IM & FM
Dr. Waqar & Dr.
General Points
- One of the most common medical issues.
- Multiple etiologies, some very serious and some not. So, diagnosis can be challenging.
- Most cases of chronic headache do not have a serious etiology.
- Headaches can be due to many systemic diseases, not just problems in the head.
Table of Contents
Types of headaches
-
Primary Headaches;
Not secondary to another disease
- Migraine Headache (& its variants)
- Tension Headache (most common type)
- Cluster Headache
-
Secondary Headaches;
Secondary to some underlying disease, either intracranial or extracranial
Clinical - FM
FM
Approach to Patient with Headache

Case Scenario
- A 27-year-old single female, she is a primary school teacher.
- She presents to the Surgery C/O headache for the past few months.
- She describes the headache as the band like around her head.
- The headache increases in intensity towards the evening times.
- It is relieved by taking Paracetamol for some times but it recurs.
- She mentioned that the headache is progressive throughout the day to become more intense, by the end of the day.
- She denies any other symptoms like nausea, vomiting, diplopia or flash of lights.
- Her past medical history and the physical examinations are unremarkable.
Objectives
- Classify the headaches based on primary and secondary causes.
- Identify Common causes of primary headache.
- Conduct a focused history for a patient presented with headache to identify the etiological factors.
- Identify important related physical examination to exclude serious causes.
- Assess and treat the patient presenting with headache.
- Identify red flag symptoms to exclude serious causes.
Headache Management
- Identify some rare but serious and treatable causes of headache.
- Recognize the limitations of images for the diagnosis of headache.
- Recognize the preventive and prophylactic strategies available for some types of chronic headache.
- Identify the referral criteria for headache.
- Act as a gate-keeper not to waste the resources.
Definition
- Headache is pain localised to any part of the head, behind the eyes or ears, or in the upper neck.
- Headaches represent 2% of all emergency department visits.
- About 90% of men and 95% of women have at least one headache per year.
Classification Of Headaches
- Primary: headache disorders, here the etiology is unknown
- Secondary: headache disorders, where the headache is attributed to a specific underlying cause in head or neck
- Chronic headache: Occurs on more than 15 days per month for more than three months.
Primary
- Tension-type headache
- Migraine headache
- Cluster headache
Secondary
- Infectious (dental, sinusitis, meningitis)
- Traumatic
- Rebound
- Intra-cranial hypertension (idiopathic, brain tumor)
- Temporal Arteritis
Diagnosis
- Practitioners should consider using headache diaries and appropriate assessment questionnaires to support the diagnosis and management of headache.
Red Flags
- Old age of onset of headache (>50 years of age)
- Acute onset (thunderclap) headache SAH (Worst in life - occipital usually associated w/ vomiting)
- **New headaches
- Significant change in the characteristics of prior headaches
- Signs or symptoms of systemic illness (e.g., fever, chills, weight loss, vomiting)
What are the Criteria for Low Risk Headache?Z
- Age younger than 30 years,
- Features typical of primary headaches.
- History of similar headache
- No abnormal neurologic findings
- No concerning change in usual headache pattern
- No high-risk comorbid conditions (e.g., human immunodeficiency virus infection).
Prevention
- Trials demonstrate that prophylaxis provides reduction in severity and frequency of headaches by 50%.
General Treatment
- Identify and remove the triggers
- Educate the patient.
- Exercise and diet
- Pharmacological (paracetamol).
- Regular sleep.

Prevention
- Good sleep hygiene
- Routine meal schedules
- Regular exercise
- Avoidance of triggers
- Water, Water, Water.



Summary
- Always look for common primary headaches
- All cases RED flag sign and symptoms to be excluded.
- Start with simple analgesia in primary headaches
- Patient education is an important step in management.
- Controlled use of radiological images to be utilized.
Clinical Medicine
Neurological symptoms Headache
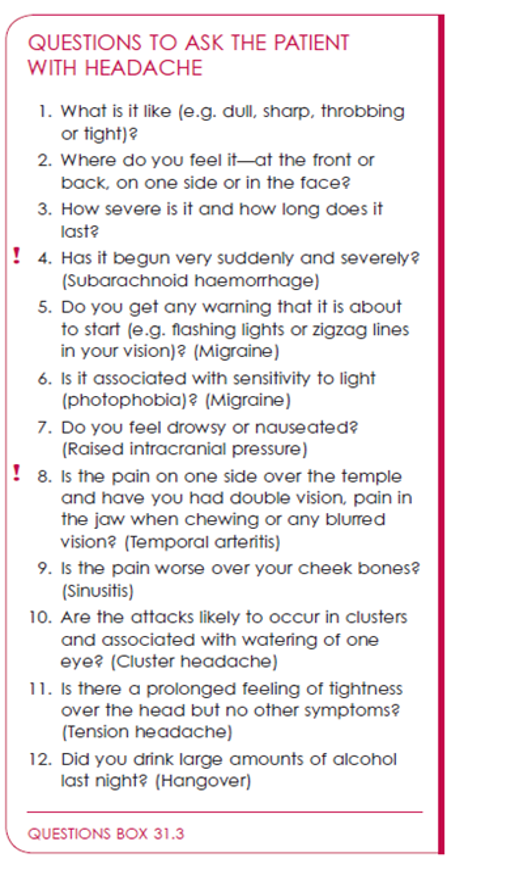
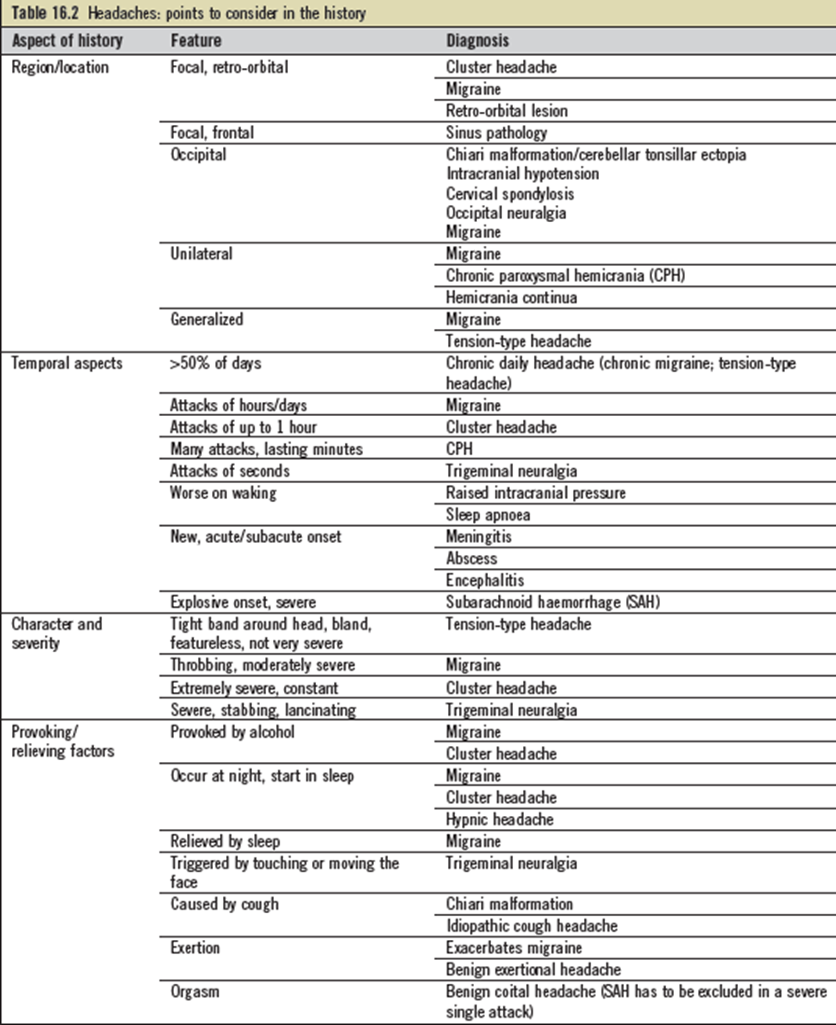
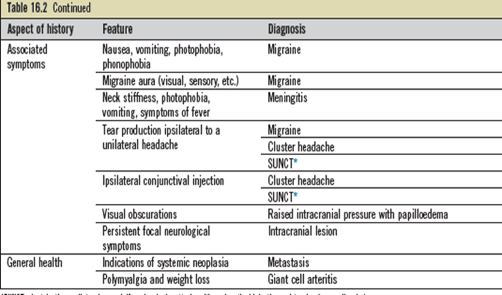
HISTORY OF HEADACHE
- A common neurological symptom
- Brain parenchyma is not sensitive to pain as it lacks pain receptors.
- Pain is caused by disturbance of pain-sensitive structures around the brain e.g extracranial arteries, large veins, cranial and spinal nerves, head and neck muscles, subcutaneous tissue, eyes, ears, sinuses and meninges
- caused by traction and irritation of the meninges and blood vessels
- Pain-sensitive structures are supplied by branches of the trigeminal nerve and upper cervical nerves: this explains the pattern of pain referral seen in intracranial diseases
It includes:
- Location
- Unilateral ~ migraine
- Periorbital (+/- visual disturbance) ~ glaucoma/uveitis
- Parietal/Occipital ~ tension
- Neck ~ meningitis or Subarachnoid hemorrhage
- Quality
- “Throbbing” ~ vascular
- “Intermittent jabbing” ~ Trigeminal neuralgia
- “Pressure” ~ sinus
- Radiation?
- Severity
- Timing
- Constant vs. intermittent
- Worse in a.m. or p.m.
- Worst headache ever?????
''Brain has no pain nerve endings so headaches are uncommon as the INITIAL Sx of a brain tumor
Suspect underlying lesion if the headache always occurs on one side
P.M. headaches may represent:
cluster headaches
intracranial lesions''
Presenting complaint
- One or several? Useful to list.
- Allow uninterrupted narrative, so far as possible
- Clarify
- Date of onset
- Frequency of recurrence
- Duration of episodes
- Evolution
- Nature of main symptom, in detail
- Associated features
- Triggers
- Exacerbating/relieving factors
- Treatment
Neurological history taking
- Headache in a 34 yr old woman
- Onset at puberty
- Attacks 1-3/month
- Few hours – 2 days
- Increasing frequency/intensity past two years
- Throbbing headache, often unilateral, either side
- 20 minutes visual disturbance, preceding headache; nausea, photo- and phonophobia with headache
- Sleeping in at the weekend; pre-menstrual week
- Worse upright, better lying flat in dark room, helped by sleep
- Helped by aspirin taken early in attack; no help if not.
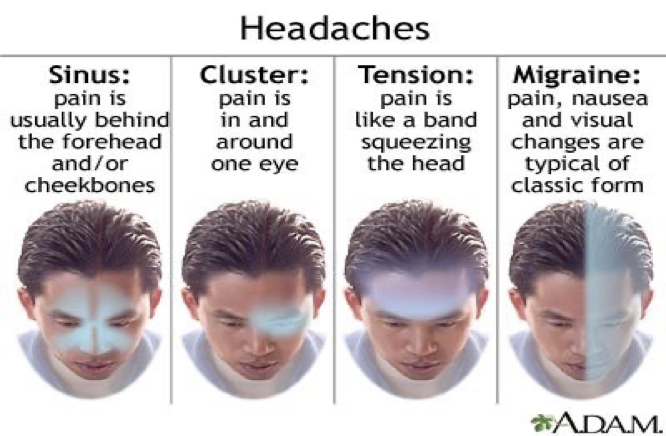
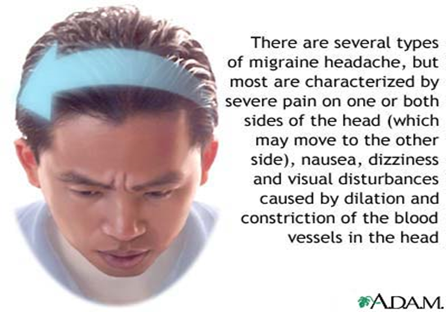
MIGRAINE
- More common in women
- Usually one sided
- Throbbing
- Mild to severe pain
- Nausea and vomiting
- Photophobia/phonophobia
- Visual aura or photopsia
- Lasts for several hours
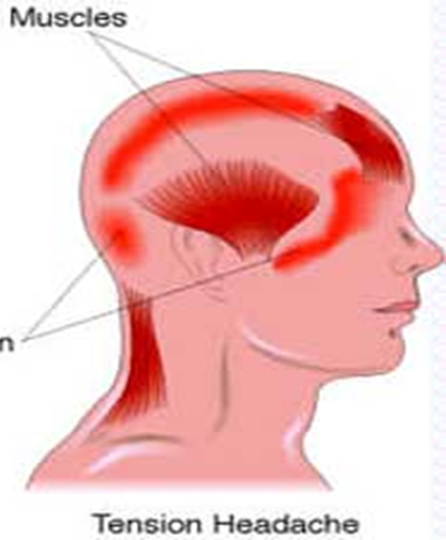
TENSION HEADACHES
- Pain usually bilateral, fronto-occipital
- Throbbing in nature
- Mild to moderate pain
- Tight band sensation
- Pressure behind eyes
- Precipitants: worry, stress, noise, etc
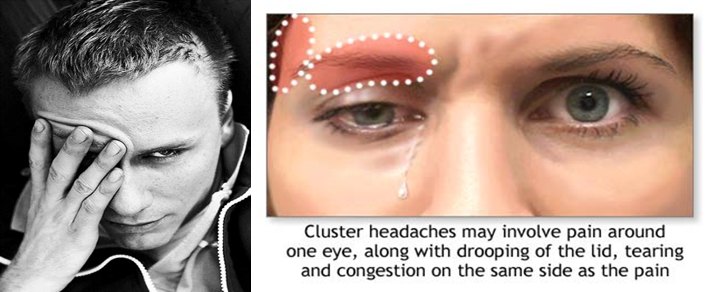
CLUSTER HEADACHES
- More common in men
- Excruciating unilateral pain around one eye
- Drooping eyelid
- Redness or tearing of one eye
- Nasal stuffiness
- Pain is brief, occurring repeatedly for weeks (in clusters) followed by a few months rest before another cluster occurs
- Attacks often provoked by alcohol
Neurological symptoms
- Headache
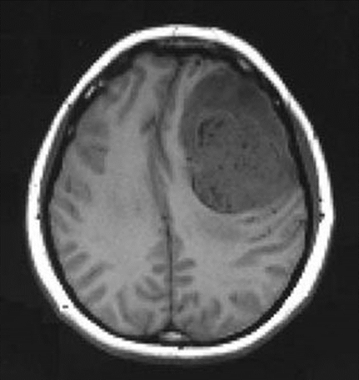
HEADACHE RELATED TO ↑ICP
- Dull ache
- Worse on waking in the morning, improves through the day
- Made, worse by coughing, sneezing, straining, bending forward or lying down
- Worsens progressively
- Associated with morning vomiting