WIPER
Exposure | position | privacy | Ask for vitals
- W ash hands (before and after)
- I ntroduce yourself to the patient and seek his or her consent from both parties
- P osition the patient correctly.
- E xpose the patient as needed (e.g. ‘Please take off your shirt for me now, if that is all right’)
- R ight side of the bed
- Vital signs / Growth parameters
Introduce yourself to the parents and the child, including your name and role.
Confirm the child’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language: “Today I’d like to perform an examination of your child’s abdomen, which will involve first observing your child, then gently feeling their tummy.”
Gain consent from the parents/carers and/or child before proceeding: “Are you happy for me to carry out the examination?”
usual presentation in GIT case organomegaly
General Appearance
ABCDEFG Well, lying comfortable in bed, connected to iv line, no dysmorphic features.
- Activity
- Alertness
- Abnormal position in the bed. Distressed or not
- Appropriate size regarding weight and height for his age, just by observation.
- Any specific medications or devices surrounding the patient.
- Any dysmorphic features.
General Examination
Now move to the right side of the patient: -Start peripheral from the hands to see for signs important for GI
HANDS
Inspect the hands for clinical signs relevant to the gastrointestinal system:
- Pallor: may suggest underlying anaemia (e.g. malignancy, gastrointestinal bleeding, malnutrition)
- Erythema
- Capillary Refill
- Peripheral oedema: associated with nephrotic syndrome (loss of albumin) and liver disease (reduced production of albumin).
Nail Signs
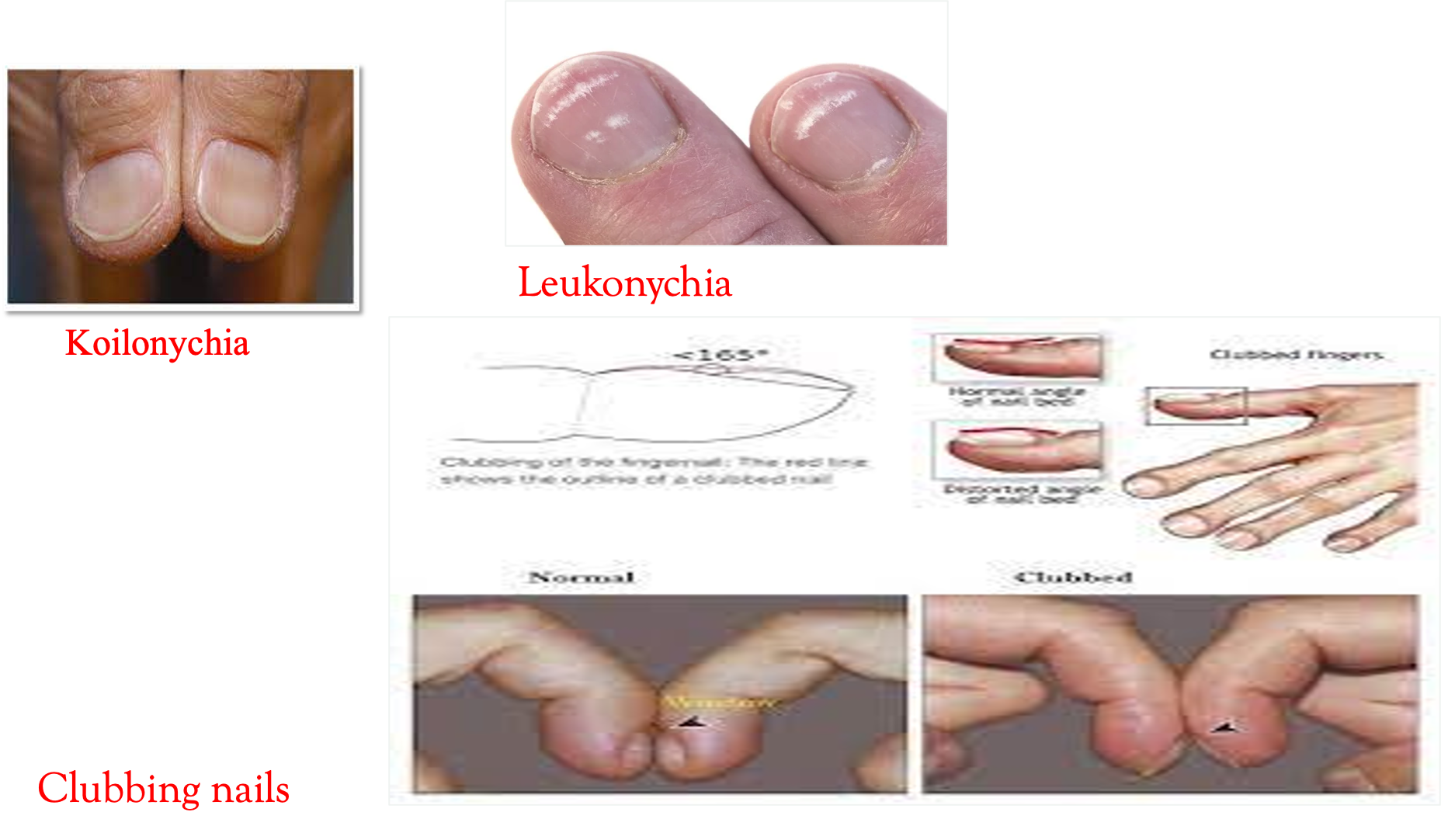
- Koilonychia: spoon-shaped nails, associated with iron deficiency anaemia (e.g. malabsorption in Crohn’s disease).
- Leukonychia: whitening of the nail bed, associated with hypoalbuminaemia (e.g. nephrotic syndrome, protein-losing enteropathy).
- Splinter Hemorrhages (liver diseases)
Finger Clubbing
Window test must be done Finger clubbing involves uniform soft tissue swelling of the terminal phalanx of a digit with subsequent loss of the normal angle between the nail and the nail bed. Finger clubbing is associated with several underlying diseases, e.g., cystic fibrosis and inflammatory bowel disease.
Palmar
- palmar erythema
- jaundice
- Flapping tremors
PULSE
Dont do pulse, just mention in GIT
Radial Pulse & Capillary Refill Palpate the child’s radial pulse, located at the radial side of the wrist, with the tips of your index and middle fingers aligned longitudinally over the course of the artery. Once you have located the radial pulse, assess the rate and rhythm. In babies, assess the femoral pulse instead.
ARM & AXILLA
- Deseferral injection pump, cannulation, etc.
- Puberty, acanthosis nigricans.

FACE & NECK
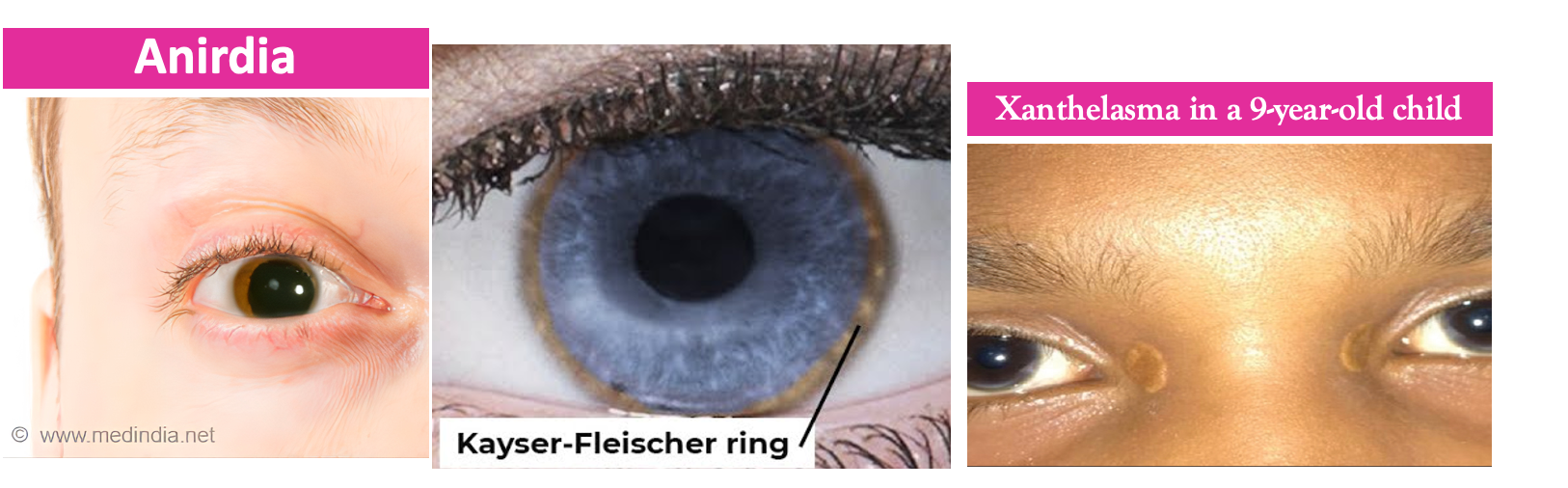
Face Observe the child’s facial complexion and features, including their eyes and mouth.
- Jaundice
- Pallor
- Periorbital edema
- teeth, tongue, mucosa
- Lips
- Pigmentations
- Angular stomatitis
- Excessive dryness
- Hygiene
- Ulceration
- Palate
Neck
-
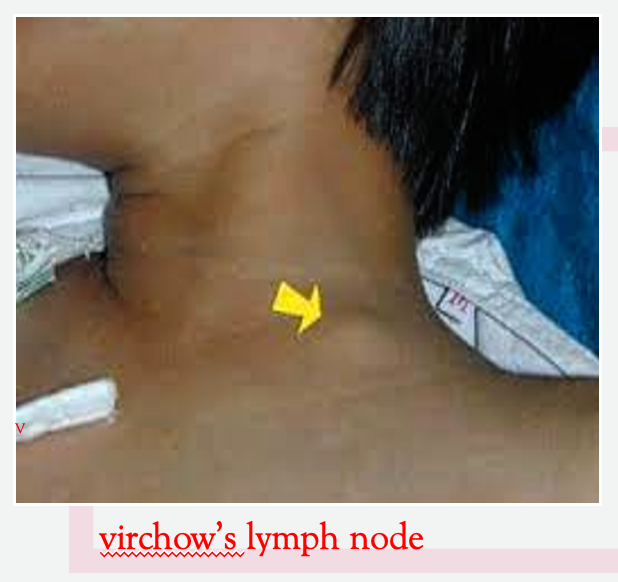
The left supraclavicular lymph node (known as Virchow’s node) can be one of the first clinical signs of metastatic intra-abdominal malignancy.
-
The right supraclavicular lymph node receives lymphatic drainage from the thorax and therefore lymphadenopathy in this region can be associated with metastatic oesophageal cancer (as well as malignancy from other thoracic viscera).
-
Palpate the supraclavicular fossa on each side, paying particular attention to Virchow’s node on the left for evidence of lymphadenopathy.
-
Acanthosis nigricans


Abdomen Focused Examination
EXPOSURE: Nipple to midthigh - assure privacy
Inspection
before starting say ideal position (supine) & exposure (mid nipple to mid thigh) - Go at end of the bed infront patient and mention the following
- Scars: there are many different types of abdominal scars that can provide clues as to the child’s past surgical history.
- Abdominal distension: can be caused by a wide range of pathology including constipation, Hirschsprung’s disease, ascites, organomegaly, and malignancy.
- Skin: pigmenations, colors
- Caput medusae/Vein diltation: engorged paraumbilical veins associated with portal hypertension (e.g. liver cirrhosis).
- Hernias - COUGH: observe for any protrusions through the abdominal wall (e.g. umbilical hernia, incisional hernia).
- Drains/tubes/stomas: gastrostomy, central venous catheter, ileostomy, and colostomy.
- Symmetry (distended or buldging)
- Umbilicus (everted?)
- Deformities
The abdomen is normally protuberant in toddlers and young children.
Palpation
Perform anticlockwise light palpation of the nine abdominal regions, whilst looking at the child’s face and assessing for rigidity, tenderness, guarding, and palpable masses. - deviating away at first from painful site, or area of concern.
No need to do deep palpation or quadrants percussion unless the superficial was positive
A- Superficial
- Tenderness & Superficial masses
Guarding is suggestive of peritonitis and indicates the need for urgent surgical review.
mention no tenderness or no masses if there were no findings
B- Deep
-
Tenderness & Superficial masses
-
Organomegaly (palpation / percussion for spleen; right illiac to left hypochondrium and liver; right illiac to right hypochondrium)
-
Kidney bi manual palpation/ballotment -(left hand below flanks, right palpating directly on the abdomen)
-
Localized in appendicitis (RIF), hepatitis (RUQ), and pyelonephritis (flank).
-
Generalized in mesenteric adenitis and peritonitis.
if palpable say: palpable liver (normally in paediatric you can feel the liver 2-3 cm below costal margin) if you feel the liver you have to measure the liver span by percussion to know if it’s hepatomegaly or not, Never say hepatomegaly without checking the liver span first !!
Guarding: Pain on coughing, moving about/walking/bumps during a car journey suggests peritoneal irritation. A child walking, whilst being flexed forwards suggests psoas irritation (e.g. appendicitis).
Incorporating play may be used to elicit more subtle guarding:
- “Can you jump up and down?” – a child will not be able to jump on the spot if they have localized guarding.
- “Blow out your tummy as big as you can, then suck it in as far as you can” – this will elicit pain if there is peritoneal irritation.
Abnormal Masses:
- Wilm’s tumour typically presents as a renal mass which is sometimes visible and does NOT cross the midline.
- Neuroblastoma typically presents as an irregular firm mass which may cross the midline. The child is usually very unwell.
- Faecal masses are typically mobile, non-tender, indentable, and often located in the LIF.
- Intussusception typically presents with a palpable mass in the RUQ (most commonly) in the context of an acutely unwell child.
LIVER PALPATION AND PERCUSSION Palpate from the right iliac fossa just above. ASIS and locate the edge of the liver with the tips or sides of your fingers in wave form (ask the child to take deep breaths if appropriate) . The liver edge may be soft or firm and you will be unable to get above it. The edge will move with respiration. Measure in centimetres the extension of the liver edge below the costal margin in the mid-clavicular line. Percuss downwards from the right lung 2 ICS to exclude downward displacement due to lung hyperinflation (i.e. in bronchiolitis). Dullness to percussion can help delineate the upper and lower border. Record the span of the liver (in cm).
Tip: Young children may be more cooperative if you palpate first with their hand or by putting your hand on top of theirs.
Hepatomegaly is an enlargement of the liver beyond age-adjusted normal values. It can be due to intrinsic liver disease or associated with systemic diseases seen in infants and children.
Normal Liver Size:
- Depends on age, gender, and body size
- Average liver span is 4.5 to 5 cm (neonates), 6 to 6.5 cm (12-year-old girls), 7 to 8 cm (12-year-old boys), and up to 16 cm (adults).
| Age | Acceptable span (cm) |
|---|---|
| Pre term infants | 4-5 |
| Healthy term infants | 5-6.5 |
| 1-5 years | 6-7 |
| 5-10 years | 7-9 |
| 10-16 years | 8-10 |
Describe organomegaly if found Z
- Span
- Surface (is it regular or irregular)
- Consistency (liver is hard - firm - smooth)
- Tenderness ( painful or not)
- Pulsations
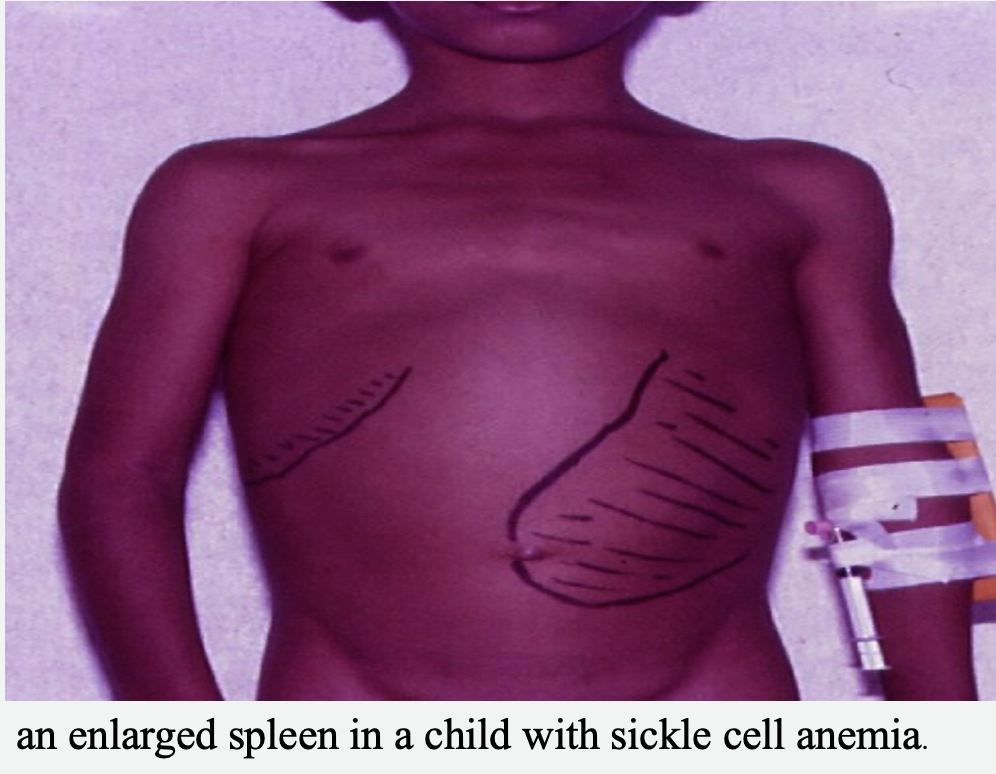
SPLENIC PALPATION AND PERCUSSION
- A palpable spleen is at least twice its normal size.
- Palpate from the right iliac fossa obliquely towards the left upper quadrant (ask the child to take deep breaths if appropriate). The edge is usually soft and you will be unable to get above it. The splenic notch is occasionally palpable if markedly enlarged. The spleen should move with respiration.
- Try palpating from Left iliac fossa to Left upper quadrant if there were not findings initially.
- Measure the degree of extension below the costal margin (in cm) in the mid-clavicular line.
- Percuss to delineate the lower border (splenic tissue will be dull to percussion).
KIDNEYS The kidneys are not usually palpable beyond the neonatal period unless they are enlarged or the abdominal muscles are hypotonic. Palpate the kidneys by balloting bi-manually in each hypochondrium. You can ‘get above them’ (unlike the spleen or liver) and tenderness implies inflammation.
Urinary bladder PALPATION palpate.... for megaly, tenderness
Causes of Kidney Enlargement:
- Unilaterally enlarged: hydronephrosis, cyst, tumour
- Bilaterally enlarged: hydronephrosis, kidney stones, polycystic kidneys
- portal hypertension
- epstien barr virus
- malaria
- glycogen storage disease
- Gushier syndrome???

Differentials depending on findings
Causes of hepatomegaly: There are several potential causes of hepatomegaly including:
- Infection: congenital, infectious mononucleosis, hepatitis, malaria
- Haematological: sickle cell anaemia, thalassaemia
- Malignancy: leukaemia, lymphoma, neuroblastoma, Wilm’s tumour, hepatoblastoma
- Metabolic: glycogen and lipid storage disorders, mucopolysaccharidoses
- Cardiovascular: heart failure
- Apparent hepatomegaly: chest hyper-expansion (e.g. bronchiolitis/asthma)
- hepatitis
- Abcess
- blood diseases (sickle thallasemia)
- leukemia / lymphoma
Causes of Kidney Enlargement:
- Unilaterally enlarged: hydronephrosis, cyst, tumour
- Bilaterally enlarged: hydronephrosis, kidney stones, polycystic kidneys
- portal hypertension
- epstien barr virus
- malaria
- glycogen storage disease
- Gushier syndrome???
Causes of splenomegaly
- There are several potential causes of splenomegaly including:
- Infection: infectious mononucleosis, malaria, leishmaniasis
- Haematological: haemolytic anaemia
- Malignancy: leukaemia, lymphoma
- Other: portal hypertension, Still’s disease
- Apparent splenomegaly: chest hyper-expansion (e.g. bronchiolitis/asthma)
Causes of Hepatosplenomegaly
- heridatiry spherocytosis (more so on spleen)
- Leukemia, Hemolytic anemia
- G6PD, SLE, Sarcoidosis
- CHF
To differentiate between splenomegaly and kidney enlargement:
- The spleen is movable with inspiration and expiration.
- The spleen is supra-peritoneal so dull in percussion.
- The kidney is infra-peritoneal so resonant in percussion(bowel above).
- Press your fingers just below the costal margin deeply if there is a window it is kidney enlargement
Percussion
A- upper and lower edges of liver (liver span)
B- Masses - resonant dull, liver;kidney;spleen if presents
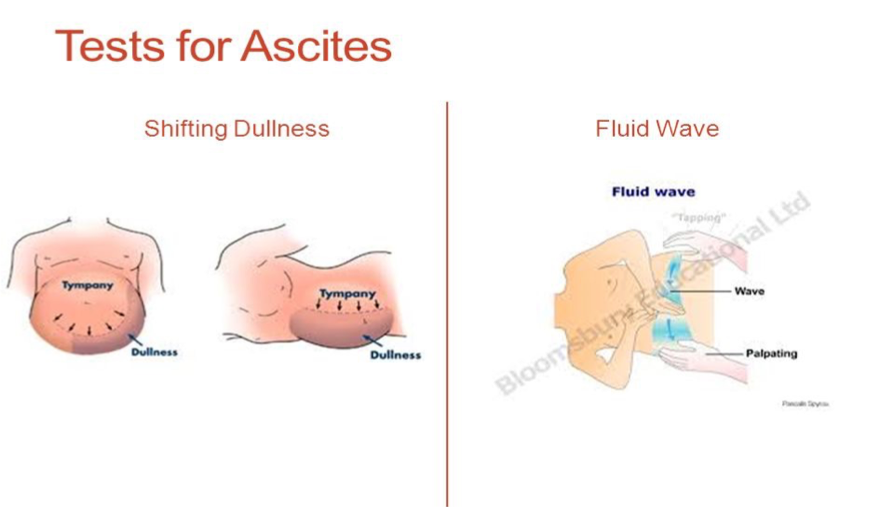
C- Shifting dullness
(below umbilicus, percuss to right or left depennding on presentation such as hepatomegaly, percuss right to the left) - wait 30 seconds afterwards from switching patient, then percuss again for dullness or resonance.
It is usually not possible to formally assess for shifting dullness in young children, due to issues with co-operation. However, in older children, it may be possible.
- Percuss from the umbilical region to the child’s left flank. If dullness is noted, this may suggest the presence of ascitic fluid in the flank.
- Whilst keeping your fingers over the area at which the percussion note became dull, ask the child to roll onto their right side (towards you for stability).
- Keep the child on their right side for 30 seconds and then repeat percussion over the same area.
- If ascites is present, the area that was previously dull should now be resonant (i.e. the dullness has shifted).
D- Fluid thrill
- (barrier in middle, then flick from opposite side to check for any wave forms)
do both tests
Causes of Ascites Ascites may be present in cirrhosis, hypoalbuminaemia, infection, or malignancy. The presence of shifting dullness is highly suggestive of ascites.
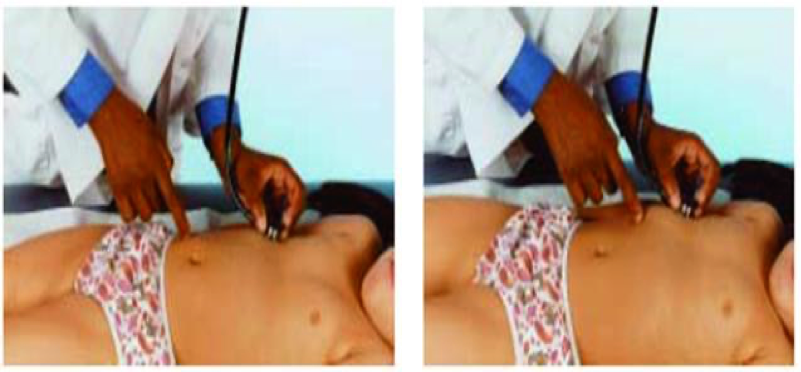
Auscultation
- auscultate all bowel areas.
- and renal bruits and other bruits
Closing exam
-
Examine the back (scoliosis, padding fat, meningocele, cafe spots, sacral edema, LNs)
-
Lower limb Exam (edema) against bony prominence
-
Urine dipstick (Bedside test) , stool analysis
-
Growth parameters (vitals, weight, height, head circumference)
-
Genital Exam
-
Rectal Exam / perrectal rarely done in pediatrics unless indicated (IBD, Crohn’s anal tags, anal proplapse, imperforate anus, Staining underwear - constipation, anemias, nephrotic, scrotal edemas) (herichpreng syndrome?)
Differential
Depends on the findings
Infectious:
Hematological:
C.T. Diseases:
Metabolic Diseases:
Immunodeficiencies:
Assessment
Labs:
Radiology:
Investigations/Approach
Depending on differentials
Virals - PCR
Electrophoresis, gene study - Sickle, Thallasemia
Autoimmune hemolytic anemia?
Tumours - biopsy
Treatment
Depends on diagnosis
thalassemia
- blood transfusion (iron overload - give chelating)
- bone marrow transplant
Sickle cell
- Hydroxyurea
- Gene therapy
- bone marrow transplantation
Notes
Bone Marrow Transplantation as a Treatment for SC, Thalassemia
Theory: How to Differentiate Between Hydrocele or Inguinal Hernia?
To differentiate between a hydrocele and an inguinal hernia:
-
Location:
- Hydrocele: Confined to the scrotum.
- Inguinal Hernia: Swelling extends from the groin to the scrotum.
-
Transillumination:
- Hydrocele: Transilluminates (fluid-filled).
- Inguinal Hernia: Does not transilluminate.
-
Reducibility:
- Hydrocele: Non-reducible.
- Inguinal Hernia: May be reducible.
-
Effect of Position:
- Hydrocele: Constant size.
- Inguinal Hernia: Increases with standing or straining.
-
Ultrasound: Confirms fluid in hydrocele or bowel in hernia.