ENT CASE SCENARIOS
اللهم يا معلّم موسى علّمني، ويا مفهم سليمان فهّمني، ويا مؤتي لقمان الحكمة وفصل الخطاب آتني الحكمة وفصل الخطاب اللهم اجعل ألستنا عامرة بذكرك، وقلوبنا بخشيتك، وأسرارنا بطاعتك، إنك على كل شيء قدير، حسبنا الله ونعم الوكيل
if there are any correction, changes, or addition in your notes please send me message dr.alkharji@proton.me
Updates through https://medatlax.com/Clinical/Level-10/ENT/CL-ENT/ENT-cs/ENT-Cs - will be highlighted yellow
Compiled from Alaa Alherz, Faisal Alkharji, Fatimah Lajami, Lamya Alotaibi, Sara Alramadhan, Yara Alzahrani, Zainab Bohulaigah. 2020-2025
Cases
Case 1
Presentation
- 55 Y.O male, smoker with a history of hoarseness from 6 months.
- Endoscopic examination shows: Reinke’s edema.
Management
- Most important step:
- Stop predisposing factors (smoking, alcohol).
- Long term risk:
- Malignant transformation.
Case 2
Presentation
- 8 months old baby post open heart surgery at age of 1 month.
- Kept intubated for 1 week post-operative.
- Presented to the clinic with stridor.
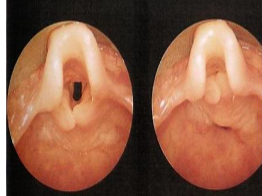
- Endoscope finding: Subglottic stenosis.
Diagnosis
- Grade:
- III
- Type of stridor:
- Biphasic stridor.

Case 3
Presentation
- Newborn with cyanosis improved with crying.
- Size 6 French catheter inserted and couldn’t be advanced more than 5cm.
Diagnosis
- Most possible diagnosis:
- Bilateral choanal atresia.
Management
- Emergency treatment:
- Insertion of oral tube.
- Confirmation:
- CT scan.
- Definitive management:
- Surgical treatment (transnasal or transpalatal choanal atresia repair).

Case 4
Presentation
- 6 Y.O child present with fever, stridor, and odynophagia.
- Examination: bulge in the posterior pharyngeal wall.
- Lateral x-ray shows: Retropharyngeal abscess.
Management
- Best management:
- Transoral incision and drainage.
- IV antibiotics.


Case 5
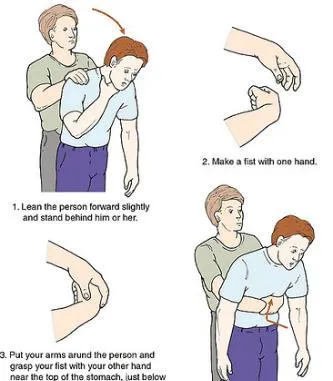
Maneuver
- Name:
- Heimlich maneuver.
- When to use:
- In case of choking.
Case 6
Presentation
- 2 months old baby with history of weak crying since birth and stridor.
- No choking.
- Scope shows: Glottic web.
Management
- Severe cases:
- Tracheostomy.
- Laser excisions & stent.
- Most likely type of stridor:
- Inspiratory stridor.

Case 7
Presentation
- 25 Y.O male with 3 days history of odynophagia and fever.
- Previous ER visit for odynophagia and fever, prescribed oral antibiotics for 7 days but stopped after 3 days.
- Oral examination showed: Right peritonsillar abscess.
Management
- Definitive management:
- Incision & Drainage.
- IV antibiotics.

Case 8
Presentation
- 6 months old child with 3 months history of inspiratory stridor that increases with exertion and feeding and improves in prone position.
- No choking or cyanosis.
- Electroscope finding during inspiration or expiration:
- Laryngomalcia.
Management
- Mild cases:
- Observation.
- Severe cases:
- Surgical (supraglottoplasty, tracheostomy).

Thyroid and Salivary Gland Cases
Case 1
Presentation
- 27 Y.O patient with lower lump since 3 months, increasing in size.
- Physical examination: 3cm right thyroid mass, not tender, no lymph node in the neck.
Investigation
- Lab: TSH, T3, T4.
- U/S.
- FNA: Papillary thyroid.
Management
- Treatment:
- Thyroidectomy +- neck dissection +- radioactive iodine.
- Follow up:
- HX, examination.
- Radioactive iodine.
- Tumor marker: Thyroglobulin or Anti-thyroglobulin antibody.
Medullary Thyroid Carcinoma
- Origin:
- Perifollicular C cell.
- Treatment:
- Thyroidectomy + central dissection.
- Radioactive iodine:
- Not included as it is not sensitive to it.
- Tumor marker:
- Calcitonin, CEA.
- Poor prognosis:
- Anaplastic thyroid carcinoma.
Case 2
Presentation
- Dysphagia, can’t eat, can’t drink, tremor, progressive severe pain.
- Examination: bi submandibular swelling, very tender.
- Bilateral wharton’s duct opening shows pus in the right side if squeezing it.
Diagnosis
- Most common diagnosis:
- Submandibular stone.
Imaging
- Stones:
- radiopaque.
- Submandibular & calcification.
Management
- Massage.
- Analgesic, antibiotic.
- Saliva stimulation.
- Oral hygiene.
Case 3
Presentation
- 86.5 Y.O female with lower lump below the jaw 3-4 days, fever.
- Parotid mass since 3 months.
- Lab: high WBC’s.
- CT scan with contrast: 3cm solid mass in the right superficial parotid, no palpable lymph nodes.
Investigation
- FNA: Pleomorphic adenoma.
Management
- Treatment:
- Parotidectomy.
- Neck dissection:
- No, benign tumor.
Mucoepidermoid Carcinoma
- high grade mucoepidermoid carcinoma.
- Management:
- Parotidectomy +- neck dissection +- radiotherapy.
Head and Neck Cancer Cases
Case 4
Presentation
- 87.5 Y.O patient with painful right side tongue mass.
- Increase in size of the lymph nodes in A1&A2, hemorrhage.
Investigation
- Biopsy:
- Squamous cell carcinoma.
Premalignant Lesions
- Leukoplakia.
- Erythroplasia.
- Highest risk:
- Erythroplasia.
HPV Subtypes
- Malignant:
- 16-18.
- Papillary hematosis:
- 6-11.
Further Investigation
- CT scan H/N & CT scan abdomen/pelvis.
Management
- Curative:
- Partial discectomy +- radiotherapy.
Case 5
Presentation
- Patient with nasopharyngeal cancer.
Management
- Early:
- radiation.
- Advance:
- radiation +- chemotherapy.
Case 6
Presentation
- Hypopharyngeal carcinoma post cricoid.
Management
- Early:
- surgical or radiation.
- Advance:
- surgical total layngo-pharyngectomy + bilateral neck dissection + reconstruction +- chemoradiotherapy.
Case 7
Moure’s Sign
- Definition:
- Absence of laryngeal click.
- Significance:
- Post-Cricoid Carcinoma.
Case 8
Laryngeal Cancer
- Most common site:
- Glottic then supraglottic then subglottic.
Case 9
Salivary Glands
- Parotid duct:
- Stensen’s duct.
- Parotid gland sis:
- Serous.
- Submandibular gland sis:
- Serous & Mucus.
- Sublingual gland sis:
- Mucosa.
- Submandibular stones:
- More common due to gravity and mucus secretion.
Case 10
Zenker’s Diverticulum
- Technique to see:
- Barium swallow.
- Treatment:
- Diverticulectomy.
Case 11
Thyroglossal Cyst
- Treatment:
- Sistrunk operation (excision of cyst, track and central part of hyoid bone).
- Hyoid bone removal:
- To prevent recurrence.
Sinus and Pediatric Cases
Case 1
Presentation
- 30 Y.O DM patient with bilateral nasal obstruction for 6 months, facial pain.
- Examination: bilateral nasal discharge + polyp.
Diagnosis
- Diagnosis:
- Chronic sinusitis.
Management
- Medical:
- steroids (nasal spray).
- Surgical:
- FESS to remove the polyps.
Investigation
- Radiological:
- CT scan without contrast.
- With contrast:
- if there is intracranial complications, vascular, abscess, tumor.
Sinus Drainage
- Maxillary sinus:
- Middle meatus.
- Sphenoid sinus:
- Superior meatus.
- Inferior meatus:
- Nasolacrimal duct.
Case 2
Presentation
- 2 months boy with stridor, no breathing or feeding difficulty, normal voice.
- Symptoms started by age of 2 weeks and become worse with crying & feeding, improve in prone position.
Diagnosis
- Diagnosis:
- Laryngomalcia.
Laryngoscope Findings
- Falling down of arytenoid or epiglottis inside larynx.
Surgery Indications
- Failure to thrive, recurrent URTI, respiratory distress, cyanosis.
Management
- Surgical:
- Epiglottoplasty.
- Symptoms resolution:
- Yes, spontaneously.
Case 3
Presentation
- 25 Y.O patient with recurrent episode of vertigo lasting few seconds.
- No tinnitus, no hearing loss, no ear discharge, no headache.
Diagnosis
- Diagnosis:
- BPPV. Benign Paroxysmal Positional Vertigo (BPPV)
Examination
- Clinical examination:
- Dix Hallpike maneuver.
Pathology
- Most common site:
- Posterior semicircular.
Management
- Treatment:
- Epley’s maneuver.
Differential Diagnosis
- BPPV vs Vestibular neuronitis:
- Duration.
Question 1
A 24-month-old child with right lung pneumonia, right-sided wheezes, and hyperinflation of the right lung. What is the most appropriate diagnosis?
- C- foreign body aspiration
Question 2
An 18-month-old child with choking and cyanosis while eating popcorn. Where will the foreign body be found most commonly?
- C-Right main bronchus
Question 3
A 62-year-old smoker male with harsh voice for 1 year and edematous vocal folds bilaterally. What is the most important measure in the management?
- D- avoid of the precipitating factor
Question 4
A 30-year-old female post-total thyroidectomy with changes in voice pitch and inability to make explosive sounds. Which nerve is injured?
- C- superior laryngeal nerve
Question 5
A 72-year-old male with dysphagia, halitosis, and regurgitation of undigested food. How can you confirm the diagnosis?
- B- Barium swallow
Question 6
A 72-year-old male with bilateral cellulitis of submandibular and sublingual spaces (Ludwig angina). What is the best treatment?
- A-tracheotomy ,external drainge and IV antibiotics
Question 7
A 2-year-old child with hoarseness and stridor for 2 months, with a history of condylomata lesion in the cervix. What is the most appropriate management?
- D- tracheostomy should be avoided as much as possible
Question 8
A 4-year-old boy suspected to have obstructive sleep apnea. When is the obstruction expected to be seen?
- B- during Rapid eye movement
Question 9
A 28-year-old teacher came to the voice clinic. Which of the following changes will be seen when elevating her voice?
- A- increase the amplitude of vocal fold vibration
Question 10
A 22-year-old patient came for electromyography to confirm the presence of abduction in the vocal folds. Where should the electrode be inserted?
- D- posterior cricoarytenoid
Question 11
A 12-month-old baby referred with Grade II subglottic stenosis. What does that mean?
- C- 51-70% obstruction of the subglottic area
Question 12
A 10-month-old baby with shortness of breath, fever, and barking cough. X-ray showed steeple sign. What is the diagnosis?
- B- Croup
Question 13
A 5-year-old child with fever, shortness of breath, extended neck, and drooling. Lateral neck x-ray showed thumb print sign. What is the diagnosis?
- A- Epiglottitis
Question 14
A 21-year-old male with fever, odynophagia, and hot potato voice. There is medialization of the right tonsil with deviation of uvula to the left. What is the most appropriate diagnosis?
- D- peritonsillar abscess
Question 15
A newborn with weak cry and shortness of breath, diagnosed with digeorge syndrome. Which of the following is highly suspected?
- C- laryngeal glottic web
Question 16
A 5-day-old full-term baby with stridor since birth. What is the diameter of the subglottic to consider a normal subglottic area?
- B- more than 4 mm
Question 17???
A newborn noticed to have stridor. Endoscopic examination showed bilateral vocal fold immobility (congenital). What is the next step?
- A- MRI brain
Question 18
A 6-month-old infant with stridor in supine position, improved on prone position. What is the most common diagnosis?
- D- laryngomalcia
Question 19
A newborn baby in distress with cyanosis that improves with crying. What is the initial emergency treatment?
- C- insertion of oral airway
Question 20
A 4-year-old child presented with nasal obstruction and snoring. What is the most common cause of snoring in children?
- C- adenoid hypertrophy
Question 21
A newborn baby immediately after birth developed cyanosis which improved with crying. What is the most appropriate diagnosis?
- C- bilateral choanal atresia
Question 22
A 30-year-old teacher with hoarseness and voice fatigue. Examination showed symmetrical bilateral round lesions over the vocal fold. What is the diagnosis?
- B-vocal fold nodules
Question 23
A 45-year-old male with tonsillitis managed with oral antibiotics, came back with fever, CN IX, X, and XI palsy and respiratory distress. What is the most appropriate diagnosis?
- C-Parapharyngeal abscess
Question 24
A 5-year-old child with fever, odynophagia, and torticollis. Lateral neck x-ray showed thickening of the retropharyngeal space. What is the best management?
- B-intra-oral drainage + IV antibiotics
Question 25
During adenotonsillectomy, a patient is found to have a bifid uvula. What is the next step?
- B-Examine for submucus cleft
others
Vocal Fold Lesions
- A teacher presented with hoarseness.
- Diagnosis:
- Vocal fold lesions secondary to vocal abuse and trauma.
- Management:
- Voice therapy (voice rest), surgical removal if no response.
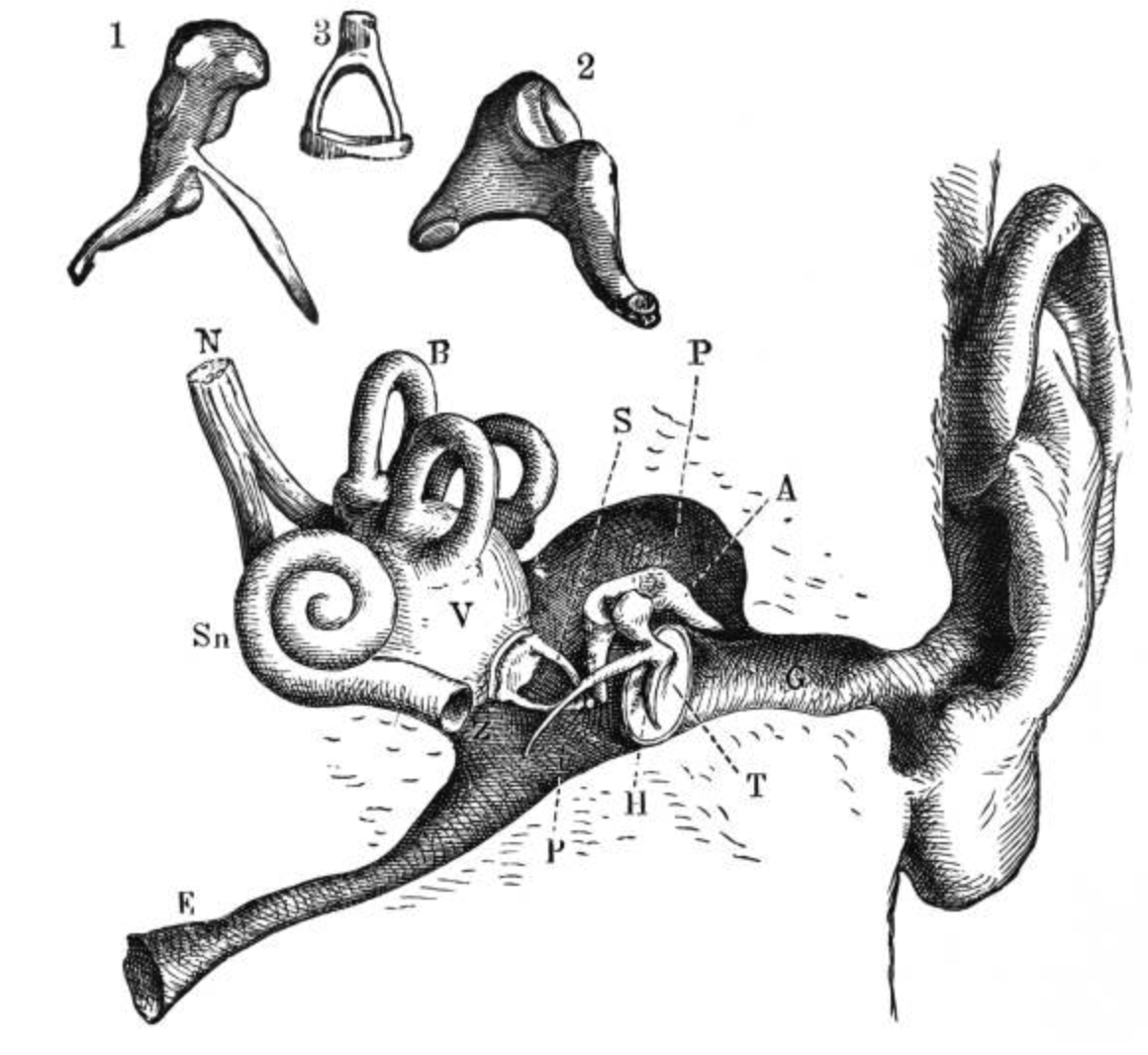
Cholesteatoma
- A 7-year-old with hearing loss, no history of ear discharge or infection.
- Diagnosis:
- Congenital cholesteatoma.
![[attachments/image34.png]]
- Treatment:
- Reconstructive surgery and mastoidectomy.
Fungal Sinusitis
- Diagnosis:
- Fungal sinusitis.
- Surgical Treatment:
- Endoscopic sinus surgery.
Others
-
Croup Management:
- Hydration.
- Airway management (steroids, epinephrine, cortisone).
-
Recurrent Croup:
- Rule out subglottic stenosis.
-
Bronchial Asthma with Unresponsive Symptoms:
- Rule out foreign body (FB) via bronchoscopy.
-
Infant Stridor Causes:
- Laryngomalacia.
- Inward collapse of arytenoids.
- Floppy epiglottis.
-
Management of Laryngomalacia:
- Mild cases: Observation.
- Moderate cases: Proton pump inhibitors (PPIs).
- Severe cases (failure to thrive, cyanotic spells, recurrent chest infections): Surgery.
-
Neonate with Bilateral Vocal Cord Paralysis:
- Perform MRI of the brain to exclude Arnold-Chiari malformation.
-
Nasal Trauma Management:
- No deformity or obstruction: Observation.
- Septal dislocation: Reduction.
- Deviated septum (after 3 weeks): Wait 6 months, then septoplasty.
- Deviated septum (after 1 week): Reduction under local/general anesthesia.
- Septal hematoma: Immediate I/D and silastic sheath.
- Nasal obstruction with synechiae (after 1 month): Surgery.
-
Foreign Body in Nose:
- Symptoms: Unilateral, thick nasal discharge, halitosis.
- Management: Suction, suspect foreign body.
-
Auricular Hematoma:
- Management: Drainage.
- Complication if delayed: Cauliflower ear.
-
Traumatic Tympanic Membrane Perforation:
- Management: Observation, no drops, no water, no suction.
-
Diver with Left Ear Pain and Conductive Hearing Loss:
- Management: Valsalva maneuver, decongestant (xylometazoline). If failed, myringotomy ± ventilation tube.
-
Facial Nerve Paralysis Post-Trauma:
- Grade 6 (complete paralysis): Immediate surgery, end-to-end anastomosis.
- Grade 3-4 (partial paralysis): Cortisone, wait for edema to subside.
-
Temporal Bone Fracture:
- Indicated by Battle sign behind the ear.
-
Neck Trauma Red Flags:
- Expanding hematoma, hemoptysis, subcutaneous emphysema, hoarseness, respiratory distress.
- Airway management in expanding hematoma: Tracheostomy.
Additional Cases
Case 4
Presentation
- 4 Y.O boy with acute onset of sore throat, neck lymphadenopathy, fever, no cough.
- Examination: large red tonsil, white follicles.
Diagnosis
- Diagnosis:
- Acute follicular tonsillitis.
- Most common organism:
- A&B hemolytic streptococcus aureus.
Management
- Medical treatment:
- Antibiotic.
- Tonsillectomy:
- If symptoms happened more than 7 times????
- Cause of bleeding after 5 days of tonsillectomy:
- Secondary hemorrhage due to infection.
Case 5
Presentation
- 50 Y.O patient with midline neck mass for 3 years, no dysphagia, no dyspnea.
- Mass is 4x4cm, moves with swallowing but with tongue protrusion, no retrosternal extension.
Investigation
- Radiological investigation:
- U/S.
- Next step after radiology:
- FNA.
Management
- Papillary thyroid carcinoma:
- Total thyroidectomy +- neck dissection +- radioactive iodine.
- Other types of thyroid cancer:
- Follicular, anaplastic, medullary.
- Indication of total thyroidectomy in benign thyroid nodule:
- Dysphagia, dyspnea, hoarseness, retrosternal extension, cosmetic.
Case 1
Presentation
- 30 year old diabetic presented with bilateral nasal obstruction for 6 months, facial pain and nasal discharge.
- Examination: nasal discharge and polyp.
Diagnosis
- Most likely diagnosis:
- Chronic sinusitis.
Management
- Medical:
- Nasal steroids.
- Surgical:
- FESS.
Investigation
- Radiological:
- CT w/o contrast.
Sinus Drainage
- Maxillary sinus:
- Middle meatus.
- Sphenoid sinus:
- Anterior ethmoid which drains into the middle meatus.
Case 2
Presentation
- Baby with stridor that improves in prone position.
- Examination: omega shaped epiglottis and closed arytenoid.
Diagnosis
- Diagnosis:
- Laryngomalacia.
- Type of stridor:
- Inspiratory.
Management
- Mild cases:
- Observation.
- Surgical intervention:
- Failure to thrive.
- Surgery name:
- Epiglottoplasty.
Case 3
Presentation
- 30 year old lady with postpartum hearing loss.
- Audiogram: left conductive hearing loss.
Diagnosis
- Type of hearing loss:
- Conductive hearing loss (left ear).
- Tympanometry:
- Type As (Reduced compliance).
- Rinne’s test:
- negative (BC louder than AC).
- Weber’s test:
- Louder towards the affected ear (Lateralization to the left).
- Most likely diagnosis:
- Otosclerosis.
- Surgery name:
- Stapedectomy.
Case 1
Presentation
- 22 years old male with right side yellow nasal discharge, periorbital swelling and fever for 3 days.
- History of flu 1 week ago.
- Vital sign: febrile 39.5.
- Right maxillary sinus tenderness with thick yellow nasal discharge in right nasal cavity.
- Right eye periorbital swelling with decrease visual acuity in the right eye.
Management
- Clinical setting:
- In patient setting with admission and IV antibiotics.
- Radiological investigation:
- Contrast-enhanced CT scan of the paranasal sinuses.
- Intracranial complications:
- The spread of the infection via valvless veins to his brain.
- Risk factor:
- Patient had recent upper respiratory tracts infection.
- Approach:
- All of the above (Radiological investigation, Taking details medical history, Full ENT examination including cranial nerves).
Case 2
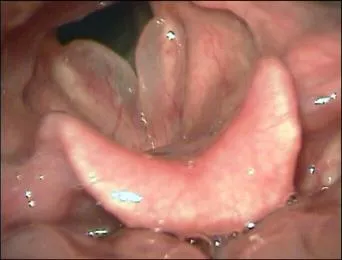
Presentation
- 6 -months -old child with 3 months history of stridor that increase with exertion and feeding and improve on prone position.
- No chocking or cyanosis.
- Fibrooptic scope done and the finding displayed in the picture during inspiration and expiration.
Diagnosis
- Gold standard tool for diagnosis:
- Fibre-Optic scope.
- Management of mild cases:
- Observation.
- Most likely diagnosis:
- Laryngomalacia.
- Type of stridor:
- Inspiratory stridor.
- Indication for surgical intervention:
- Failure to thrive.
Case 3
Presentation
- 70 years old male with sever right ear pain for 2 months, increasing in severity, associated with ear discharge for the same period.
- Hearing loss but no vertigo or tinnitus.
- Past medical history positive for lung cancer on chemotherapy.
- Used multiple eardrops and analgesia with no benefit.
- Since one week, he has drop face.
Examination
- Physical examination:
- Narrow external auditory canal with intact tympanic membrane.
- Most commonly affected cranial nerve:
- Facial.
- Best radiological investigation:
- bone scan
- Most likely diagnosis:
- Sskull base osteomyelitis
- Treatment of choice:
- iv antibiotic
Case 4
Presentation
- 50 years old presented midline neck swelling for 2 years that moves with swallowing but not with tongue protrusion.
Investigation
- Best first line radiological investigation:
- US neck.
- Most common thyroid cancer:
- Papillary thyroid cancer.
- Most likely origin of the mass:
- Thyroid gland.
- Next step if the radiology showed a nodule:
- Fine needle aspiration.
- Nerve most likely injured during total thyroidectomy:
- Recurrent laryngeal nerve.
Case 4
Presentation
- Trauma to the ear and swelling.
Diagnosis
-
Most likely diagnosis:
-
Auricular hematoma.
-
Treatment:
-
Incision and drainage, Aspiration, Pressure.
-
Complication:
-
Cauliflower ear (necrosis) – Perichondritis.
-
Difference between auricular hematoma and perichondritis:
-
Auricular hematoma:
-
Only a collection of blood.
-
Perichondritis:
-
An inflammation with fever, pus and pain.
-
Treatment of perichondritis: Antibiotics.
Case 5
Presentation
- Man presented with a midline swelling for 2 years that moves with swallowing but not with tongue protrusion.
Diagnosis
- Most likely diagnosis:
- Simple nodular goiter.
- Best radiological investigation:
- Ultrasound.
- Next step after the radiological finding of a nodule:
- FNA.
- Most common thyroid cancer:
- Papillary carcinoma.
- Thyroid cancer with the worst prognosis:
- Anaplastic carcinoma.
2025 Notes
Case 1: 70-Year-Old with Ear Pain
A 70-year-old patient presents with ear pain and has experienced yellowish discharge for 2 months without any odor or fever. Pain medication is ineffective, and there is decreased hearing on the right side, along with facial nerve changes suggesting compression. There are no enlarged lymph nodes, tenderness, or itching, but the patient experiences vertigo. The patient is diabetic and not well-controlled.
Differential Diagnosis:
- Otitis media or externa, differentiated by tympanic membrane involvement.
- Given the duration of more than 3 weeks, the condition is chronic. Chronic otitis media typically lacks pain.
- Most likely diagnosis: Malignant otitis externa (lasting >2 months), characterized by narrowing, redness, and discharge.
Investigations:
- CT scan, MRI, culture, ESR, CRP.
Management:
- Suction
- 6-week course of IV antibiotics targeting Pseudomonas.
Case 2: 30-Year-Old Swimmer with Ear Discharge
A 30-year-old swimmer presents with a one-week history of yellowish ear discharge, itching, and hearing loss, but no vertigo.
Most Likely Diagnosis:
- Fungal infection, as the discharge is acute and painless.
Examination:
- Narrowing of the external canal with black heading.
Treatment:
- Suction
- Topical antifungal medication.
Case 3: Ear Pain and Discharge
A patient presents with ear pain, discharge, and hearing loss for one week.
Examination:
- Intact tympanic membrane
- Presence of ulcers, with a history of diabetes.
Treatment:
- Acyclovir
Case 4: Recurrent Ear Discharge in a 3-Year-Old Boy
A 3-year-old boy presents with recurrent ear discharge, ear pain, fever, severe headache, hearing loss, limited movement, and decreased feeding.
Diagnosis:
- Consider lumbar puncture if not contraindicated; otherwise, rule out with a CT scan.
Treatment:
- Antibiotics based on culture sensitivity
- Ventilation tube insertion.
Case scenario head and neck tumors
Patient presented right neck mass 20 years old how do you approach the patient.
Progressed from two months
not associated with pain hoarseness difficulty breathing, smelly mouth, fever, weightloss, epistaxis, smoking, medication, allergies, contacts, family
Differential cold abcess, lipoma, ln enlargement, carotid body tumour
Examine mass
Complete Head & neck + Scope
Cystic non tender at level sternocleidomastoid
branchial cyst
U/S investigation (pediatrics or thyroid), CT initially in adults
Midline mass
- Approach?
- history (1 week, suddenly, painful, redness, hotness, discharge)
- Exam (moves deligation, midline)
- Differential (Thyroglossal cyst)
Submandibular Mass
- pain on swallowing,
- scialothiasis most likely
Case scenario head and neck tumors
Patient presented right neck mass 20 years old how do you approach the patient.
Progressed from two months
not associated with pain hoarseness difficulty breathing, smelly mouth, fever, weightloss, epistaxis, smoking, medication, allergies, contacts, family
Differential cold abcess, lipoma, ln enlargement, carotid body tumour
Examine mass
Complete Head & neck + Scope
Cystic non tender at level sternocleidomastoid
branchial cyst
U/S investigation (pediatrics or thyroid), CT initially in adults
Midline mass
- Approach?
- history (1 week, suddenly, painful, redness, hotness, discharge)
- Exam (moves deligation, midline)
- Differential (Thyroglossal cyst)
Submandibular Mass
- pain on swallowing,
- scialothiasis most likely
Case scenario head and neck tumors
Patient presented right neck mass 20 years old how do you approach the patient.
Progressed from two months
not associated with pain hoarseness difficulty breathing, smelly mouth, fever, weightloss, epistaxis, smoking, medication, allergies, contacts, family
Differential cold abcess, lipoma, ln enlargement, carotid body tumour
Examine mass
Complete Head & neck + Scope
Cystic non tender at level sternocleidomastoid
branchial cyst
U/S investigation (pediatrics or thyroid), CT initially in adults
Midline mass
- Approach?
- history (1 week, suddenly, painful, redness, hotness, discharge)
- Exam (moves deligation, midline)
- Differential (Thyroglossal cyst)
Submandibular Mass
- pain on swallowing,
- scialothiasis most likely
Ear Conditions and Management
-
Congenital Cholesteatoma:
- Symptoms:
- Hearing loss (bilateral), no pain, no discharge, no fever.
- Examination:
- Normal external ear, white mass intact with the tympanic membrane.
- Treatment:
- Surgery (tympanomastoidectomy).
- Type of Hearing Loss:
- Conductive.
-
Serous Otitis Media:
- Examination:
- Air bubbles behind the tympanic membrane.
- Treatment:
- Observation; if no improvement, surgery (ventilation tube).
-
External Otitis Media:
- Symptoms:
- Ear pain, continuous discharge, unilateral, facial nerve palsy (in malignant cases), no fever, no headache. Granulation tissue and intact tympanic membrane on examination.
- Diagnosis:
- Based on intact tympanic membrane and discharge.
-
Malignant Otitis Externa:
- Symptoms:
- Pain more than one month, facial nerve palsy.
- Most Likely Organism:
- Pseudomonas.
- Investigations:
- Blood sugar, biopsy, CT, culture.
- Treatment:
- Long-term IV antibiotics (more than 6 months).
-
Acute Otitis Media with Complications:
- Symptoms:
- Ear pain, fever, decreased oral intake, vomiting, lethargy, pale and red bulging tympanic membrane.
- Diagnosis:
- Complication (meningitis) due to decreased oral intake and vomiting.
- Investigations:
- Lumbar puncture (LP).
- Management:
- IV antibiotics + myringotomy + ventilation tube.
-
Differentiation between External and Middle Otitis:
- Pain relieved after discharge indicates middle otitis.
- Pain remains the same indicates external otitis.
-
Management Based on Pus and Complications:
- Acute otitis media with pus inside without complication: IV antibiotic.
- Acute otitis media with pus inside with complication: IV antibiotic + myringotomy.
- Chronic otitis media with pus inside without complication: IV antibiotic.
- Chronic otitis media with pus inside with complication: IV antibiotic + tympanomastoidectomy.
Case Reviews
Congenital Subglottic Stenosis
- Presentation:
- 6-month-old baby, 5-month history of stridor, episodes of cyanosis, fibrotic scope findings.
- Diagnosis:
- Congenital subglottic stenosis.
- Gold Standard Diagnostic Tool:
- Bronchoscope or endoscopy.
- X-ray Sign:
- Steeple sign.
- Stridor Type:
- Biphasic.
- Surgical Treatment (Grade 3-4):
- LTR-CTR.
Parotid Mass
- Presentation:
- 20-year-old female, parotid mass appeared 8 months prior.
- Ideological Choice:
- CT with contrast.
- Next Step after CT:
- FNA.
- Benign Causes:
- Pleomorphic and Warthin’s tumor.
- Nerve Injured During Surgery:
- Facial nerve.
Temporal Bone Fracture
- Presentation:
- 25-year-old, motor car accident, trauma to the skull, right hearing loss, CT showing right transverse temporal bone fracture through the inner ear.
- Type of Hearing Loss:
- Sensorineural hearing loss.
- Tympanogram Type:
- Type A (normal middle ear).
- Rinne Test:
- Positive.
- Weber Test:
- Lateralizes to the left ear.
- Management:
- Hearing aid.
Fungal Sinusitis
- Presentation:
- 30-year-old, bilateral nasal obstruction, facial pain, nasal discharge, bilateral nasal discharge and polyps on examination, CT showing opacification in sinuses with heterogeneity.
- Diagnosis:
- Fungal sinusitis.
- Medical Treatment:
- Normal saline irrigation, corticosteroid nasal spray (no antifungals for chronic cases, only for acute).
- Surgical Treatment:
- FESS.
- Radiological Investigation:
- CT scan.
- Anterior Ethmoid Sinus Drainage:
- Middle meatus.
- Inferior Meatus Opening:
- Nasolacrimal duct.
- Middle Meatus Opening:
- Maxillary sinus, anterior ethmoid, frontal sinus.
- Superior Meatus Opening:
- Sphenoid sinus, posterior ethmoid.
Adenoid Hypertrophy
- Presentation:
- 4-year-old boy, snoring, mouth breathing, disturbed sleep, large adenoids on examination.
- Diagnosis:
- Adenoid hypertrophy.
- Anatomical Location of Adenoid:
- Nasopharynx.
- Surgical Treatment:
- Adenoidectomy.
- Relative Contraindication:
- Cleft palate.
- Complications:
- Bleeding, pharyngitis, otitis media, rhinosinusitis, recurrent upper respiratory tract infections, sleep apnea.
- Management:
- Investigation:
- X-ray lateral view, CT scan.
- Treatment:
- Penicillin, adenoidectomy, tonsilloadenoidectomy.