Principles of surgical oncology
DR. AHMED KHAN
Surgical Oncologist:
“A surgical oncologist is a well-qualified surgeon who has obtained additional training and experience in the multidisciplinary approach to the prevention, diagnosis, treatment, and rehabilitation of cancer patients, and devotes a major portion of his or her professional practice to these activities and cancer research.”
Society of Surgical Oncology Training Program Guidelines, 2004
Multidisciplinary Team
Multidisciplinary approach for management:
- Surgery
- Radiation
- Chemotherapy
- Pathology
- Radiology
- Nutrition
Nomenclature:Z
-
Epithelial cells (Endoderm, mesoderm or ectoderm) – Carcinoma
-
Adenocarcinoma is a malignant tumor arising from “glandular tissue”.
-
Connective Tissues – Sarcoma
-
Blood: WBC – Leukaemia, Lymphoid – Lymphoma
-
Germ cells – Teratoma, Seminoma, Dysgerminoma (germ cells in females)
-
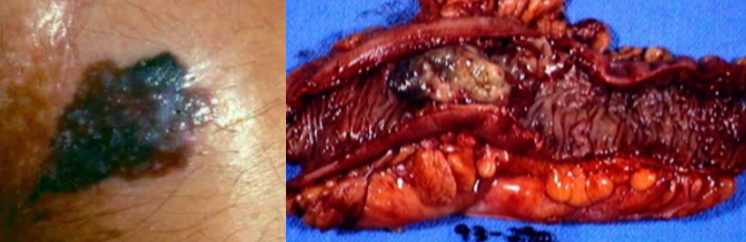
Neuroectoderm (Different names – Melanoma)
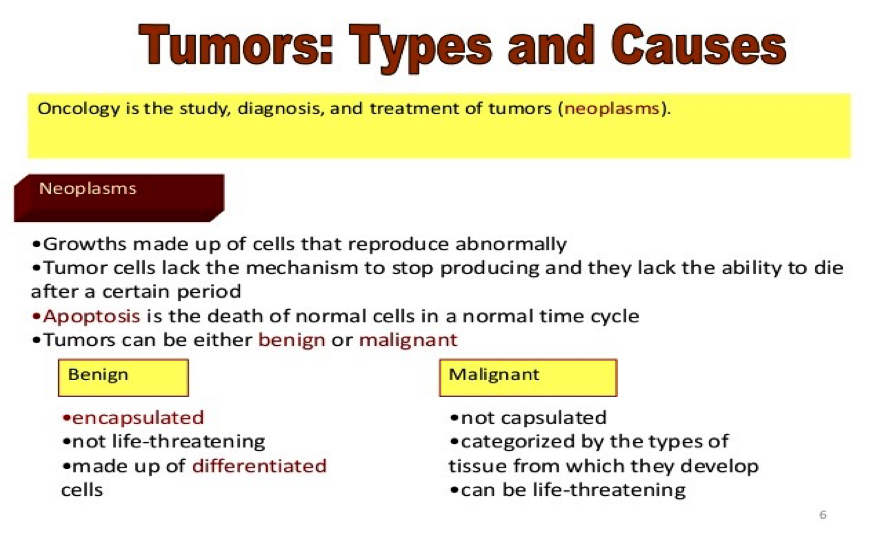
Benign versus Malignant Tumors
-
Benign
- Usually encapsulated
- Cells similar in structure to cells from which they originate
- Well-defined borders
- Slow growing and limited to one area
- Possible growth displacement (but not invasion) to adjacent tissue
-
Malignant
- Not encapsulated; not cohesive, and irregular pattern of growth
- No resemblance to cell of origin
- No well-defined borders
- Growth into adjacent cells rather than displacing or pushing them aside
- Rapid growth through rapid cell division and multiplication
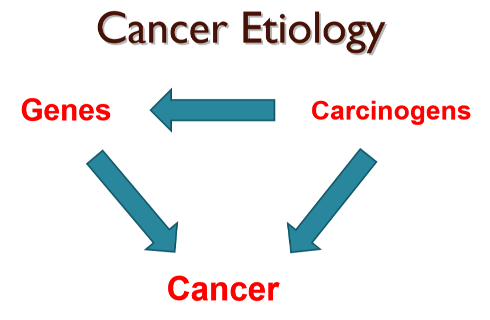
Three steps of Tumorigenesis: initiation, promotion & Progression
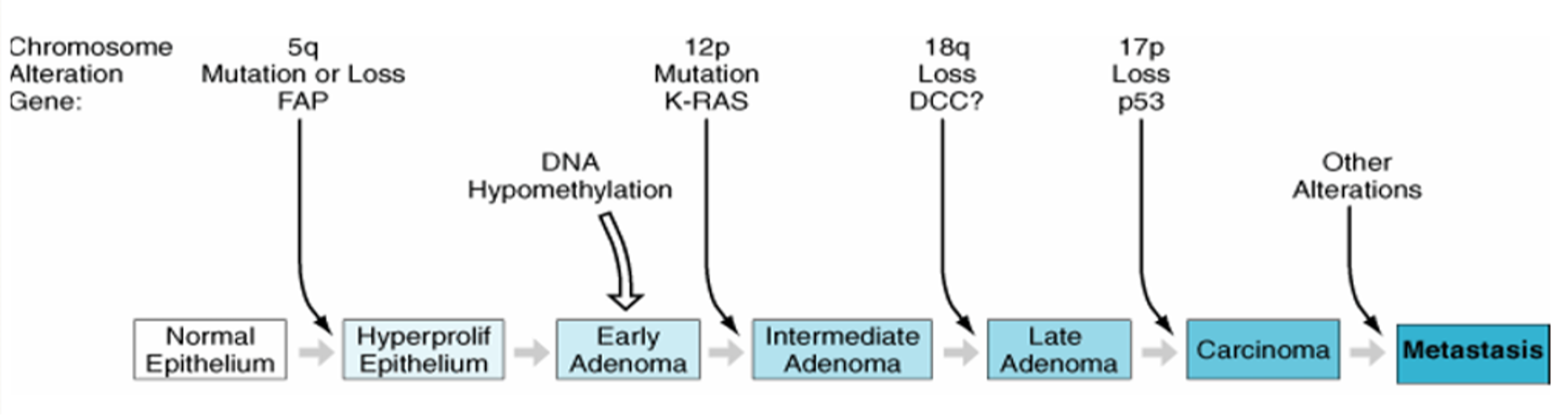
The first step in this process is initiation, which requires exposure of normal cells to carcinogenic substances.
Substances that may act as carcinogens or initiators include chemical, physical, and biologic agents.
Two major classes of genes are involved in carcinogenesis: oncogenes and tumor suppressor genes.
Genes Associated with Hereditary CancerZ
| Genes | Syndrome |
|---|---|
| APC | Familial adenomatous polyposis (FAP) |
| BMPRIA | Juvenile polyposis coli |
| BRCA1 | Breast/ovarian syndrome Breast Cancer |
| BRCA2 | Breast/ovarian syndrome Breast Cancer |
| hMLH1; hMSH2; hMSH6; hPMS1; hPMS2 | Hereditary nonpolyposis colorectal cancer |
Criteria suggest of Hereditary Cancer
- Tumor development at a much younger age than usual
- Presence of bilateral disease
- Presence of multiple primary malignancies
- Presentation of a cancer in the less affected sex (e.g., male breast cancer)
- Clustering of the same cancer type in relatives
- Cancer associated with other conditions such as mental retardation or pathognomonic skin lesions
Carcinogens
- Chemical Carcinogens
- Physical Carcinogens
- Viral Carcinogens
A) IARC Group 1 Chemical Carcinogens
| Chemical | Predominant Tumor Type |
|---|---|
| Aflatoxins | Liver cancer |
| Arsenic | Skin cancer |
| Benzene | Leukemia |
| Benzidine | Bladder cancer |
| Ethylene oxide | Leukemia, lymphoma |
| Estrogen replacement therapy | Endometrial cancer, breast cancer |
| Tamoxifen | Endometrial cancer |
| Tobacco smoke | Lung cancer, oral cancer, pharyngeal cancer, laryngeal cancer, esophageal cancer (squamous cell, pancreatic cancer, bladder cancer, liver cancer, renal cell carcinoma, cervical cancer, leukemia) |
B) Physical Carcinogenesis
- Radiation (UV .. SUnlight) & Ionising radiation
- Non-radiation (Mechanical, burns, scars, abestos, surgical implants, foreign bodies)
C) Viral Carcinogens
| Virus | Predominant Tumor Typeb |
|---|---|
| Epstein-Barr virus | Burkitt’s lymphoma |
| Hodgkin’s disease | |
| Immunosuppression-related lymphoma | |
| Sinonasal angiocentric T-cell lymphoma Nasopharyngeal carcinoma | |
| Hepatitis B | Hepatocellular carcinoma |
| Hepatitis C | Hepatocellular carcinoma |
| Human immunodeficiency virus-1 | Kaposi’s sarcoma |
| Non-Hodgkin’s lymphoma | |
| Human papillomavirus types 16 and 18 | Cervical cancer |
| Anal cancer | |
| Human T-cell lymphotropic viruses | Adult T-cell leukemia/lymphoma |
Leukoplakia of the tongue:
thick white patches on the inside surfaces of mouth (precancerous)

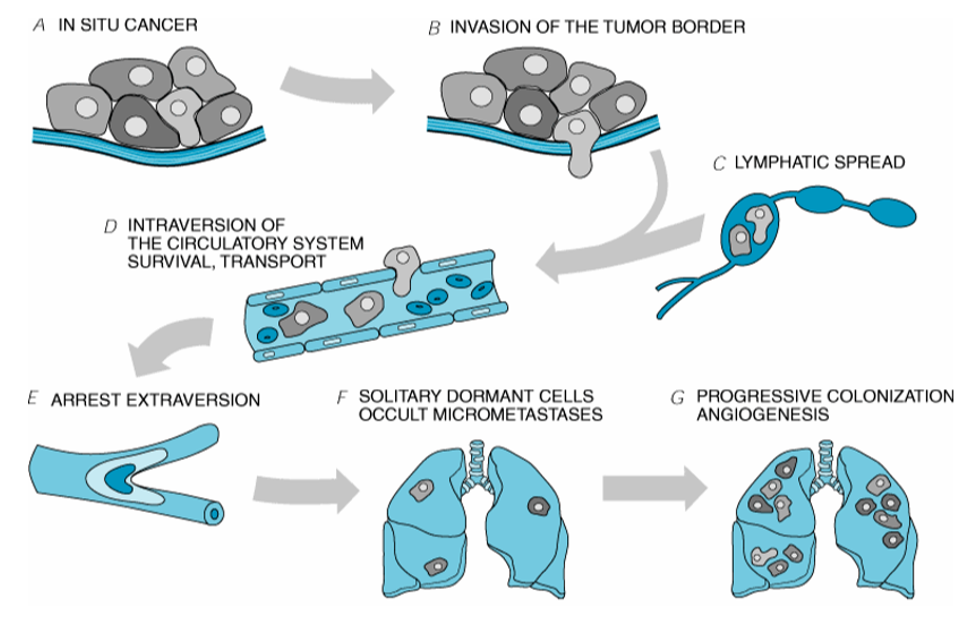
Metastatic Process
Cancer Screening
| Cancer Site | Population | Test or Procedure | Frequency |
|---|---|---|---|
| Breast | Women, age 20+ | Breast self-examination 1M 20A | Monthly, starting at age 20 |
| Clinical breast examination 3Y 20-39 1Y 40A | Every 3 years, ages 20-39 Annual, starting at age 40 | ||
| Mammography 1Y 40A | Annual, starting at age 40 | ||
| Colorectal | Men and women, age 50+ | Fecal occult blood test (FOBT) 1Y 20A | Annual, starting at age 20 |
| Flexible sigmoidoscopy 5Y 50A | Every 5 years, starting at age 50 | ||
| Fecal occult blood test and flexible sigmoidoscopy 5Y 50A | Annual FOBT and flexible sigmoidoscopy every 5 years, starting at age 50 | ||
| Double-contrast barium enema (DCBE) 5Y 50A | DCBE every 5 years, starting at age 50 | ||
| Colonoscopy 10Y 50A | Colonoscopy every 10Y years, starting at age 50 | ||
| Prostate | Men, age 50+ | Digital rectal examination (DRE) and prostate-specific antigen test (PSA) 1Y 50A | Offer PSA and DRE annually, starting at age 50, for men who have life expectancy of at least 10 years |
Ulcerative Colitis
-
40% of UC (Pancolitis) die of colon cancer
-
3% of children with UC develop colon cancer by the age of 10, and 20% develop cancer during each ensuing decade
-
Colectomy is indicated for patients with ulcerative colitis if the chronicity of this disease is well established.
Tumor Markers
| Marker | Cancer | Sensitivity | Specificity |
|---|---|---|---|
| PSA (4 g/L) | Prostate | 57–93% | 55–68% |
| CEA | Colorectal | 40–47% | 90% |
| Breast | 45% | 81% | |
| Recurrent disease | 84% | 100% | |
| AFP | Hepatocellular | 98% | 65% |
| CA 19-9 | Pancreatic | 78–90% | 95% |
| CA 27-29 | Breast | 62% | 83% |
| CA 15-3 | Breast | 57% | 87% |
Diagnosis of cancer
Acquisition of tissue for exact histological diagnosis ⇒ biopsy
Biopsy
- Aspiration Biopsy
- Needle Biopsy
- Incisional Biopsy
- Excisional Biopsy
Frozen section examination:
A measure of the adequacy of the oncological surgical operation.
-
The operative specimens need to be correctly orientated by the surgeon.
-
The key issues are: whether the margins of the specimen removed are clear of tumour.
-
The total number of lymph nodes excised together with the number of involved lymph nodes.
Margins of surgical excision
In general, a margin of 2–5 cm is suggested.
BUT
-
For excision of melanomas, the depth of excision is more important than the extent of surrounding skin. A margin of 2 cm usually suffices in contrast to the 5cm previously practiced.
-
For oesophageal resection, the majority of the oesophagus needs to be resected because the tumour does spread up and down in the submucosal plane.
-
Soft tissue sarcomas may spread along aponeurotic planes so that complete excision requires the resection of the entire muscle group and fascial compartment.
-
Rectal cancer occurs in perirectal tissues has led to the use of the total mesorectal excision of the rectum.
Definitive surgical therapy with sufficient margins is sufficient local therapy
-
wide excision of primary melanomas of skin can be cured locally by surgery alone in 90% of cases.
-
The resection of colon cancers with a 5-cm margin from the tumor results in anastomotic recurrences in fewer than 5% of cases.
Cancer Staging
American Joint Committee on Cancer (AJCC) Union Internationale Contre Cancer (International Union Against Cancer, UICC)
three components:
- Primary tumor (T),
- Nodal metastases (N),
- Distant metastases (M)
Clinical staging (cTNM or TNM), Pathologic staging (pTN M), re-treatment (rTNM) or autopsy staging (aTNM)
Staging: Why?
- To aid the clinician in planning treatment
- To give some indication of prognosis
- To assist in evaluating the results of treatment
- To facilitate the exchange of information between treatment centers
- To contribute to continuing investigations of human malignancies
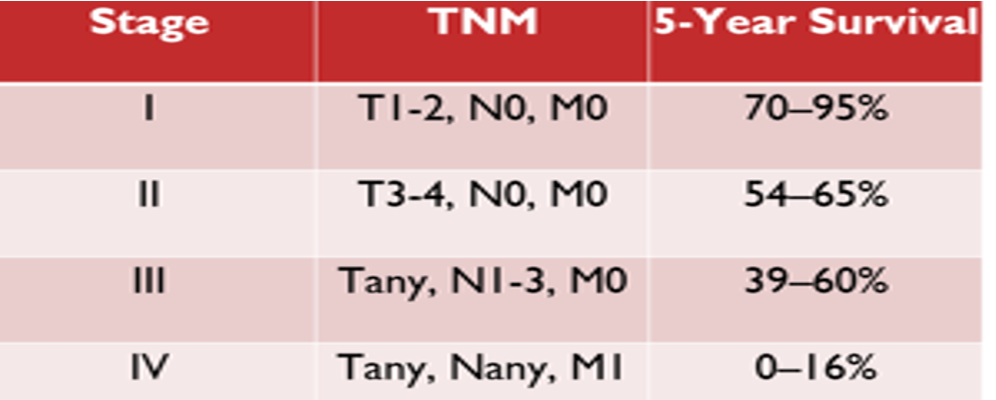
Anatomic Staging
Based on three components:
- T: The extent of the primary tumor
- N: The absence or presence and extent of regional lymph node metastasis
- M: The absence or presence of distant metastasis
Therapy
-
Primary (or definitive) therapy en bloc resection of tumor with adequate margins of normal tissues and in some cases regional lymph nodes
-
Adjuvant therapy refers to radiation therapy and systemic therapies, including chemotherapy, immunotherapy, hormonal therapy, and increasingly, biologic therapy.
Radiation therapy, often combined with chemotherapy, so-called chemoradiation:
- May be used preoperatively to reduce the bulk of a large primary tumour in order to improve successful surgical resection. (neoadjuvant therapy)
- Post-operatively (adjuvant therapy).
Some cancers can be cured with chemotherapy alone. Testicular tumours and Hodgkin’s disease are such examples.
Types of surgery in cancer treatment Based on outcome:
- Curative surgery
- Palliative surgery
- Debulking surgery
- Preventive prophylactic surgery
- Diagnostic surgery
- Staging
- Supportive surgery
- Restoration surgery
- Oncoplastic surgery
- Radioablaton surgery