Alopecia Areata
- Sudden hair loss ( localized or generalized)
- Alopecia Areata affects up to 2%
- 75% : Self recovery, 2-6 m
Causes :
- 30%: +ve Family history
- autoimmune
Etiology
- Exact cause is still unknown.
- It is an autoimmune disease-
- Modified by genetic factors
Triggered by environmental factors-
- Trauma.
- Neurogenic inflammation.
- Infections agents.
ASSOCIATED DISEASE
Higher incidence of alopecia areata in patients of-
- Atopic dermatitis.
- Autoimmune disease –
- SLE
- Thyroiditis.
- Myasthenia gravis.
- Vitiligo.
- Lichen planus.
- Down syndrome.
Clinical features
-
Well demarcated
-
Exclamation point
-
Normal scalp
-
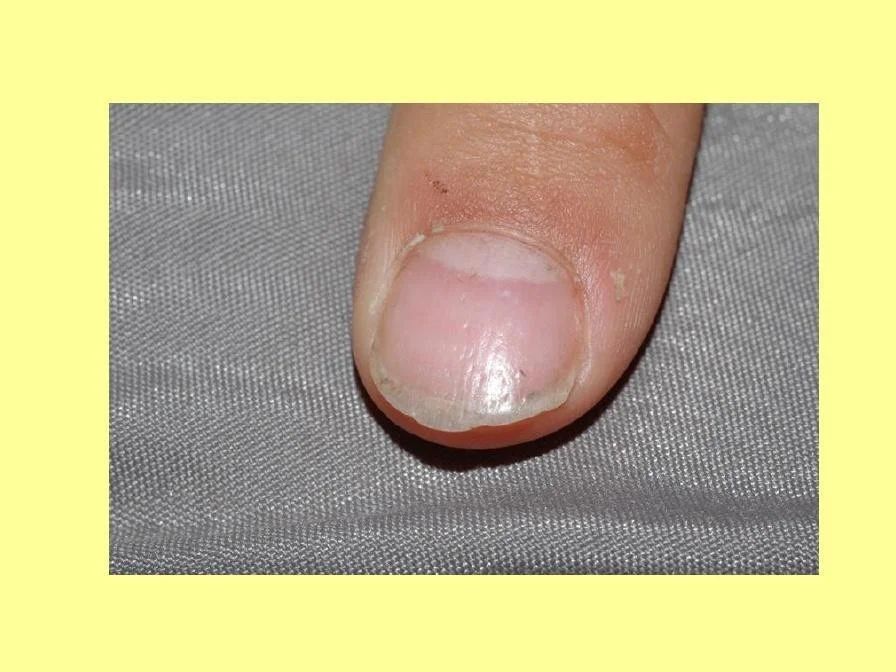
Nail: pitting, ridges
-
Rapid and complete loss of hair in one or several patches.
-
Site – Scalp, bearded area, eyebrows, eye lashes and less commonly other areas of body.
-
Size – Patches of 1-5 cm in diameter.
- “Exclamation point” hair- at the periphery of hair loss, there are broken hairs, whose distal ends are broader than the proximal end.



Types of alopecia areata
- Localized partial
- Localized extensive
- Alopecia ophiasis
- Alopecia totalis
- Alopecia universalis


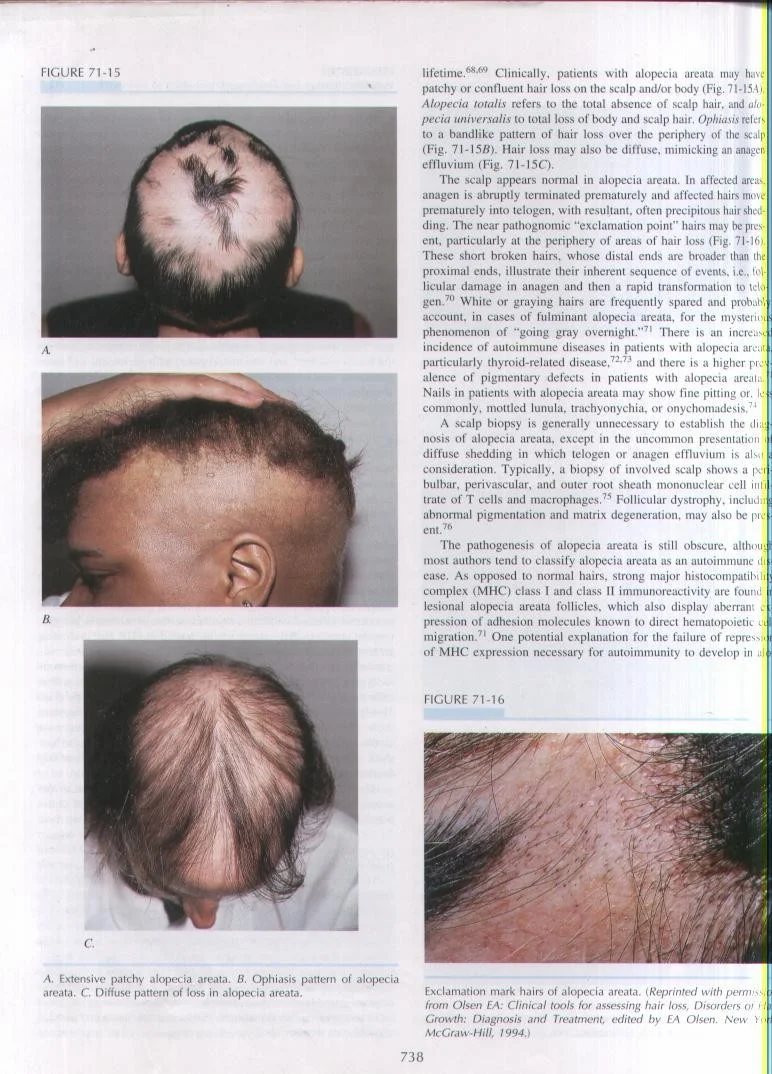
OPHI ASIS PATTERN OF ALOPECIA AREATA
ALOPECIA UNIVERSALIS
Loss of all the hair from all over the body including the scalp

Diagnosis
- Clinically
- H/E: sworm bees
DIFFERENTIAL DIAGNOSIS
- Tinea capitis.
- Trichotilomania.
- Secondary syphilis
Treatment
- Observation
- Intralesional Corticosteroids
- Skin Sensitizers
- Anthraline
- Diphencyclopropenone (DPCP)
- others
- Topical steroids
- Systemic Steroids
- Cytotoxic Rx
- Phototherapy
- Minoxidil
- Hair Transplant
⇒Spontaneous recovery is extremely common for patchy alopecia areata.
⇒For localized patchy alopecia areata- • Steroid- both local (intralesional and topical) and systemic (in short course).
Bad prognostic factors
- Young age
- Atopy
- Alopecia totalis, universalis, ophiasis
- Nail changes
Alopecia Areata (AA)

Alopecia Areata Features
- A condition characterized by either generalized or localized sudden hair loss from the scalp or other body sites
- Common: It affects up to 2% of the population.
- About 75% of patients show spontaneous self recovery within in 2-6 months.
- It can affect any age, but most cases are children or young adults
Causes (multifactorial):
- Psychological stress can be predisposing factor.
- Genetic background as 30% has +ve family history.
- Autoimmune (the strongest): as hair follicles attacked by immune cells
Clinical findings
- Well defined and demarcated alopecic patches.
- Exclamation point: characteristic around the hair follicle. Normally the hair is thick near the follicle and it becomes thinner as we go up, in this case the hair is thin near the follicle resembling an exclamation point → !)
- Normal scalp: no inflammation or scarring.
- Nail: pitting, ridges.

Types of Alopecia Areata:
1. Localized partial:
- – 1-2 patches.
- – complete recovery
- – most common type 2. Localized extensive:
- – 5-6 patches and could reach 10. 3. Alopecia ophiasis:
- – At the periphery of the scalp, for e.g. in the occipital region
- – Having this type of alopecia is a bad prognostic factor 4. Alopecia totalis: total hair loss in the scalp. 5. Alopecia universalis:
- – The whole body is affected (e.g. no eyelashes, actually NO hair at all, all over the body).
Bad prognostic factors:
- Young age.
- Atopy. (very important)
- Alopecia totalis, universalis, ophiasis.
- Nail changes: because it indicates that the effect of the disease is very bad.
- Loss of eyebrows and eyelashes
Diagnosis:
- Clinically: spot diagnosis, an area with no hair and the skin under it is normal.
- History and examination
Treatment
- Observation
- because in most cases the hair will re grow spontaneously.
- do it if the lesion small
- Intralesional corticosteroid:
- It’s the drug of choice in adults.
- We can’t give it to children b/c it’s painful. So, we give them topical corticosteroids coated under occlusion.
- Skin Sensitizers: Anthralin, Diphencyclopropenone (DPCP)
- Topical Steroids: under occlusion
- Systemic Steroids
- If the case was acute or an extensive case.
- We only give it for a short period of time
- Phototherapy: Narrow band - UVB - PUVA
- Minoxidil
