugs can cause hemolysis)
HEPATIC CAUSES
- Hepatitis A
- Hepatitis B & C (cases in hospitals are usually chronic Hep B & C)
- Cirrhosis (any chronic liver disease can lead to cirrhosis e.g., chr. Hep B, C, fatty liver)
- Primary biliary cholangitis
- Drug-induced hepatitis
1) Hep A:
- Recent travel history (eating street food, drinking unclean water)
- Recent restaurant visits (Hep A is spread by the fecal-oral route)
2) Chronic Hep B & C:
- Ask about IV drug abuse, any blood transfusion, any needle stick injury from a Hep B or C positive person, history of Hep B/C in the spouse or mother, use of unsterile syringes, history of multiple sexual partners, especially unknown people.
3) Cirrhosis:
- Same questions as for Hep B and C
- Ask about DM (causes fatty liver)
4) Primary biliary cholangitis:
- Female with jaundice, itching & xanthelasma (confirmation of PBC is by blood test)
5) Drugs:
- Take a drug history, even simple medicines
POST HEPATIC ETIOLOGIES
Ask about:
- Symptoms of gallstones
- Wt. loss (cancer)
- Stool color: Due to biliary obstruction, stools become pale
- Ask “are the stools easy to flush?”
Labs to do in Jaundice
CBC: Can show:
- Anemia
- Low platelets (cirrhosis)
2) PT/INR: High in chronic liver disease
3) LFTs: Abnormal
- In hepatic causes, AST and ALT are much higher than alkaline phosphatase, in post hepatic causes, alk phos is much higher
4) Serum albumin: Low in chronic liver disease
5) Check Hep B & C serology. Any other serologies depending on the cause
IMAGING
- Ultrasound
- CT/MRI (rarely)
- Biopsy (not always)
Complications of Cirrhosis RR
- Portal HTN
- Esophageal varices
- Ascites
- Hepatocellular carcinoma
Treatment
- Hep A: No specific treatment. Just good nutrition
- Hep B: Interferon + some other drugs
- Hep C: Oral meds. Now available
- Avoid any medicines which damage the liver
Treatment of complications
- Ascites: salt & water restriction, Diuretics (e.g., Aldactone)
- Esophageal varices: Sclerotherapy
In patients with cirrhosis, always rule out hepatocellular carcinoma by doing:
- Liver ultrasound every year
- Check blood levels of alpha-fetoprotein every year (very high in cancer)
SURGERY
Biliary
Classical symptoms of obstructive Jaundice
The why behind it all
-
Pruritis
- Bile salts reflux back into plasma, I/t mast cell degranulation in the skin
-
Clay coloured stools
- Conjugated bilirubin does not reach the gut, no sterco/urobilin, stools devoid of yellow colour
-
High coloured urine
- Conjugated bilirubin (soluble) diffuses into plasma, is filtered by kidney
Pain
-
RUQ pain and tenderness
- Stasis of bile in ducts l/t inflammatory response causing pain
- Elicited as tenderness (irritation of parietal peritoneum) and palpable lump (omentum)
-
Biliary colic
- A misnomer as CBD in most individuals does not contain muscle layers
- Stasis leads to release of inflammatory mediators (phospholipase A2 and prostaglandins)
| Benign | Malignant | |
|---|---|---|
| Choledocholithiasis* | Carcinoma gall bladder | |
| Primary sclerosing cholangitis | Periampullary carcinoma | |
| Post-surgical stricture | Cholangiocarcinoma | |
| Pancreatitis | Carcinoma of the head of pancreas | |
| Parasitic infections | Obstruction due to metastatic LN |
Features
Calculous obstruction: Younger patient, intermittent abdominal pain, fatty dyspepsia, fluctuant jaundice, dark urine, pale stool, pruritus (bile salt deposits)
Neoplasia: Older age, painless/ mild discomfort, weight loss, progressive jaundice, dark urine, pale stool, pruritus, Courvoisier sign, hepatomegaly
Hepatocellular: Stigmata of CLD- liver palm, spider naevi, gynecomastia, signs of PH (splenomegaly, ascitis, caput medusae), hepatomegaly
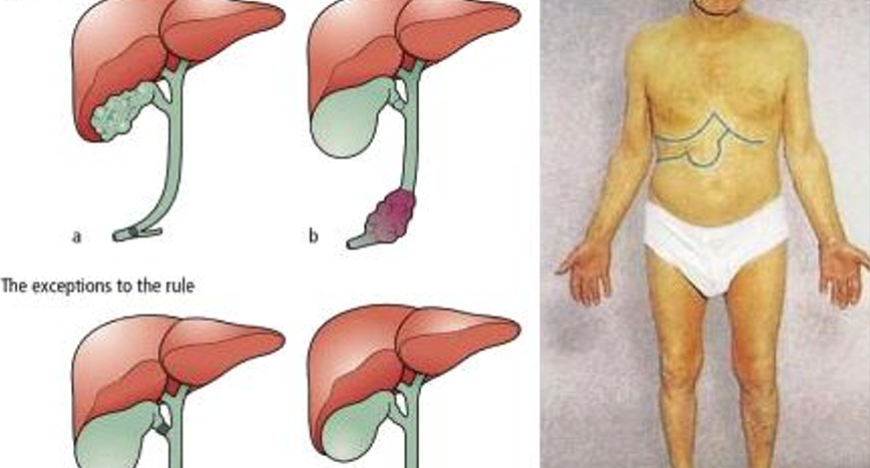
Courvoisier’s law/sign Z
-
In the presence of jaundice, a palpable gallbladder is unlikely to be due to gallstone
-
More likely MALIGNANT to be due to carcinoma eg, carcinoma of head of pancreas
-
If the CBD is obst. due to calculus, the GB is usually not distended owing to previous inflammatory fibrosis.
-
If CBD is obstr. due to malignant growth, the GB becomes distended in order to reduce the press. in the biliary system.
-
In presence of enlarged g b associated with jaundice, the cause is unlikely to be gall stone
-
This classic clinical sign first appeared in the 1890 edition of the book “The pathology and surgery of the gallbladder” by the Swiss professor Ludwig Georg Courvoisier
Laboratory Investigations
- Blood test (Hemoglobin, WBC, Platelets)?
- Coagulation Profile
- Hepatic profile
- Hepatitis profile
- Tumour marker
Blood test (Hemoglobin, WBC, Platelets)? ⇒ infections. Hemolysis - Coagulation Profile (PTT, INR,..)? ⇒ in liver failure patients the tendency of bleeding is high, (vit. K deficiency—? because this is lipid soluble vitamin so it will not be absorbed because of the live unable to produce bile which is responsible for lipid absorption. and unable to produce clotting factors) Antibody assay? ⇒ rule out infectious and autoimmune diseases Surface antigen? ⇒ look for hepatitis virus Total and fractional Bilirubin ⇒ see the summery slide
Alkaline phosphatase and Gamma GT
Alk Phosphatase
- Liver, bone, placenta and intestine.
- Used mainly as indicator of ductal causes: partial obstruction of bile ducts, primary biliary cirrhosis, sclerosing cholangitis
- Elevated in all extra hepatic obstruction with values greater 3-5 times the normal.
Gamma GT
- Very sensitive for hepatobiliary diseases.
- Mainly it increases in ductal injury
- In case of increase in alkaline phosphatase GGT is a good test to exclude the bone source of ALP
- Source: Bone and Liver, how to differentiate.
AST & ALT Necroinfalammatory
- AST (aspartate aminotransferase): liver, cardiac muscle, skeletal muscles, kidneys, brain, pancreas
- ALT (alanine aminotransferase) liver, skeletal muscle
- Used as indicator of liver cell injury
- ALT is more specific
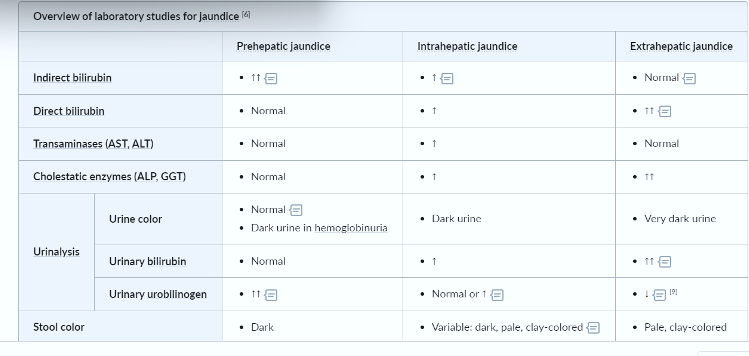
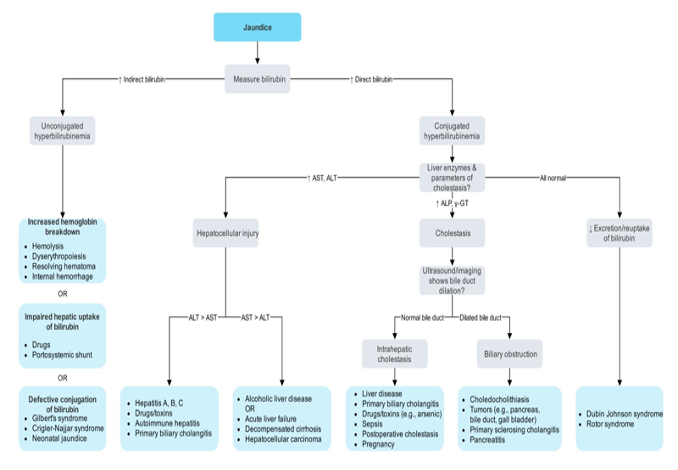
Haemolytic jaundice
- High unconjugated (indirect) serum bilirubin
- No bilirubin in urine
- Normal liver enzymes
Obstructive jaundice
- Serum conjugated bilirubin↑ - 50% of total: more suggestive of post hepatic than hepatic jaundice
- ALP ↑
- Transaminases: normal/ moderately elevated
- Fecal urobilinogen: ↓ -incomplete obstruction, absent - complete obstruction
- Urobilinogen in urine: absent in complete obstructive jaundice with ↑ bilirubinuria.
Treatment options for obstructive jaundice
- Antibiotic therapy (if indicated for infection)
- Intravenous fluids
- Pain medications, nutritional support
- ERCP: biopsy, stone removal, dilatation, stent placement (NEVER TUMOUR)
- Surgery: Curative resection, palliative by-pass
- Adjuvant therapy for cancer: chemotherapy, or radiotherapy
LIVER
Pathogenesis
Jaundice is caused by an increase in the level of circulating bilirubin and becomes obvious in the skin and sclera when levels exceed 50 µmol/ l.
Bile flow Causes of Jaundice
-
Pre hepatic
- transfusion reactions
- hemolysis secondary to sepsis, drugs or hematological diseases such as hereditary spherocytosis , sickle cell anemia
-
Hepatic
- hepatitis (e.g. viral hepatitis a, b, c)
- cirrhosis
- drugs
-
Post Hepatic (Biliary Obstruction – Surgical Jaundice)
- A- Intraluminal - gallstones
- B- Intramural
- benign biliary stricture (ischemic, traumatic, primary sclerosing cholangitis)
- primary cancer (cholangiocarcinoma, Ampullary carcinoma)
- C- Extramural
- secondary carcinoma (e.g. portal nodes)
- carcinoma on the head of pancreas
- chronic pancreatitis with pressure on distal CBD
Diagnosis
History and physical examination
-
a) Detailed history of the age, sex, occupation, social habits, drug and alcohol intake, history of drug injection or blood transfusion.
-
b) History of intermittent pain, fluctuating jaundice and dyspepsia suggest calculus obstruction of the common bile duct.
-
c) History of weight loss and progressive jaundice favors diagnosis of neoplasia.
-
d) Obstructive jaundice is likely if there is a history of passage of dark urine, pale stools and pruritus (owing to inability to secret bile salts into the obstructed biliary system)
-
e) Hepatocellular jaundice is likely if there are stigmata of chronic liver disease such as liver palms, spider naevi, testicular atrophy, and gynaecomastia
-
f) The abdomen must be examined for evidence of hepatomegaly, or distended gallbladder and for signs of portal hypertension such as splenomegaly, ascites and large collateral veins “caput medusa” in the abdominal wall
Biochemical and hematological investigations
-
a) Complete blood count: anemia may signify occult blood loss or hemolysis and low white cell and platelets count may indicate hypersplenism.
-
b) Coagulation screening: prolongation of prothrombin time may be present in both hepatocellular and obstructive jaundice and should be corrected with administration of vitamin k
-
c) Liver function test: in jaundice due to biliary obstruction, the circulating bilirubin is conjugated and rendered water-soluble; it can then excreted in the urine and gives it a dark color. as bile can not pass to the gastrointestinal tract, the stool becomes pale and urobilinogen is absent from the urine. obstruction increase the formation of alkaline phosphatase from the cells of bile ducts. serum transaminase levels may raise in obstructive jaundice. however they significantly raised in hepatocellular injury.
Radiological investigations
If the clinical picture and biochemical investigations suggest that jaundice is obstructive, radiological technique can be used to define the site and nature of the obstruction.
a) Ultrasound: obstructive jaundice is diagnosed by biliary dilatation, especially the intrahepatic bile ducts and it can follow down the cause of biliary obstruction. ultrasound can show gallstone, common bile duct stone, space occupying lesion in the liver, liver metastases, ascites. gallstone can appear as hyper-echoic shadow with classical ‘acoustic shadowing’ in ultrasound.
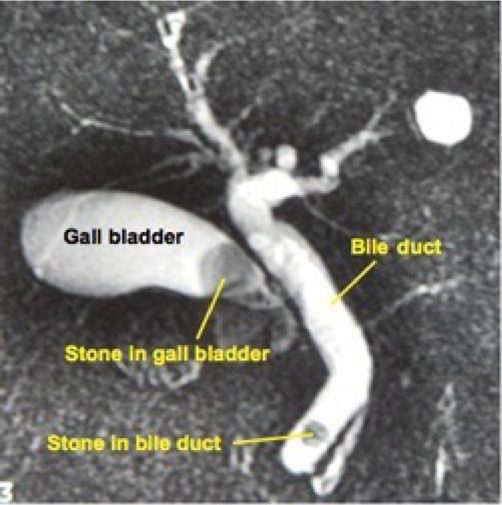
b) Magnetic resonance imaging (MRI): magnetic resonant cholangiopancreatography (MRCP) is non-invasive tool to assess the biliary system. MRI can assess for any lesion causing biliary obstruction such as pancreatic tumor or cholangiocarcinoma.
MRCP showing stone in the common bile duct and in the gallbladder
c) Endoscopic retrograde cholangiopancreatography (ERCP): ERCP is an invasive diagnostic and therapeutic investigation which outline the biliary and pancreatic system by injecting contrast through a cannula inserted into the papilla of Vater by means of side viewing endoscope passed into the duodenum. it gives more detailed information than ultrasound and allows endoscopic extraction of common bile duct stones, biopsy of periampullary tumors, and relief of obstructive jaundice by stent insertion. complications of ERCP included acute pancreatitis, cholangitis, duodenal perforation and bleeding. *NEVER USED IN CASE OF CANCER - COMPLICATED CHOLANGITIS *
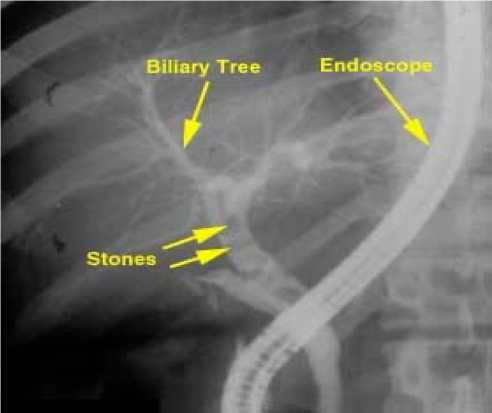
ERCP showing stone in the bile ducts
d) Percutaneous transhepatic cholangiography (PTC): it is invasive investigation used to outline the proximal biliary tree in obstructive jaundice by injecting contrast through slim flexible needle passed percutaneously to the liver parenchyma and biliary system.

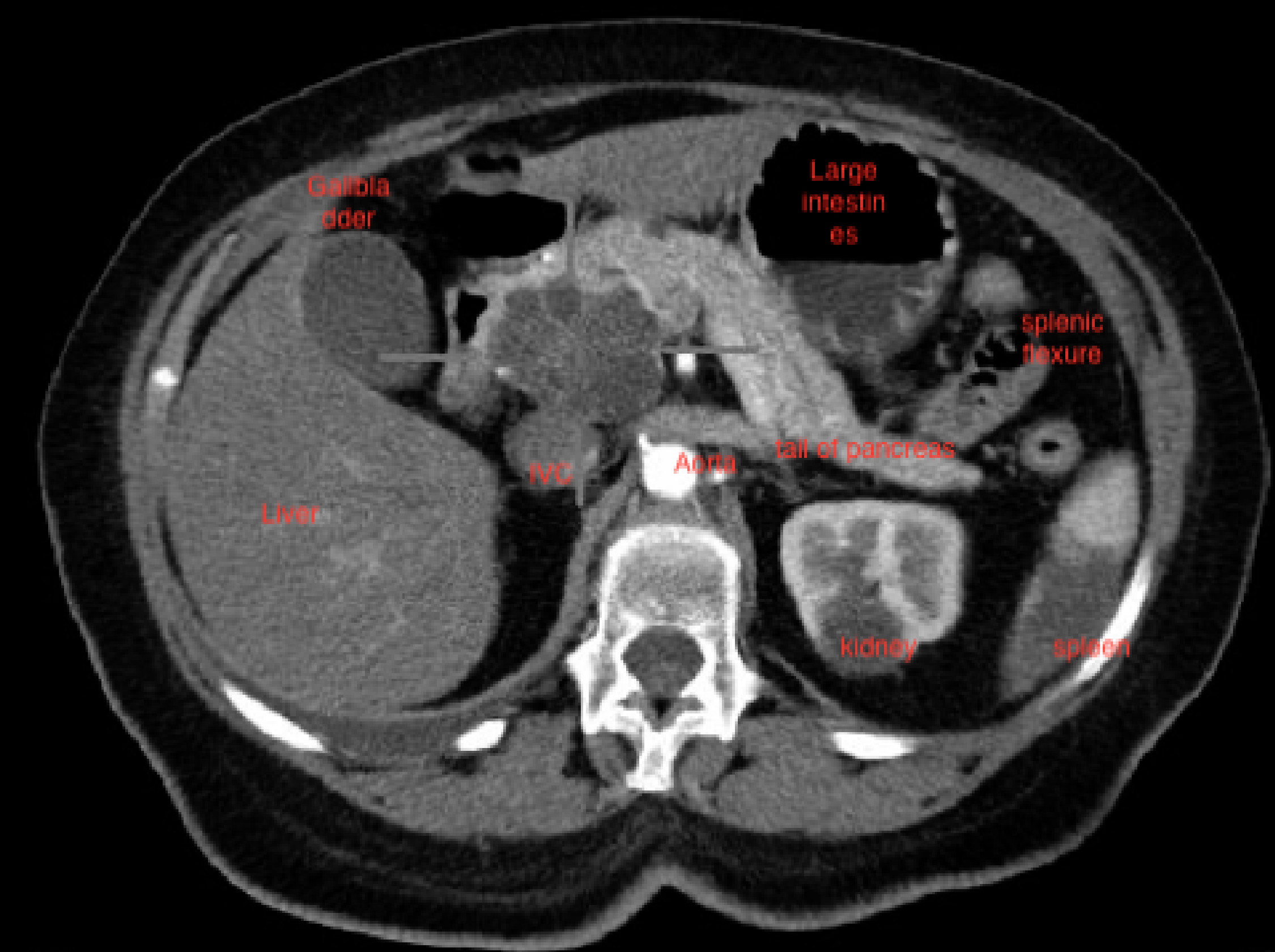
e) Computed tomography (CT): contrast enhanced CT scan can be used to identify and stage hepatic, bile duct and pancreatic tumors in obstructive jaundice due to these tumors.
CT scan showing tumor in the head of pancreas
Liver biopsy
Liver biopsy may be considered in patients with unexplained jaundice, in whom an obstructing lesion has been excluded radiologically.
Laparoscopy
Laparoscopy under general anesthesia may be used in the evaluation of liver disease. in selected patients with malignancy of liver, biliary tree, and pancreas, it may have a role in the staging of the tumor t exclude peritoneal or liver dissemination.
BIO Thera
Yellow color of skin, mucous membranes & sclera caused by deposition of bilirubin secondary to increased bilirubin levels in blood (hyperbilirubinemia)
JAUNDICE IS NOT A DISEASE HOWEVER, IT IS A SIGN OF AN UNDERLYING DISEASE
Pseudojaundice [14]
- Carotenoderma: Deposition of carotene in the skin cause yellow-orange skin. Due to excessive consumption of beta carotene (e.g., carrots, sweet potatoes, kale, oranges)
- Addison disease: hyperpigmentation of skin by increased melanin synthesis
Types of Jaundice = hyperbilirubinemia
Adult jaundice divided into prehepatic, intrahepatic, and posthepatic etiologies. The most common causes of adult hyperbilirubinemia can be remembered with the mnemonic “HOT Liver”: Hemolysis, Obstruction, Tumor, and Liver disease.
- Hemolytic Jaundice (Pre hepatic) (Unconjugated)
- Obstructive Jaundice ((Post) hepatic) (Conjugated)
- Hepatocellular Jaundice (Hepatic) (mixed)
Neonatal Jaundice
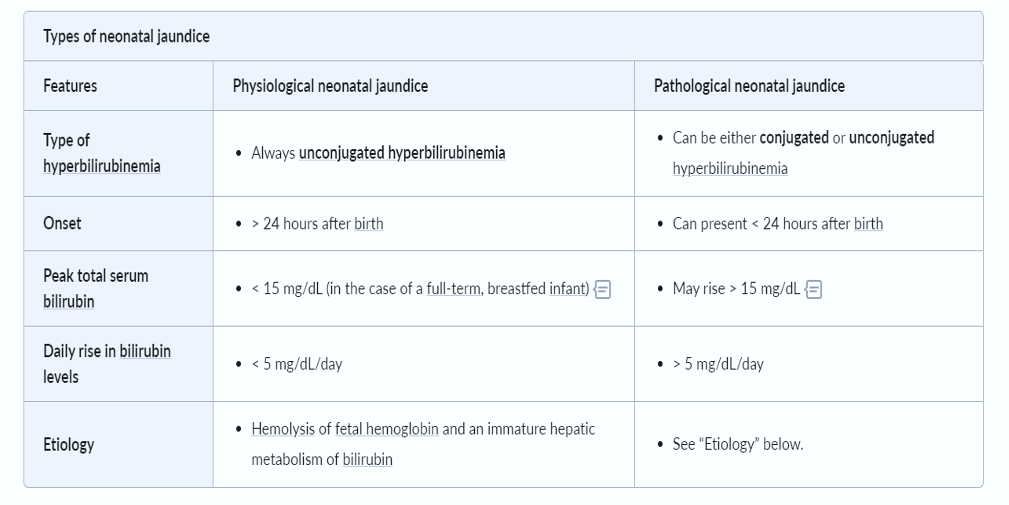
Medicine
Yellowish discoloration of the sclera of the eyes, mucous membrane , and skin •
Types of jaundice
- Prehepatic; If it is associated with pallor
- Hepatic; If it is associated with fever ⇒ (viral hepatitis )
- Post hepatic; if it is associated with pruritus Imaging is used to determine the site (e.g. distal common bile duct) and, if possible, the cause of obstruction.
Imaging
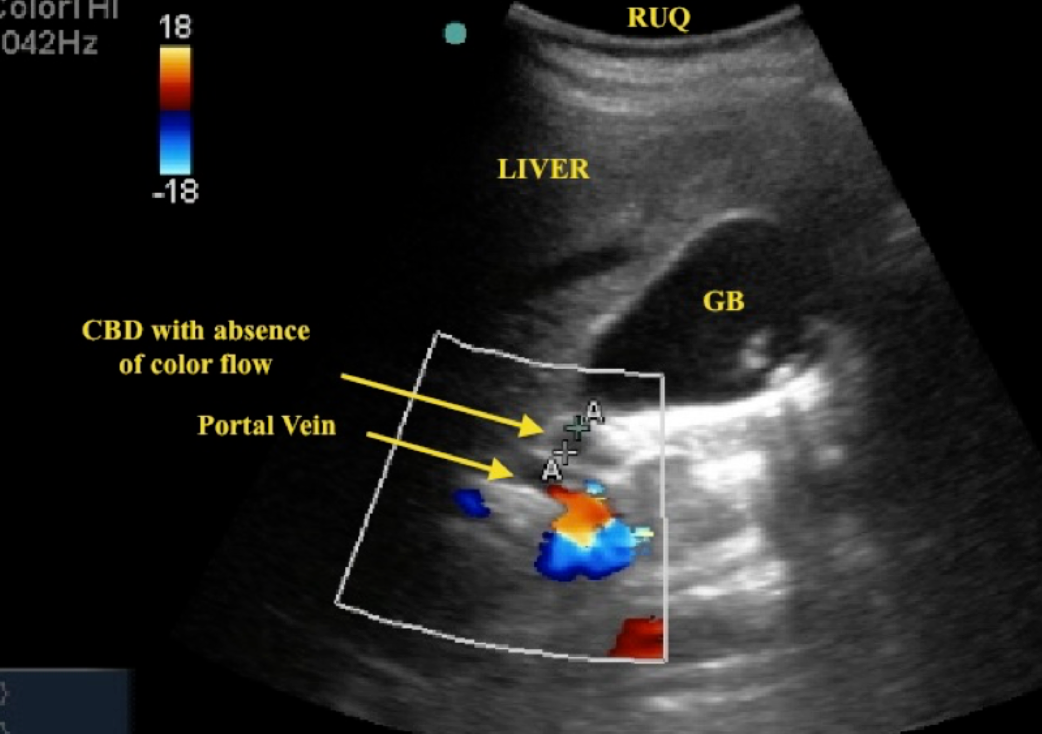
Dilatation of the intra- and extrahepatic biliary system can be identified at ultrasound, CT and MRI. #Z ***Ultrasound is usually the first test to be performed. ***
Dilated intrahepatic biliary ducts are seen at Ultrasound as serpentine structures paralleling the portal veins, a finding known as the ‘double channel sign’. Z
The common bile duct lies just in front of the portal vein and is dilated when more than 7 mm in diameter.
 Dilated biliary ducts. - obstruction of biliary
(a) Longitudinal ultrasound scan showing a dilated common bile duct (CBD) measuring 11 mm in diameter lying in front of the portal vein (PV). Normally the duct is much smaller than the accompanying vein. A dilated intrahepatic duct is noted.
Dilated biliary ducts. - obstruction of biliary
(a) Longitudinal ultrasound scan showing a dilated common bile duct (CBD) measuring 11 mm in diameter lying in front of the portal vein (PV). Normally the duct is much smaller than the accompanying vein. A dilated intrahepatic duct is noted.
(b) CT scan showing dilated intrahepatic ducts (arrows) in the liver.
MRCP study - stone in GB z
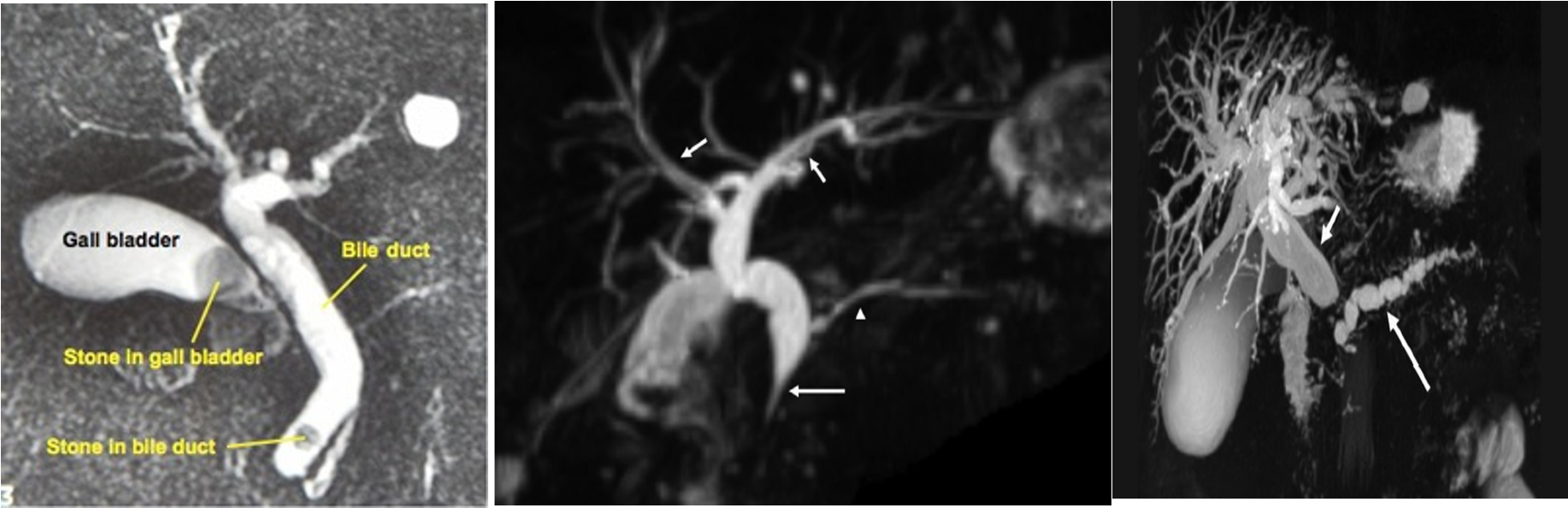 Double duct sign and stricture at the lower end of CBD strongly suggest carcinoma of pancreas
Double duct sign and stricture at the lower end of CBD strongly suggest carcinoma of pancreas
-
Note: Double duct sign Z shows that CBD and PD are both dilated
-
The width of a normal pancreatic duct is 3–4 mm Z
ERCP - CBD Stone
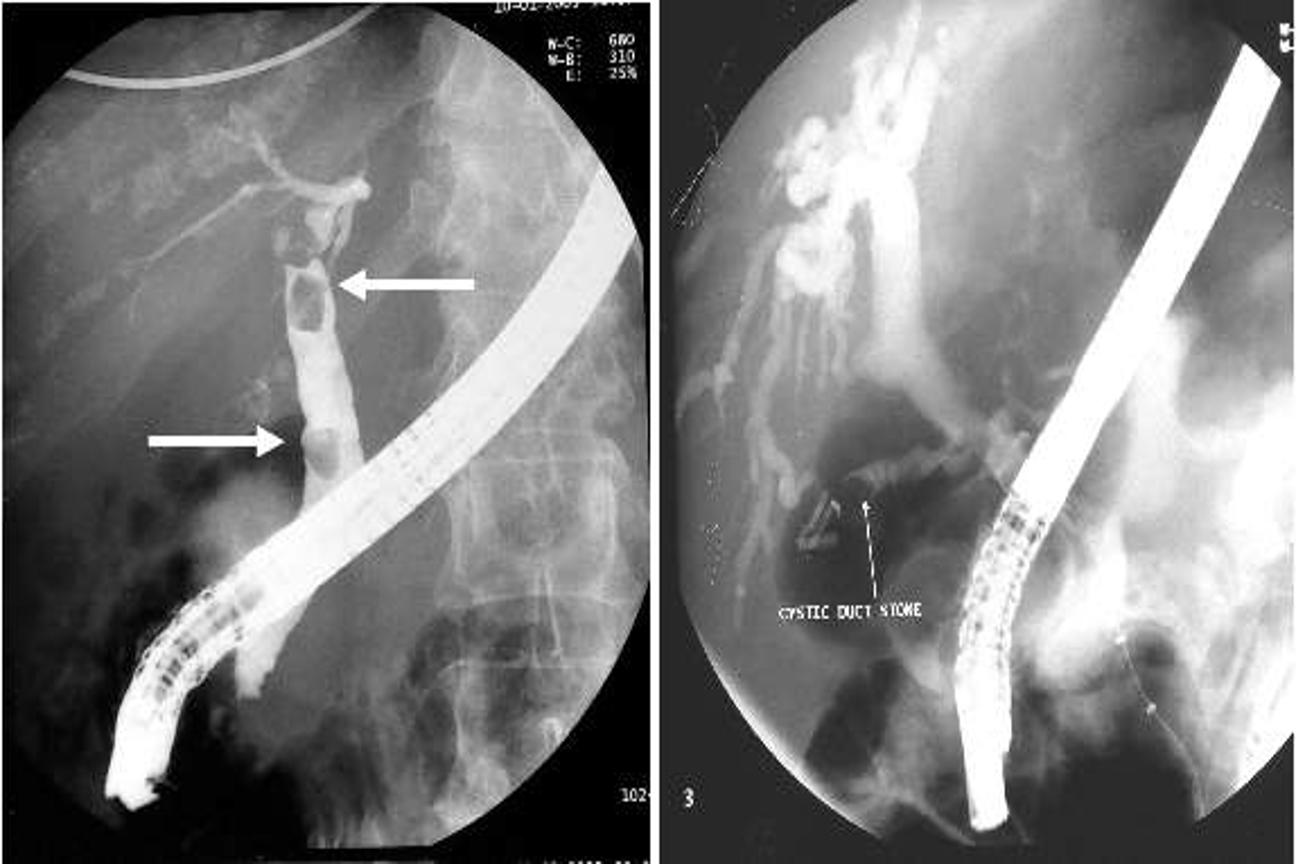
- Sign of filling defect