Principles of Ethics
Four Pillars of Medical Ethics
- Autonomy الاستقلالية
- Beneficence الاحسان
- Non-Maleficence غير مؤذ
- Justice العدالة
Informed Consent
A competent 30 years old lady, 38 weeks pregnant refuses to have a cesarean delivery despite the fact that without surgery, the fetus could die. Both her surgeon and psychiatrist have failed to convince her to have the surgery. What is the most appropriate action for her surgeon to take at this time
What is Informed Consent
- “Informed consent is a consent obtained freely, without threats or improper inducements, after appropriate disclosure to the patient of adequate and understandable information in a form and language understood by the patient on.
- The patient should be informed about:
- The expectation of benefit
- Other reasonable alternatives
- Possible risks that are known
- It can be given orally, by signing a form or a written statement or simply agreeing by a gesture.
- It must always be obtained in advance.
Requirements for Valid Consent
- Patient should be:
- Competent i.e., should have the capacity to make a decision. (free of a defect of mind or judgment, or not be a minor)
- Must do it freely and voluntarily (without threat)
- Doctor must give options to choose from and patient not to fear a rejection or neglect by the doctor in case he or she refuses to agree. (no threat)
- Doctor must also ensure that the information has been clearly understood. ( consequences & side effects )
PREPARED System
- There is general agreement that consent must be genuinely voluntary and made after adequate disclosure of information
- The PREPARED checklist is a useful tool to ensure covering all required aspects
THE PREPARED SYSTEM: A CHECKLIST TO ASSIST THE PATIENT AND PROVIDER IN THE PROCESS OF INFORMED CONSENT
| P | Plan | The course of action being considered |
|---|---|---|
| R | Reason | The indication or rationale |
| E | Expectation | The chances of benefit and failure |
| P | Preferences | Cultural and patient-centered priorities (utilities) affecting choice |
| A | Alternatives | Other reasonable options/plans |
| R | Risks | The potential harm from plans |
| E | Expenses | All direct and indirect costs |
| D | Decision | Fully informed collaborative choice |
Exceptions to the Rule of Informed Consent
-
Patients brought into emergency and accident departments (unconscious, alone & require life-saving measures)
-
Child under 16 years (in these cases, the parents may be given this right)
-
Impaired capacity to give consent (The guardian)
Confidentiality
How Much?
A doctor is expected to preserve absolute confidentiality on all that they know about their patient, not only during the treatment but also after it and even after the patient’s death.
A 30-year-old woman, is diagnosed to have post partum psychosis and she wants to kill the child thinking that he is a monster.
At this point, the physician’s best course of action is ?
Breaches of Confidentiality
- When a patient authorizes to do so in situations such as, while seeking employment.
- Medical report or opinion for the employer.
- Report prepared for a second opinion.
- Health care team.
- Disclosure is in the best interest of the patient.
- Public interest
- Holding back the information can cause harm to the members of the society.
- Legal requirement as in matters of Laws on Public Health control of diseases such as cholera, smallpox, plague, or venereal diseases.
- For research purposes but only as anonymous data after consent of the patient.
A 32-year-old woman with a positive test for human immunodeficiency virus (HIV) antibodies refuses to notify her husband because of fear of end of marriage.”
The doctor’s best response ?
Modern Principles of Data Protection
- Data shall be accurate and up to date.
- Stored data should be adequate, relevant, not excessive
- Data is available to the patient to verify factual accuracy.
- Data is not stored for longer than will serve the interests of the patient.
- Data protection shall include security against improper access
Justice, Beneficence, Non-Maleficence
-
Justice: Race, sex, and religion are not considered morally legitimate criteria for the distribution of benefits
-
When resources are scarce, issues proper and clear distribution of care should follow clear guidelines that are fair and free of bias.
-
Beneficence: be nice, be better and kind.
-
Non-Maleficence: Do no Harm “first, do no harm,” originated from the Hippocratic school, and although few would dispute the basic concept, in day-to-day medical practice, physicians and their patients may need to accept some harm from treatment (such as necessary surgical trauma) in order to achieve a desired outcome.
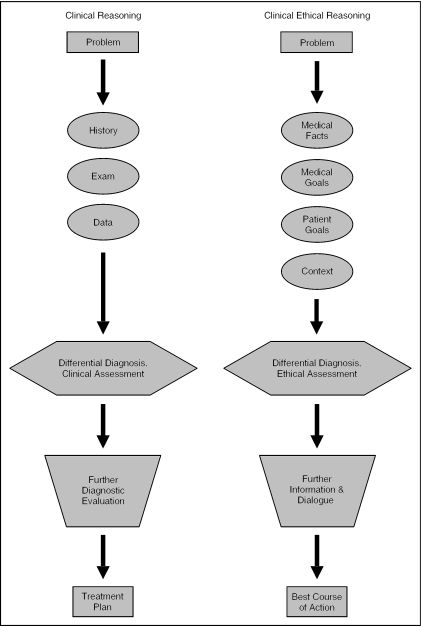
How Ethics Interact with Clinical Decisions?
Appraise the Principles of Ethics
Clinical Reasoning
- Problem
- History
- Exam
- Data
- Differential Diagnosis, Clinical Assessment
- Further Diagnostic Evaluation
- Treatment Plan
Clinical Ethical Reasoning
- Problem
- Medical Facts
- Medical Goals
- Patient Goals
- Context
- Differential Diagnosis, Ethical Assessment
- Further Information & Dialogue
- Best Course of Action
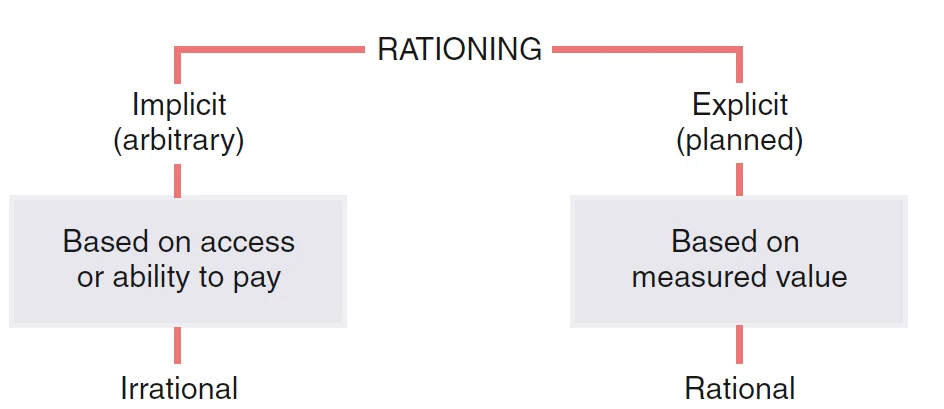
Rationing
- Implicit (arbitrary)
- Based on access or ability to pay
- Irrational
- Explicit (planned)
- Based on measured value
- Rational
Remember
-
The interface of medicine and the law raises major ethical issues because legality and morality are not always synonymous.
-
If your are not sure , you can always consult the Ethical committee in your hospital
-
Do what is in the best interest of your patient and her wishes or goals and keep her informed