Endotracheal tube is: A flexible hollow tube designed to enter the trachea via the oropharynx or the nasopharynx, facilitate gas exchange, and protect the airway from aspiration
Definitive Airway is: A tube placed in the trachea with cuff inflated below the vocal cord.
Advantages of Intubation
- A cuffed endotracheal tube protects the airway from aspiration
- Access is gained to the tracheobronchial tree for the suctioning of secretions
- Ventilations via an endotracheal tube do not cause gastric distention
- Maintains a patent’s airway and assists in avoiding further obstruction (like in burns)
- Enables delivery of certain medications
Indications
- For supporting ventilation in patient with :-
- Upper airway obstruction
- Respiratory failure
- Loss of conciousness
-
For supporting ventilation during general anesthesia.
-
Patients at risk of pulmonary aspiration
- Massive hemoptysis
- Uncontrollable vomiting
-
Difficult mask ventilation
-
Anticipated airway obstruction (inhalation Burns).
-
Cardiac arrest
Contraindications
- Laryngeal disruption / Fracture
- DNAR (Do Not Attempt Resuscitation)
Conditions that associated with difficult Intubation
- Congenital anomalies ⇒ Down’s syndrome
- Infection in airway ⇒ Retropharyngeal abscess, Epiglottitis
- Tumor in oral cavity or larynx
- Enlarge thyroid gland ⇒ trachea shift to lateral or compressed tracheal lumen
- Maxillofacial ,cervical or laryngeal trauma
- Temperomandibular joint dysfunction
- Burn scar at face and neck
- Morbid obesity
Air way assessment Z
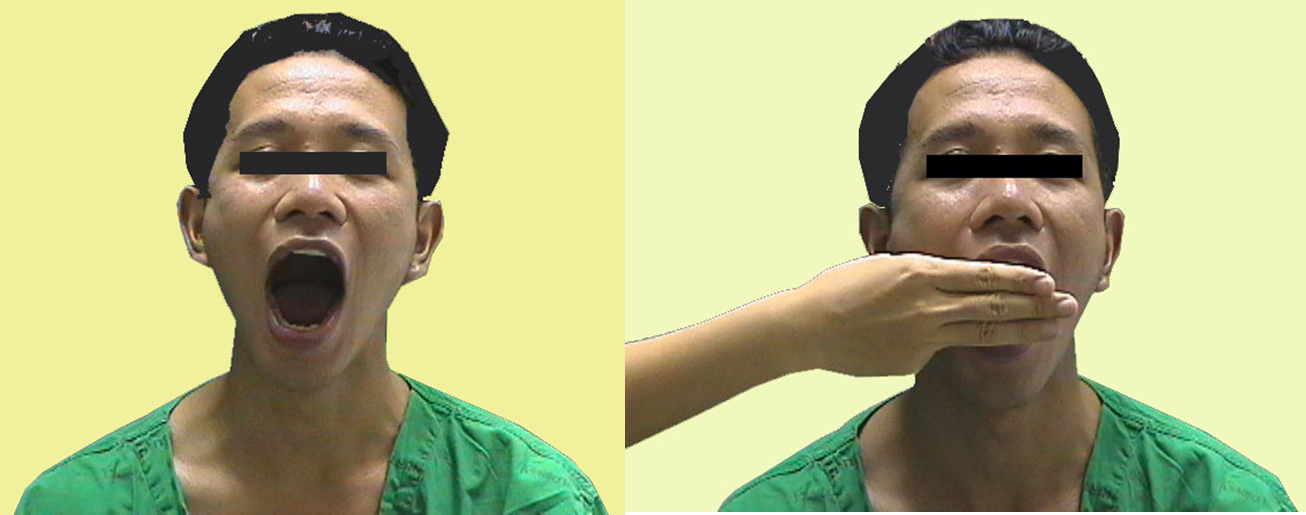
- Mallampati classification This test is performed with the patient in the sitting position, head in a neutral position, the mouth wide open and the tongue protruding to its maximum
- Class I: Visualization of the soft palate, uvula, anterior and the posterior pillars.
- Class II: Visualization of the soft palate and uvula.
- Class III: Visualization of soft palate and base of uvula.
- Class IV: Only hard palate is visible. Soft palate is not visible at all
Class III, IV difficult to intubate

- Interincisor gab: Normal >4.5 cm (3 fingers)
3) Thyromental distance (TMD) :
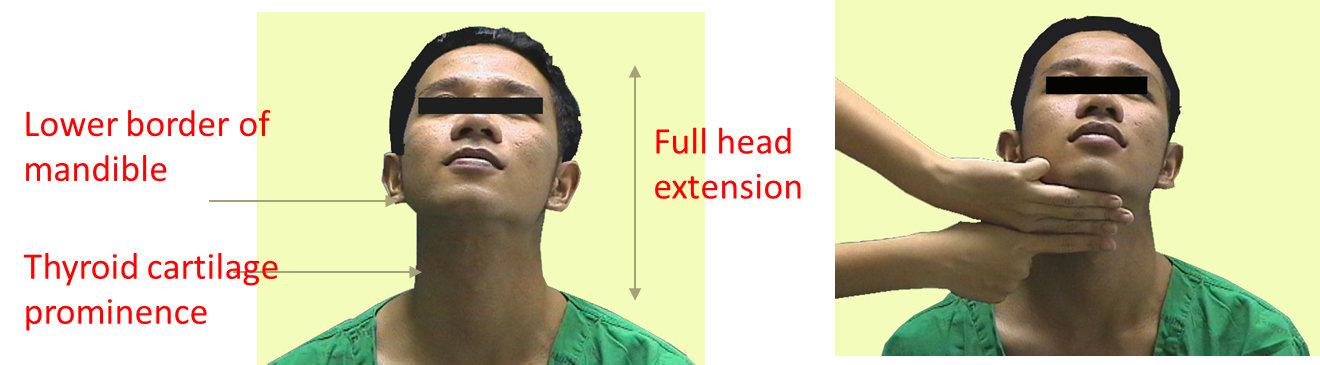
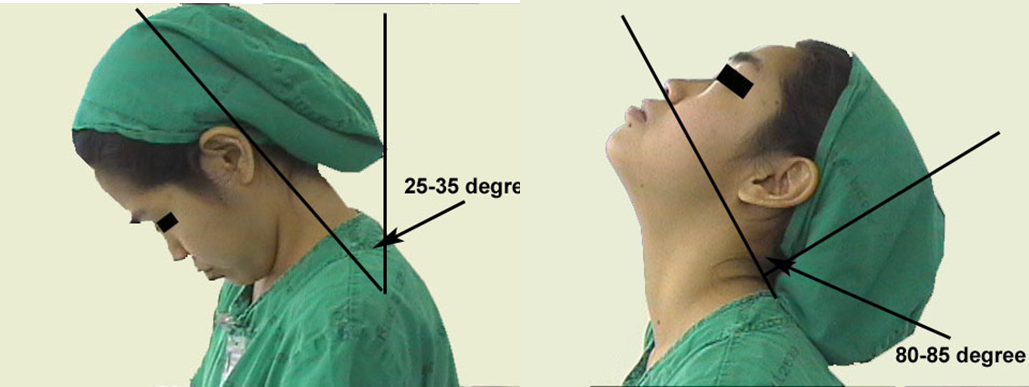
4) Flexion and extension of neck
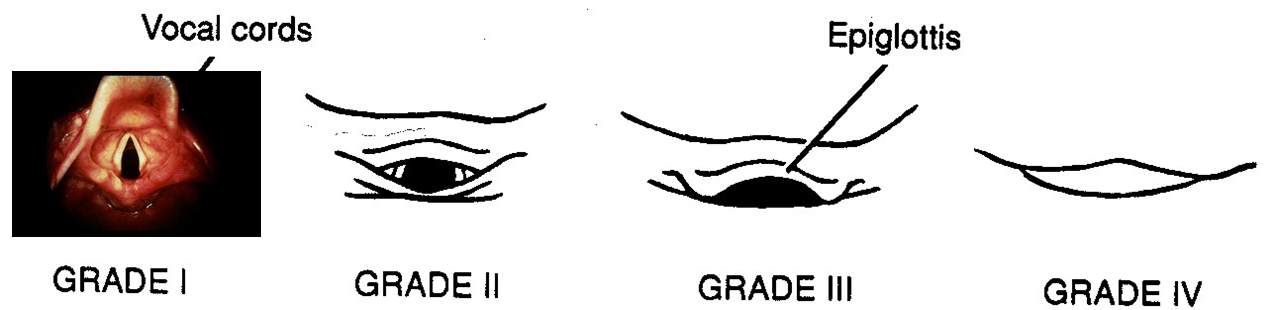
- Laryngoscopic view
6) Movement of temperomandibular joint (TMJ)

Preparing the procedure…
Essentials that must be present to ensure a safe intubation!.. They can be remembered by the mnemonic SALT
-
Suction. This is extremely important. Often patients will have secretions in the pharynx, making visualization of the vocal cords difficult.
-
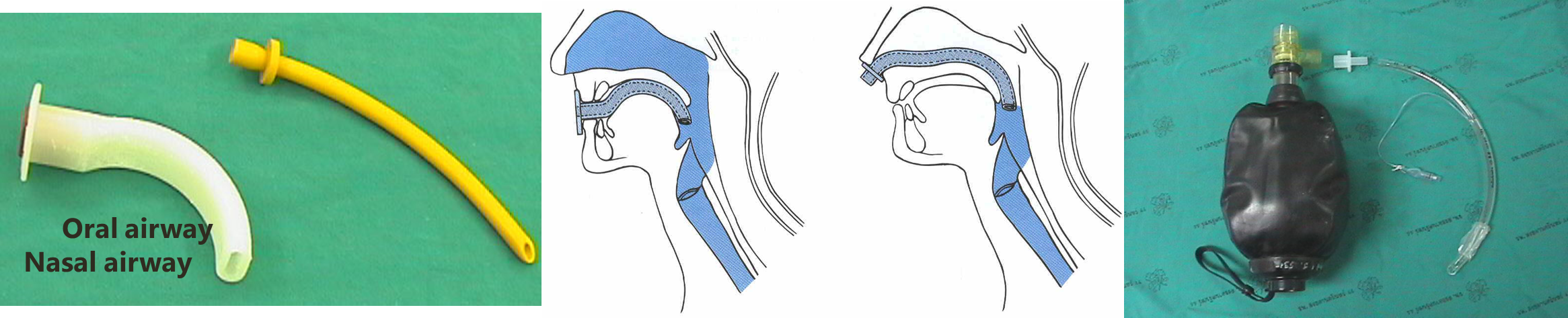
Airway. the oral airway is a device that lifts the tongue off the posterior pharynx, often making it easier to mask ventilate a patient. Also a source of O2 with a delivery mechanism (ambu-bag and mask) must be available.
-
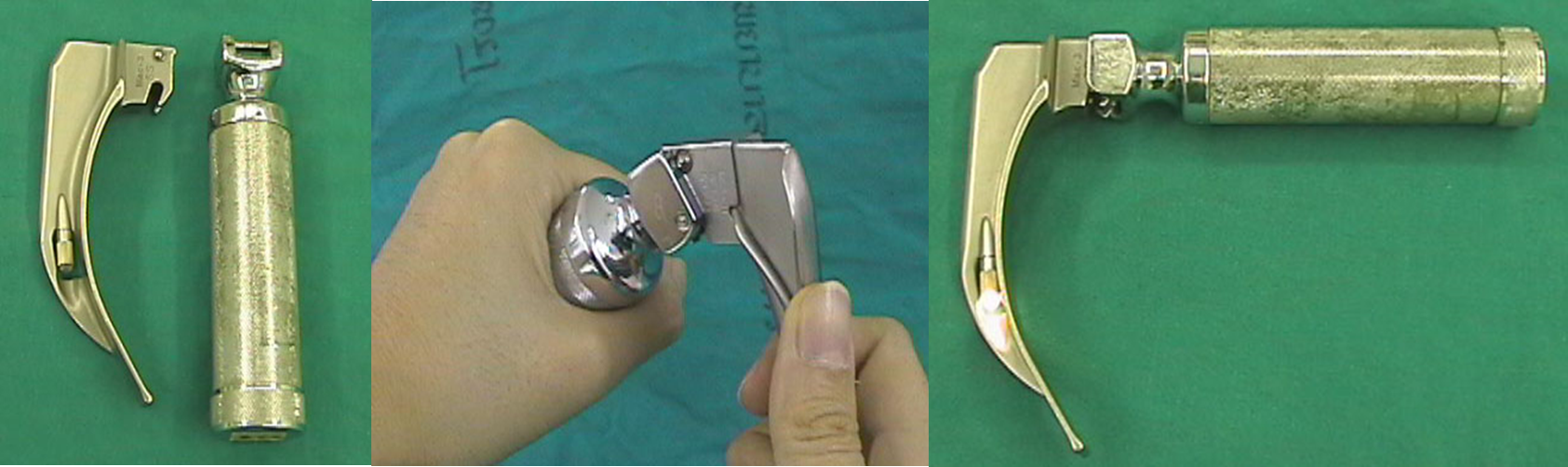
Laryngoscope. This is vital to placing an endotracheal tube.
-
Tube. Endotracheal tubes come in many sizes. In the average women adult, a size 7.0 or 8.0 endotracheal tube and 7.5 to 8.5 mm in men
Instruments used…
- Self-refilling bag-valve combination (eg, Ambu bag), tubing, and oxygen source.
- Plaster or tube holder .
- Introducer (stylets or Magill forceps).
- Laryngoscope
- Suction apparatus
- Syringe, 10-mL, to inflate the cuff.
- Mucosal anesthetics (eg, 2% lidocaine)
- Water-soluble sterile lubricant.
- Gloves.
- Pulse oximeter
- Stethoscope

Oropharyngeal or nasopharyngeal airway
Laryngoscope : handle and blade
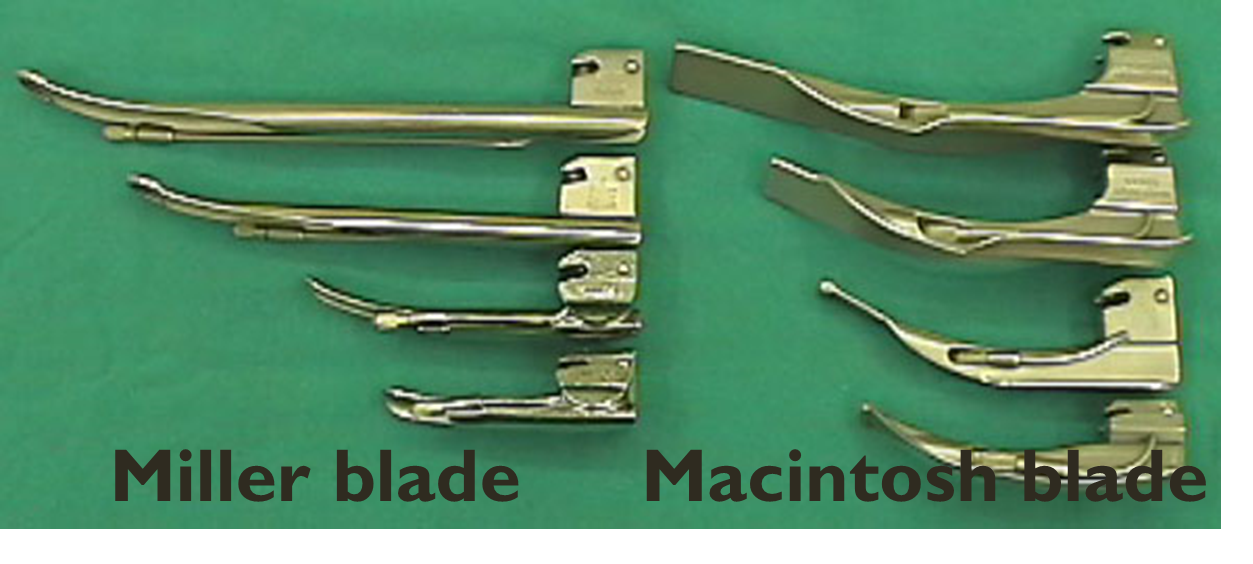
LARYNGOSCOPIC BLADE
- Macintosh (curved) and Miller (straight) blade
- Adult : Macintosh blade (No 3 and No 4),
- Children : Miller blade (No 2 and No 3)
Video Laryngoscopy (Glidescope)

2) Endotracheal tube
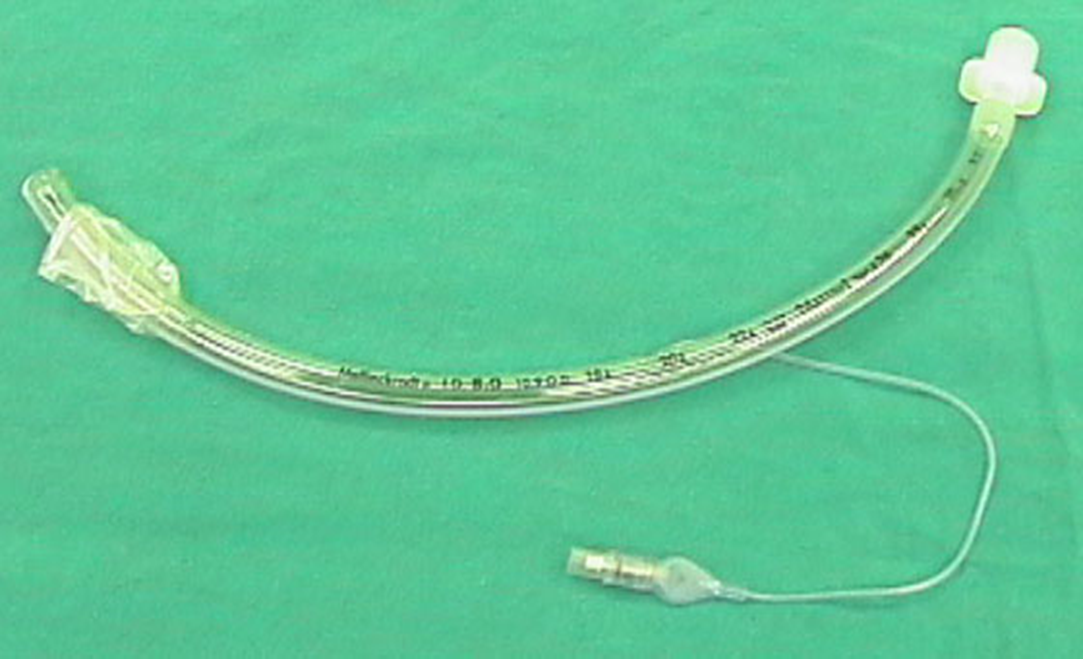
Endotracheal tube - Size of endotracheal tube : internal diameter (ID) Y
Male: ID 8.0 mms . Female : ID 7.5 mms New born - 3 months : ID 3.0 mms 3-9 months : ID 3.5 mms 9-18 months : ID 4.0 mms 2- 6 yrs : ID = (Age/3) + 3.5 6 yrs : ID = (Age/4) + 4.5
Depth of endotracheal tube :
Midtrachea or below vocal cord ~ 3-4 cms ,
- Adult: Male = 23 cms ,
- Female = 21 cms
- Children: endotracheal tube = (Age/2) + 12 (cm)
The goal is to place the tip of the ETT 2 to 4 cm from the carina (to avoid endobronchial intubation) and the proximal edge of the cuff at least 3 cm below the vocal cords (to avoid vocal cord damage and inadvertent extubaion).
Technique:
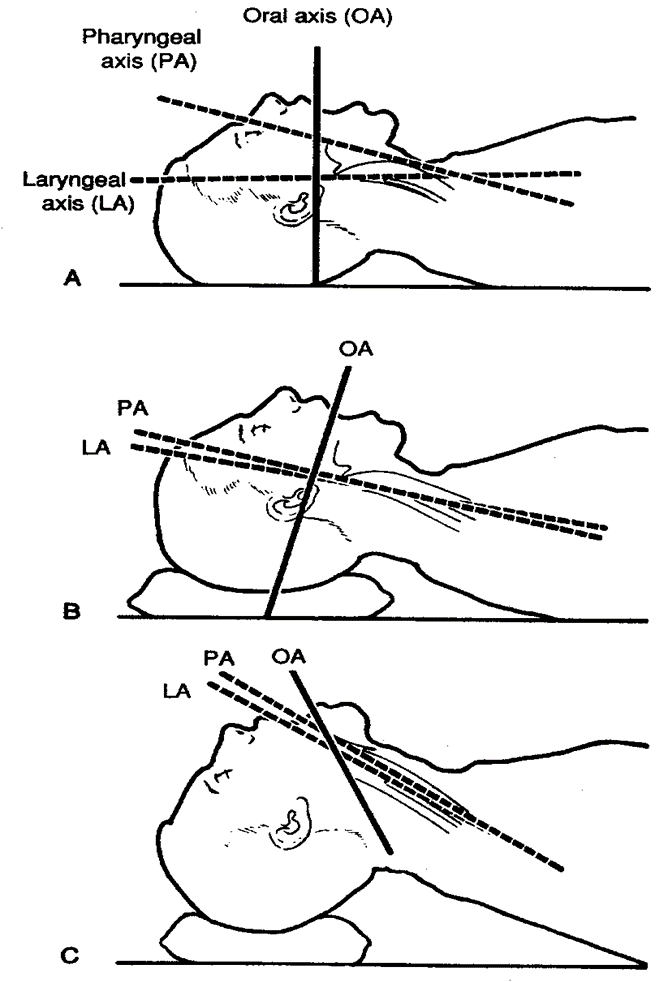
Sniffing position
- Flexion at lower cervical spine
- Extension at atlanto-occipital joint
- Make sure that all materials are assembled and close at hand
- Make sure that the balloon inflates
- Check the laryngoscope and blade for proper fit, and make sure that the light works
- Anesthetize the mucosa of the oropharynx, and upper airway with lidocaine 2%, if time permits and the patient is awake.
- Hyperventilate the patient with 100% oxygen for 1 minute prior to intubation attempt
- Place the patient in the sniffing position.
- Open the patient’s mouth with the right hand,.
- Grasp the laryngoscope in the left hand
- Spread the patient’s lips, and insert the blade between the teeth, being careful not to break a tooth.
- Pass the blade to the right of the tongue, and advance the blade into the hypopharynx, pushing the tongue to the left.
- Lift the laryngoscope upward and forward, without changing the angle of the blade, to expose the vocal cords.
- Take the endotracheal tube in the right hand and starts inserting it through the mouth opening.
- The tube is inserted through the cords to the point that the cuff rests just below the cords (between 21-23 mark on the tube)
- Holding the tube firmly in place, quickly remove the laryngoscope
- Remove the stylet from the endotracheal tube (if used)
- Finally, the cuff is inflated with 5-10 ml of air
- Ventilate the patient
- Observing the chest rise and fall with each ventilation
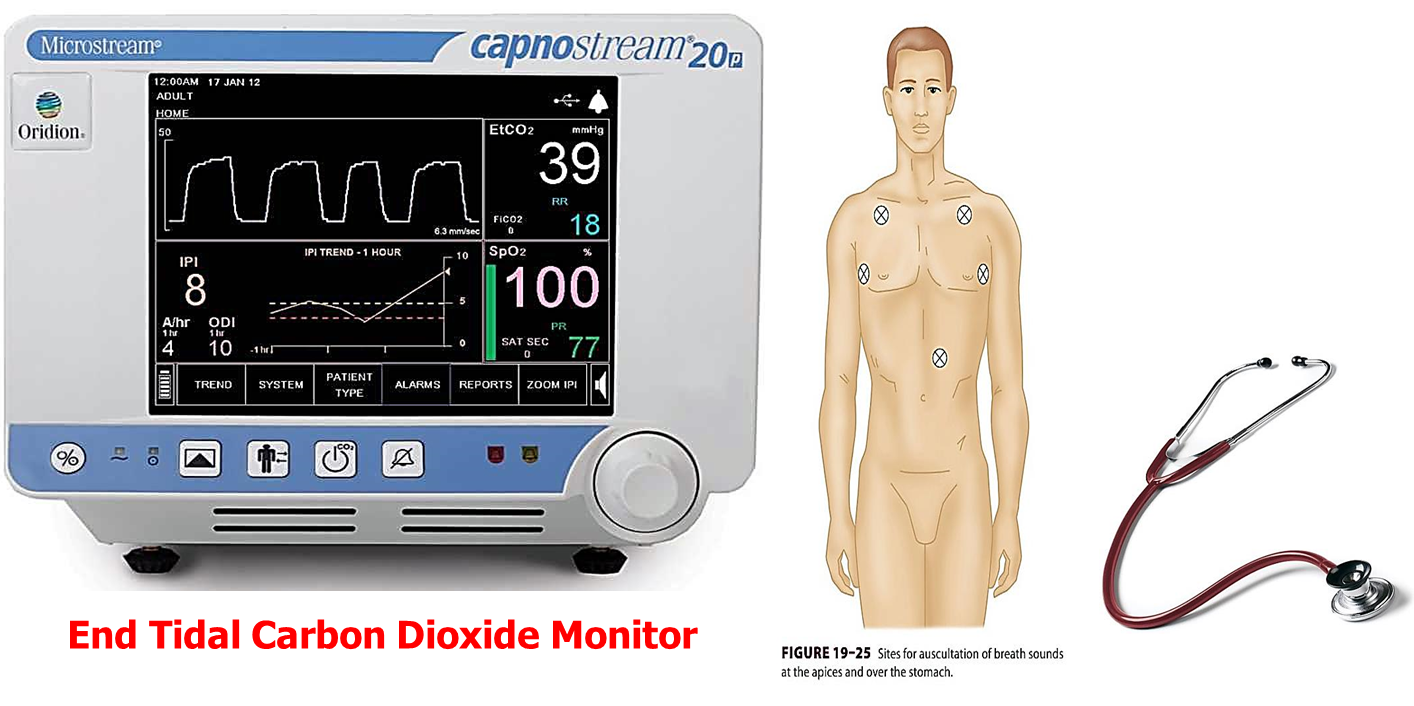
- Listens for breathing sounds to ensure correct placement of the tube (in stomach and chest)
- If no breath sounds and there is bubble sound in stomach (it is in stomach) remove the tube and ventilate the patient and start all over again
- If the tube is advanced too far, it will get into the right bronchus and only the right lung is ventilated. If this occurs deflate the cuff with draw 2-3 cm and re-inflate the cuff and listen again
- Attach the tube to the patient and to the ventilating apparatus

Confirmation of Tube Placement
-
Direct visualization of endotracheal tube
-
Auscultation: breath sounds audible over both lung fields
-
Condensation: consistently visible in the tube during exhalation
-
CO2 detection: gold standard of successful endotracheal intubation
-
Imaging CXR: The distal tip of the endotracheal or tracheal tube should be 2–6 cm above the carina Trained practitioners only: Ultrasound may be used to confirm tube position.

Complication of endotracheal intubation
- During intubation
- Trauma to lip, tongue or teeth
- Hypertension and tachycardia or arrhythmia
- Pulmonary aspiration
- Laryngospasm
- Bronchospasm
- Laryngeal edema
- Increased intracranial pressure
- Spinal cord trauma in cervical spine injury
- Esophageal intubation
- During remained intubation
- Obstruction from secretion or overinflation of cuff
- Accidental extubation or endobronchial intubation
- Disconnection from breathing circuit
- Lip or nasal ulcer in case with prolong period of intubation
- During extubation
- Laryngospasm
- Pulmonary aspiration
- Edema of upper airway
- Failed extubation
- After extubation
- Sore throat
- Hoarseness
- Tracheal stenosis (Prolong intubation)
- Laryngeal granuloma
Source:
•AMBOSS •UpToDate •Essential Clinical Procedures 2nd edition