RDS / “Hyaline Membrane Disease (HMD)”
The most common cause of respiratory failure in the premature newborn. Occurs almost exclusively in premature infants. The incidence and severity of respiratory distress syndrome are related inversely to the gestational age of the newborn infant.
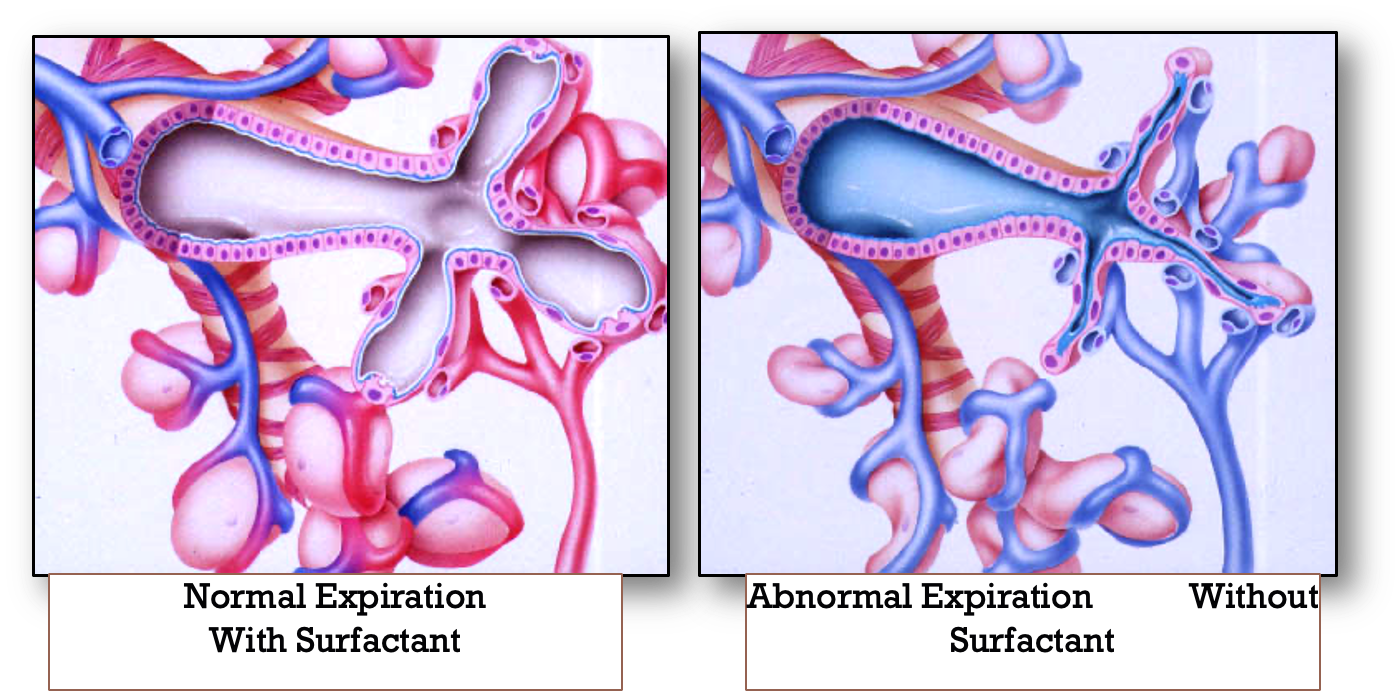
Respiratory distress syndrome develops in premature infants because of impaired surfactant synthesis and secretion leading to lung atelectasis. Surfactant is a mixture of lipids and proteins produced by type II pneumocytes in the lung epithelium. The absence of surfactant in the alveoli causes an increase in surface tension with consequent atelectasis at the end of expiration.
If not treated, such atelectasis leads to increased work of breathing, intrapulmonary shunting, ventilation-perfusion mismatch, hypoxia, and eventual respiratory failure. Subsequently, serum proteins that inhibit surfactant function leak into the alveoli and with other components form the hyaline membrane.
Surfactant Composition
Surfactant is stored in type II alveolar cells and composed of:
- Dipalmitoyl Phosphatidylcholine (Main component)
- Phosphatidylglycerol 90%
- Apoproteins & Cholesterol
Clinical Features
Signs and symptoms appear immediately after birth or within 6 hours of life, then reach a peak at 24-48 hours:
- Tachypnea usually >60 breaths per minute
- Expiratory grunting (from partial closure of glottis)
- Subcostal and intercostal retractions
- Cyanosis
- Nasal flaring
If the disease progresses, apnea and hypotension may occur, indicating the need for mechanical ventilation.
Diagnosis
-
Chest radiographs: Bilateral, diffuse, reticular granular, or ground glass appearances; air bronchograms (prominent air bronchograms represent aerated bronchioles superimposed on a background of collapsed alveoli); poor lung expansion.
-
Blood gas: Hypoxia; respiratory/metabolic acidosis; hypercarbia.
Radiographic Findings
1 or 2 = RDS
- Low lung volume
- Air bronchogram
- Diffuse fine atelectasis (ground glass appearance)
- Near-total atelectasis will show complete opacification of lungs (White Lung)

Antenatal Diagnosis/Prediction
Fetal lung test for lung maturity prediction:
- Lecithin/sphingomyelin ratio in amniotic fluid (lecithin is at twice the sphingomyelin)
- Elevated phosphatidylglycerol level in amniotic fluid
Complications
- Intraventricular hemorrhage/periventricular hemorrhage
- Patent Ductus Arteriosus (PDA)
- Pulmonary hemorrhage
- Pneumothorax and air leak
- Chronic Lung Disease (Bronchopulmonary Dysplasia, the lung is not dependent, 02 is required) كثير بالشميسي
- Removed —Retinopathy of prematurity----
Risk Factors
- Prematurity
- C-section
- Hypoxia, acidosis
- 2nd born twin
- Infant of diabetic mother
- Family history of RDS
- Antepartum hemorrhage
Treatment
- Admission to NICU
- Connect to oxygen (CPAP will open the alveoli)
- Correct hypoxemia and acidosis, reduce metabolic demands
- Chest X-ray
- Intravenous fluids
- Intratracheal Surfactant (2 doses 24 hours apart)
- Mechanical ventilation for severe cases
Prevention surfactant endotracheal
Antenatal steroids (betamethasone or dexamethasone) 24-34 WOG who are at risk of premature delivery will enhance lung maturation and rapid alveolisation