 E.g. Ductal carcinoma 80%, Fibroadenoma, Lymph nodes examination, supra infra calivcal lymph nodes & Axillae lymph nodes
E.g. Ductal carcinoma 80%, Fibroadenoma, Lymph nodes examination, supra infra calivcal lymph nodes & Axillae lymph nodes
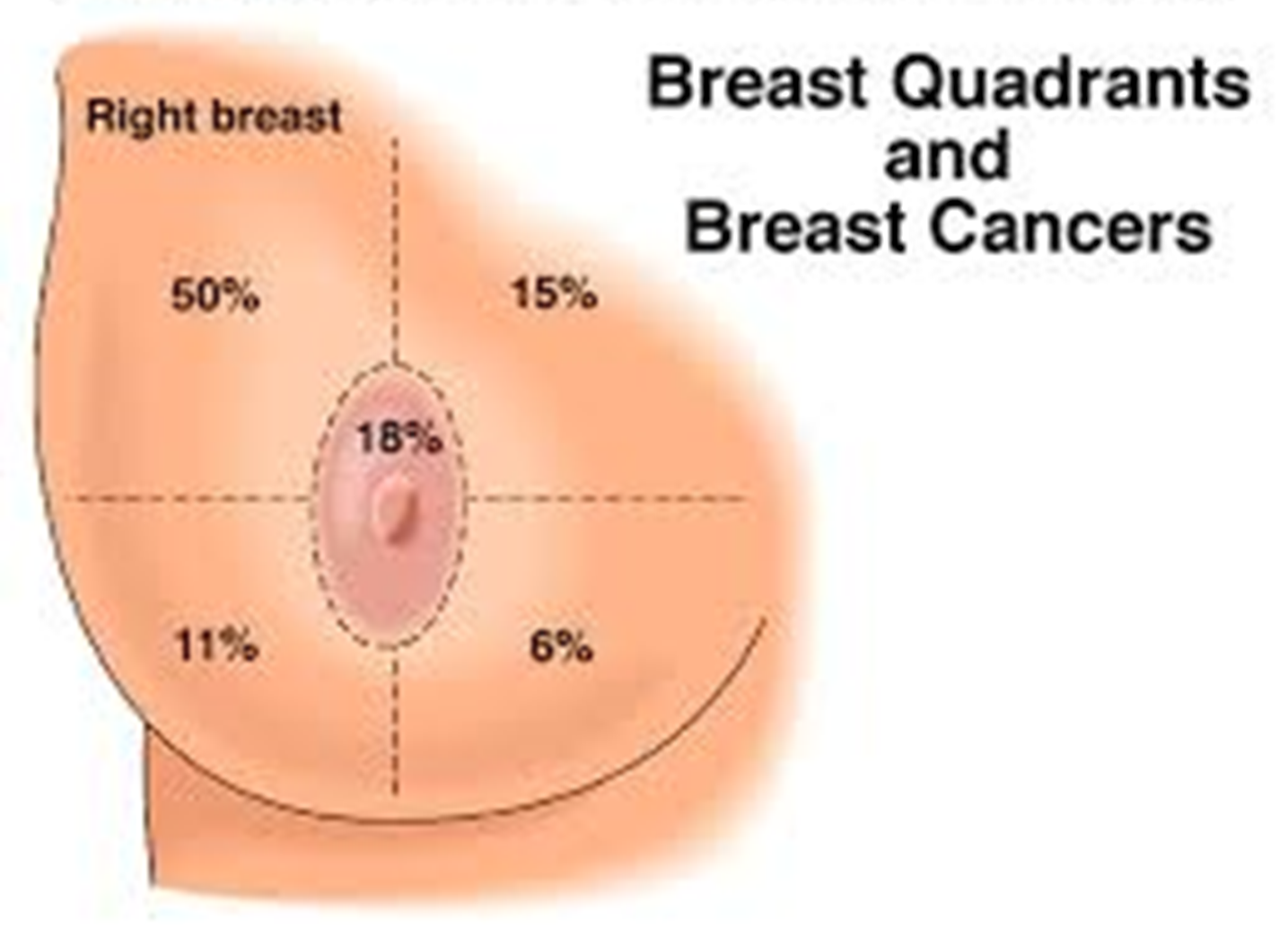
more common in upper quadruant of the breast.
 govenile hypertrophy cell - severe enlargement
in 3rd - Asymmetrical, alveoli extended, visible nodules, skin is shiny and thin, dilated vein,
4th image nipple is retracted; not inverted as its not inside yet
govenile hypertrophy cell - severe enlargement
in 3rd - Asymmetrical, alveoli extended, visible nodules, skin is shiny and thin, dilated vein,
4th image nipple is retracted; not inverted as its not inside yet
SURG
S. AHMED KHAN
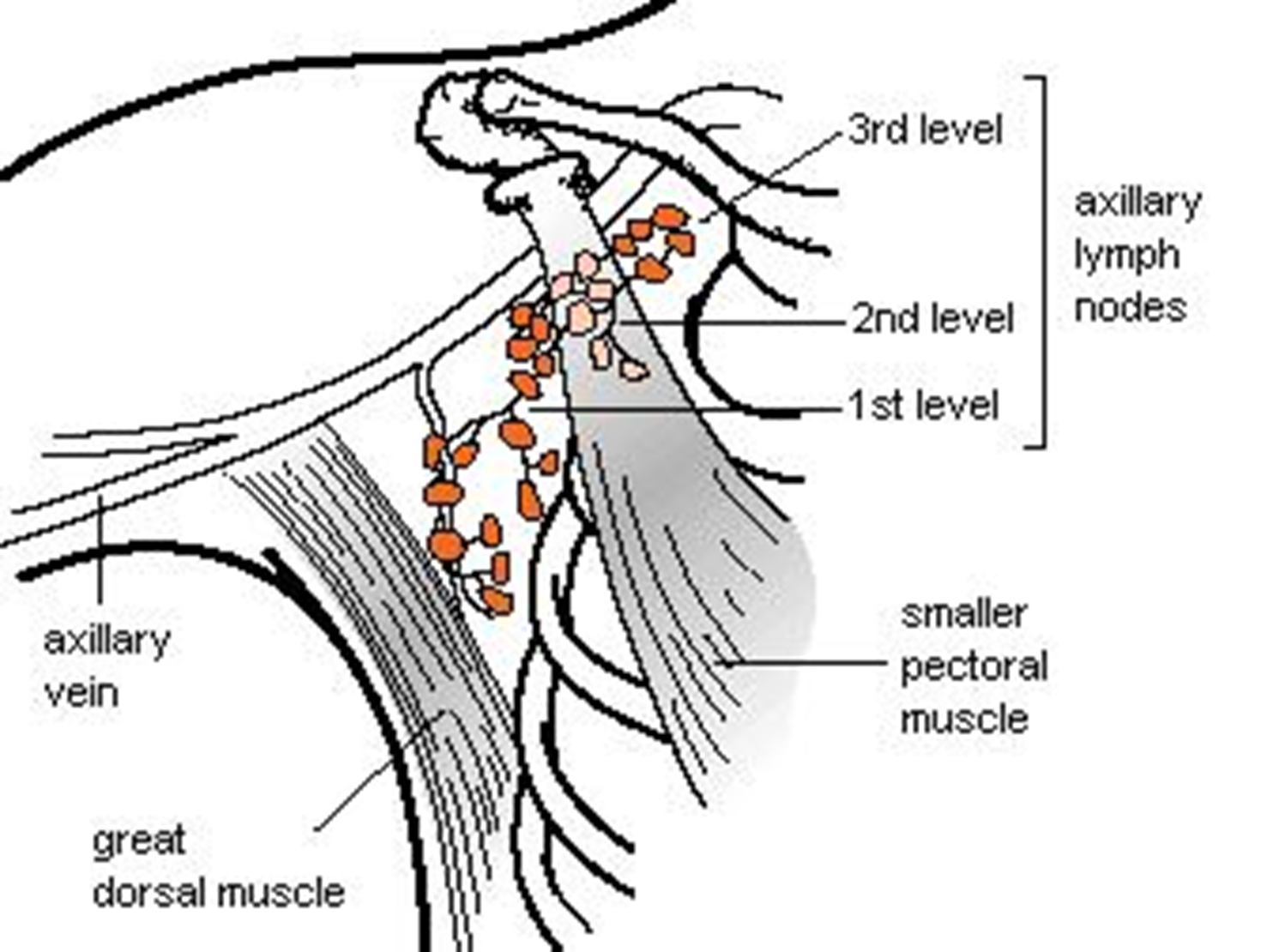
Axillary Lymph Nodes
- Level I: Lateral to the pectoralis minor muscle
- Level II: Posterior to the pectoralis minor muscle
- Level III: Medial to the pectoralis minor muscle
- Rotter’s nodes: Between the pectoralis major and the minor muscles
Changes in the Breast During Menstrual Cycle
- Increase in size in 2nd half of the cycle
- Slightly painful and tender during the later part of the menstrual cycle
- Pre-existing complaints may get worse
- Pre-existing lump may increase in size
History
Common complaints:
- Lump (most common)
- Pain/tenderness (Mastalgia)
- Change in breast size
- Change in the nipple
- Discharge from the nipple
Presentation of Breast Diseases
Painless lumps:
- Carcinoma
- Fibroadenoma
- Fat necrosis
- Cysts
Painful lumps:
- Fibroadenosis
- Abscess
Breast pain:
- Fibroadenosis (fibrocystic disease)
- Premenstrual pain
Changes in breast size:
- Giant fibroadenoma
- Phylloides tumor
- Benign hypertrophy (bilateral)
Changes in nipple:
- Carcinoma (retraction)
- Paget’s disease (ulceration)
Discharge from nipple:
- Red: Duct papilloma, carcinoma
- Yellow/Green: Fibrocystic disease, duct ectasia
- White/Milky: Galactorrhea

History
History taking follows the standard pattern
Detailed analysis of complaints
Important areas of history: menstrual, pregnancy, lactation (Breast feeding), family, previous breast problems
History of a Lump
- When noticed (duration)?
- How noticed?
- Any change in the lump since first noticed?
- Any change in the breast/nipple?
- Any associated symptom? Pain, discharge
- Any relationship with the menstrual cycle?
- Any history of trauma?
History of Pain
- Site
- Duration
- Onset and severity
- Relationship to the menstrual cycle (cyclical or non-cyclical)
- Aggravating factors
- Relieving factors
History of Discharge
- Duration
- Colour of discharge: blood (red), serum (brown, green, straw-coloured), pus, milky
- Spontaneous or on pressure
- Unilateral/bilateral
- Any change in the nipple
- Other accompanying symptoms (pain)
Past Medical/Surgical History
- Breast problem
- Mammogram
- Breast biopsy
- Exposure to radiation (face, chest) - risk factor
- Other medical/surgical history
- Obesity (BMI >25) - risk factor
Menstrual History
- Age of menarche
- Age at menopause
- early menarche (<12 years), late menopause (>55 years) - increases risk for carcinoma
- Last menstrual period
- Regularity of the menstrual cycle
- Breast changes during the menstrual cycle
History of Pregnancy
- Age at 1st pregnancy - younger age (<18) is protective
- >30 years - increased risk
- Number of pregnancies - protective
- Lactational history - protective
Medications
- Oral contraceptives - not a known risk
- Hormone replacement therapy - increased risk
- Other medications
Family History
- At least two generations
- Breast, gynecologic (ovarian), colon, prostate, gastric, or pancreatic cancer
- Their age at the diagnosis of these tumors
Clinical Examination
- Explain to your patient
- Patient’s permission
- Privacy
- Nurse’s presence
- Semi-recumbent position (45°), supine, sitting
- Expose the upper half of the patient, both breasts exposed
- Arms by the sides
Inspection of the Breast
- Stand in front of the patient
- 4 quadrants
- Symmetry & size of breasts (underlying lump)
- Any obvious mass or lump
- Skin changes - redness (infection, inflammatory carcinoma), edema (peau d’orange), dimpling, ulceration (carcinoma)
- Skin dimpling in the lower inner quadrant of the left breast associated with breast cancer
- Changes in the nipple/areola: raised level, retraction (carcinoma, duct ectasia), ulceration (Paget’s disease)
- Discharge from the nipple - spontaneous
- Raise arms above the head - inspect breasts & axillae and note any change
- Inspect the supraclavicular area
Palpation of the Breast
-
Semi-recumbent position
-
Ask for any painful area
-
Normal side first
-
Palpate with the palmar surface of the fingers for the presence of a lump
-
Lump characteristics: site, size, shape, surface, mobility, temperature, tenderness, texture, edge, attachment to skin or deep tissue For these characteristics - use the pulp of your fingers\
-
Site: More carcinoma develops in the upper outer quadrant
-
Size: Variable, Large mass - giant fibroadenoma, Phylloides tumor
-
Shape: Well defined - fibroadenoma, ill-defined - carcinoma
-
Mobility: Fibroadenoma freely mobile
-
Temperature: Raised in inflammation, inflammatory carcinoma
-
Tenderness: Inflammatory – abscess
-
Texture: Hard - carcinoma, firm - fibroadenoma, fluctuant - cyst
-
Attachment: Carcinoma, sometimes inflammatory lesions
-
Skin tethering - tumor infiltration of Cooper’s ligament pulling on the skin. Skin dimples when the tumor is moved to one side or arm raised above the head.
-
Skin fixation - when the tumor is directly fixed to the skin. The skin cannot be moved/pinched separately.
-
Muscle attachment - patient’s both hands resting on hips, test lump mobility before & after muscle contraction (ask the patient to press against hips).
Palpation of the Nipple
- Any retraction/ulceration
- Palpate for a mass underneath the affected nipple
- Nipple discharge - blood (red), serum (brown, green, straw-coloured), pus, milky
- Pathological discharge: Bloody, spontaneous, unilateral
- Discharge spontaneous or on pressure of a segment of the areola
- Any mass associated with the discharging duct
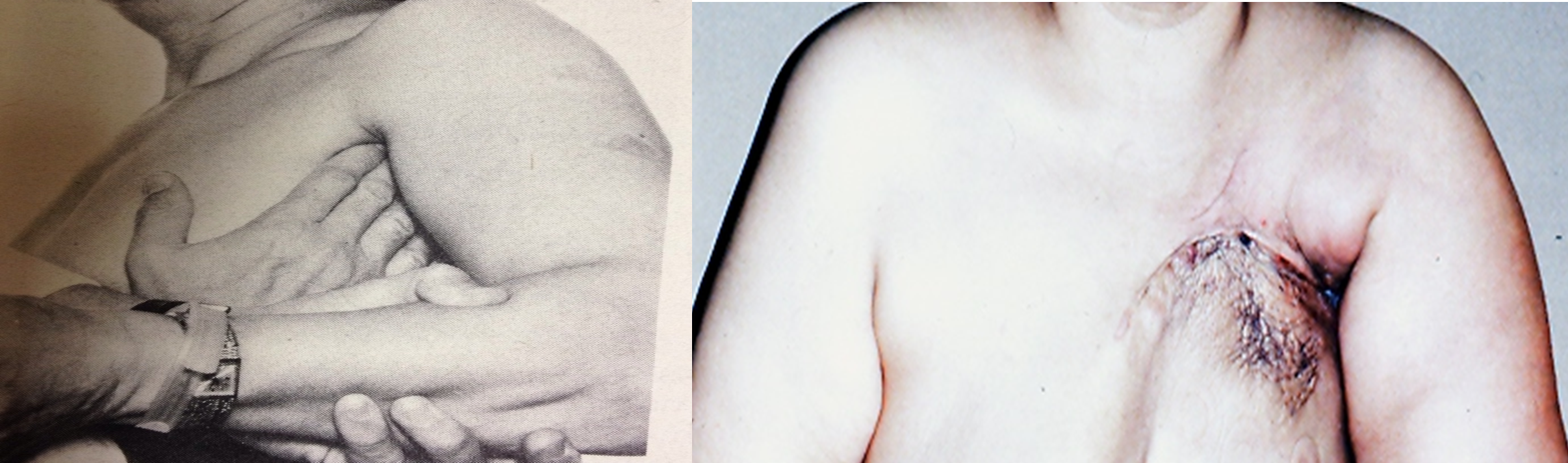
Palpation for the Lymph Nodes
-
Axilla, supraclavicular, infraclavicular lymph nodes
-
Patient sitting upright
-
Rt. Axilla: Hold the patient’s right elbow in your right hand. Palpate the axilla with your left hand. For the apex of the axilla, press the finger pulp upward and medially.
-
Lt. axilla - reverse
-
Palpate for supraclavicular, infraclavicular lymph nodes
-
Size, number, and fixation of lymph nodes
-
Examine the arm for any swelling
General Examination
Full general examination like any other patient
Concentrate on:
- Chest: any effusion
- Abdomen: hepatomegaly, ascites
- Spine: pain, tenderness, limitation of movement