Perioperative Fluid Management

Total Body Water (TBW)
- Varies with age and gender.
- 60% of body weight in males.
- 50% of body weight in females.
- 80% of body weight in infants.
- Less in obese: fat contains little water.
Body Water Compartments
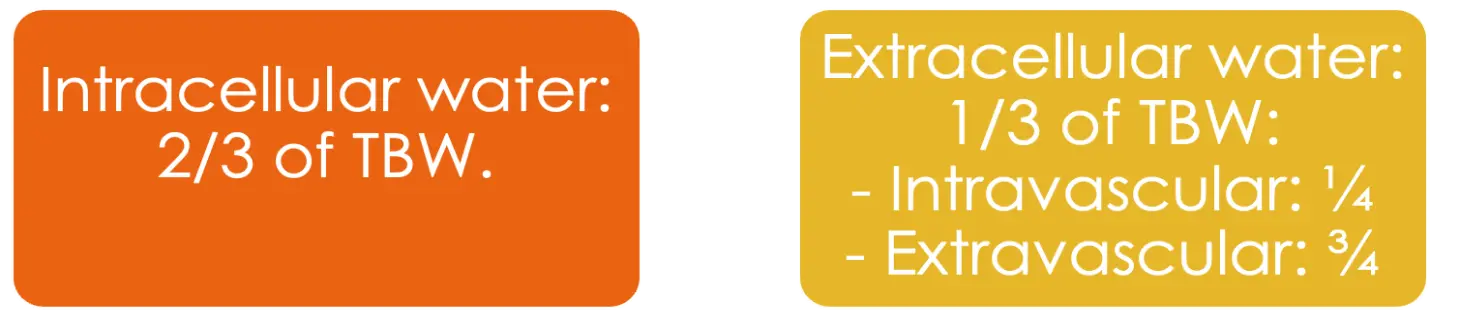 Intracellular water: 2/3 of TBW.
Extracellular water: 1/3 of TBW:
Intracellular water: 2/3 of TBW.
Extracellular water: 1/3 of TBW:
- Intravascular: _
- Extravascular: _
Electrolyte Contents
- Primary ECF cation is Na
- Very small contribution from K, Ca, Mg
- Primary ICF cation is K
- smaller contribution from Mg, Na
Fluid & Electrolyte Regulation
Volume regulation:
- Antidiuretic hormone.
- Renin/angiotensin/aldosterone system.
- Baroreceptors in carotid arteries and aorta.
- Stretch receptors in atrium and juxtaglomerular apparatus.
- Cortisol
Why It Is Important
- The final goal is delivery of adequate oxygen to the tissues
Factors affecting oxygen delivery include:
- Cardiac output. (stroke volume x heart rate)
- Hemoglobin concentration.
- Oxygen saturation.
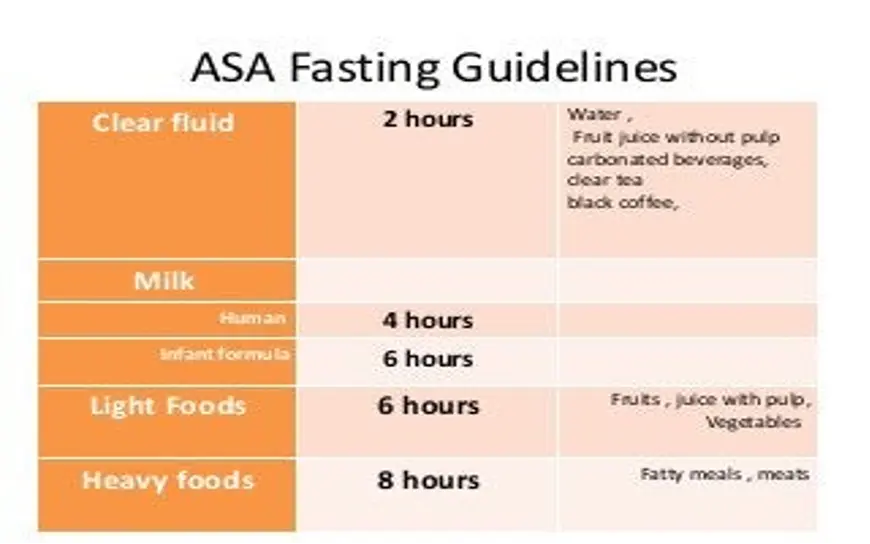
ASA Fasting Guidelines
- Clear liquid and water = 2 h
- Breast milk = 4 h
- Formula milk = 6 h
- Light meal = 6 h
- Heavy meal = 8 h
Perioperative Fluid Requirements
- Maintenance fluid requirements.
- Fluid deficits (NPO time and other deficits)
- Third space losses.
- Blood loss.
- Special additional losses (e.g. diarrhea)
1) Maintenanc˚e Fluid Requirements Z
-
Insensible losses such as evaporation of water from respiratory tract, sweat, feces, and urinary excretion.
-
Occurs continually.
-
4-2-1 Rule
- 4 ml/kg/hr for the first 10 kg of body weight.
- 2 ml/kg/hr for the second 10 kg of body weight.
- 1 ml/kg/hr for each subsequent kg of body weight.
2) Fluid Deficits
- NPO deficit = number of fasting hours x maintenance fluid requirement
- Bowel prep may result in up to one liter fluid loss.
- Measurable fluid losses. (e.g. Ostomy output, NGT suctioning, Vomits)
3) Third Space Losses
- Isotonic transfer of ECF from functional to non-functional body fluid compartments.
- Depends on location and duration of surgical procedure, amount of tissue trauma, temperature.
4) Replacing Third Space Losses
- Superficial surgical intervention: 1-2 ml/kg/hr
- Minimal surgical trauma: 3-4 ml/kg/hr (head and neck, hernia, knee)
- Moderate surgical trauma: 5-6 ml/kg/hr (hysterectomy, chest surgery)
- Severe surgical trauma: 8-10 ml/kg/hr (AA repair, nephrectomy)
5) Blood Loss
-
Every ONE ml of blood loss is replaced by THREE ml of crystalloid solution (WHY??)
-
When using PRBCs or colloids: replace blood loss as volume per volume.
Special Additional Losses
-
Ongoing fluid losses from other sites:
- Gastric drainage.
- Ostomy output.
- Others.
-
Replace as volume per volume using crystalloid solutions.
Example
- A 70 kg gentleman, going for open hemicolectomy at 08:00 am
- NPO after 22:00, received bowel prep
- Expected procedure duration is 3hrs
- Expected blood loss is 500 ml
What are his estimated intraoperative fluid requirements?
Example Calculation Z
-
Maintenance: Use rule 4x(10kg),2x(10kg),1x(restkg)
- 10kg x 4=40ml
- 10x2=20ml
- 50x1=50ml
- 110mls x 3hrs = 330mls=40+20+50
-
Fluid deficit: Rule hr/s maintenance x NPO hours
- NPO (110 x 10hrs = 1100mls)
- Bowel prep (1000ml)
- Total deficit = 2100mls
-
Third space losses: surgical trauma type x Kg x surgery duration 8ml/kg/hr
- (8ml x 70kg x 3hr) = 1680mls
- Superficial surgical intervention: 1-2 ml/kg/hr
- Minimal surgical trauma: 3-4 ml/kg/hr (head and neck, hernia, knee)
- Moderate surgical trauma: 5-6 ml/kg/hr (hysterectomy, chest surgery)
- Severe surgical trauma: 8-10 ml/kg/hr (AA repair, nephrectomy)
- (8ml x 70kg x 3hr) = 1680mls
-
Blood loss: 1:3 rule
- 500ml x 3 = 1500mls
-
Total: 330 (maintenance) + 2100 (fasting + prep) + 1680 (3rd space) + 1500 (blood loss) = 5610mls
Intravenous Fluids
- Conventional Crystalloids
- Colloids
- Blood/blood products and blood substitutes
Crystalloids
- Combination of water and electrolytes
- Isotonic salt solution
- Hypotonic salt solution
- Hypertonic salt solution

Crystalloids in Trauma: Advantages
- Balanced electrolyte solutions
- Buffering capacity (Lactate)
- Easy to administer
- No risk of adverse reactions
- No disturbance of hemostasis
- Promote diuresis
- Inexpensive
Colloids
-
Fluids containing molecules sufficiently large enough to prevent transfer across capillary membranes.
-
Solutions stay in the space into which they are infused (remain intravascular).
-
Examples:
- Hetastarch (Hespan)
- Albumin
Advantages
- Moderate volume
- Prolonged plasma volume support
- Minimal risk of tissue
- enhances microvascular flow
Disadvantages
- Adverse effect on Hemostasis, renal function
- Risk of volume overload
- Anaphylactic reaction
- Expensive
Blood Volume Management
- (up to 30% of blood volume can be treated with crystalloids)
- If blood loss exceeds 20% of blood volume and still there is ongoing bleeding, this will necessitate blood transfusion.
Blood Volume Formula
- Neonate - 90 ml/kg
- Infants and child - 80 ml/kg
- Adult male - 70 ml/kg
- Adult female - 60 ml/kg
Blood Transfusion
?WHY
- Improvement of oxygen transport
- Restoration of red cell mass
- Correction of bleeding caused by platelet dysfunction
- Correction of bleeding caused by factor deficiencies
When is Transfusion Necessary
- Transfusion Trigger: Hgb level at which transfusion should be given“
- Varies with patients and procedures
Oxygen Delivery
- Oxygen Delivery (DO2) is the oxygen that is delivered to the tissues
DO2 = COP x CaO2 - Cardiac Output (CO) = HR x SV
- Oxygen Content (CaO2)
- O2 saturation + PaO2(0.003)(Hgb x 1.39) -
Hgb is the main determinant of oxygen content in the blood
- O2 saturation + PaO2(0.003)(Hgb x 1.39) -
- Therefore: DO2 = HR x SV x CaO2
- If HR or SV are unable to compensate, Hgb is the major determinant factor in O2 delivery
- Healthy patients have excellent compensatory mechanisms and can tolerate Hgb levels of 7 gm/dL
- Compromised patients may require Hgb levels above 10 gm/dL
Blood Components
- Whole blood is separated by differential centrifugation
- Packed Red Blood Cells (pRBC’s)
- Platelets
- Fresh frozen Plasma, Contain all clotting factors
- Cryoprecipitate contains factor VIII and fibrinogen
- Factor VIII
- Albumin
- Others, antibody concentrate, Plasma protein fraction
Packed Red Blood Cells
- Unit = 250 ml. Hct. = 70-80%
- Unit pRBC’s raises Hgb 1 gm/dL
- Mixed with saline: LR has Calcium which may cause clotting if mixed
- with PRBC’s
RBC Transfusions: Administration
- Dose
- Usual dose of 10 cc/kg infused over 2-4 hours
- Maximum dose 15-20 cc/kg can be given to hemodynamically stable patient
- Procedure
- Filter use—routinely
- Monitoring
- Do NOT mix with medications
- Complications Z
- Rapid infusion may result in Pulmonary edema
- Transfusion Reaction

Transfusion Complications
- Hemolytic Reactions (acute or delayed) ►
- Febrile Reactions (FNHTR) ►
- Allergic Reactions ►
- TRALI ►
- Coagulopathy with Massive transfusions ►
- Infection ►
Signs
- Hypotension
- Fever, chills
- Dyspnea, skin flushing
- Substernal pain, Back/abdominal pain
- Oliguria, Dark urine, Pallor
Signs are easily masked by general anesthesia
- Free Hgb in plasma or urine
- Acute renal failure -
- Disseminated Intravascular Coagulation (DIC) -
Massive Blood Transfusion
Massive transfusion is generally defined as the need to transfuse one to two times the patient’s blood volume. For most adult patients, that is the equivalent of 10–20 units.