Hx Taking
1) Demographic
Name, age, Martial status, Nationality, Residency,
(Occupation also can be said in social history)
EX: 54 year old male driver, not married, lives in apartment in riyadh
2) Chief of complaint
why did you come to hospital; write same as “Abdominal pain ((not specific to Epigastric pain))
3) HPI
- HPI features⇒
- associated symptoms + days + detail, then with exclusion + leg swelling
- B symptoms; weight loss, loss of apetite, fever, night sweats
- then lastly systemic review (could be after past hx)
Complaining of 5 day hx of progressive diffused abdominal pain relieved by sitting, exacerbated by movement associated with… no reported b symptoms… no other system findings…
you can ask abou
in depth Systemic review always yes or no question - direct questions
CNS Sys
- ICP; Symptomps
- Motor weakness
- Sensory; parathesia in DM, hemiparesis
- CNV; ask on all cranial nerve symptoms
- Cerebellar; Abnormal movement
- Sphincter; Bladder - autonomic; DM CNS
Cardiac Sys
- Ischemic; Retrosternal pain, Stabbing/Heaving, Radiation proximity, increased with exertion, relieved with glycerine; coronary heart disease; MI, Angina etc..
- Non-Ischemic; Diffused chest pain, increased with cough, strain, breathing; skin infection neuralgia, muscle myopathy, rib fracture/truama costrochondritis, pleural effusion, parynchemous lung, Pulmonary Embolism, SOB
- Grade of dyspnea I-IV; association w/ orthopnea? pillow? wake up w/ SOB? ; paroxysmal
- CVS cause dyspnea; pericarditis, myocardial infarction, valvular heart disease
- RESP cause dyspnea; pneumonia, TB, initial lung fibrosis, cough, Hemoptysis, use of accessory muscles
Resp Sys
- Productive; Phelgm / Nonproductive;Dry - amount, Color, Smell
- Asthma, COPD, Bronchiestasis,
- hemoptysis; resp | Hematemesis; git - frequency, clotting
- bleeding tendency, severe mitral stenosis
GIT Sys
Upper: Heart burn, neusea, vomitting, abdominal pain, dysphagia
- Dysphagia; timing of swallow - oropharyngeal vs esophageal | liquid or solid on dysphagia | Continuous or interrupted | Presentation of: scleroderma, malignancy, Infection, Neusea, vomitting, heart burn, epigastric pain; left
- Pain Radiation
Heaving/ Colicky pain: ?
Radiation epigastric to right shoulder: cholecystitis
Epigastric to back: Pancreatitis
Relieved by leaning forward: pericarditis
- Melena; dark stool if upper GIT blood
- Renal Symptoms: Pyelonephritis, renal stone w/ fever, bone ache, lost of apetite ||| lower with frequency/urgency/like tea?
Lower: ??? CC
itching; obstructive jaundice,
urine, stool, vomitting, loss of weight, job, iv, sexual, fever
autimmune = thallassemia, hemolytic anemia
infectious= malaria
paracetamol liver toxicity - 5 times per day
old age; pancreatic cancer
Gym; anabolic steroid - cholecstsyic jaundice
MSK
-
Joint pain;
- Arthritis; redness, Hotness, swelling, tenderness, limited motility
- Arthralgia;
-
Mechanical vs Inflammatory
- Mechanical; Traumatic - constant bone ache, increased with activity
- Inflammatory; morning stiffness improving with activity
-
Type of Joint
small joint of hand -
Large joint - -
Symmetry
-
Associated Rheuma Symptomps
Autoimmune, SLE, Rheumatoid Arthritis, Lupus
4) Past HX
past medical:
- similar episode as before - (you can mention with HPI)
- Chronic diseases + Family Hx / similar conditions
- Past Admission + transfusion + Surgeries
- Pregnancy / Lactation
- Medication (name dose side effects)
- Allergy
Social: im going to ask some specific question to reach to diagnosis, may i?
- Occupation, Travel, kids, smoking, alcohol, drugs, sexual activity
5) Summary
77 yo sudanese male complaining of chest pain for 9 days which was severe compressing radiating to back associated with cough, with no hx of palpitation, syncopal attack - with hx of cabg.
6) Differential, Impression
put three differential for example;
- autoimmune,
- malignancy,
- infection
7) Workup / Investigation
routine; Blood sugar, electrolyte, CBC
Related to System - Spirometry, Bronchoscopy, MRI, CT etc… ANA antibody sle, specific tests - ANTI-TPO; Thyroid
B- Examination
- introduction, explain examination -
- Exposure | position | privacy (important to mention in every exam process)
1- General Appearance
- Conscious and alert
- features
- connected devices
Summary for general Appearance
EX: elderly male with good build lying comfortable to be - connected to cannula - not connected oxygen. (note general exam findings)
EX: young boy morbidly obese, in resp distress connected to oxygen
2- General examination: ask for Vitals - CHECK Leg swelling
dont touch patient until needed
-
Hand: organized explaination from distal to proximal
- distal - nail, feature…
- dorsum - no janeway…
- flip hand - no osler node…
- specific - cardiac, GIT, Resp
- no infection, no swelling, no deformitiy in dorsum
- no palmar erythema:liver cirrhosis, mitral stenosis , rheumatoid arthritis
- No janeway lesion: CVS
- Leukonechia kolionechia
- Clubbing (window test); Hypoxia; angiogenesis many causes— likely resp cvs, congenital heart diseases, malignancy
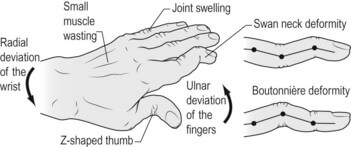
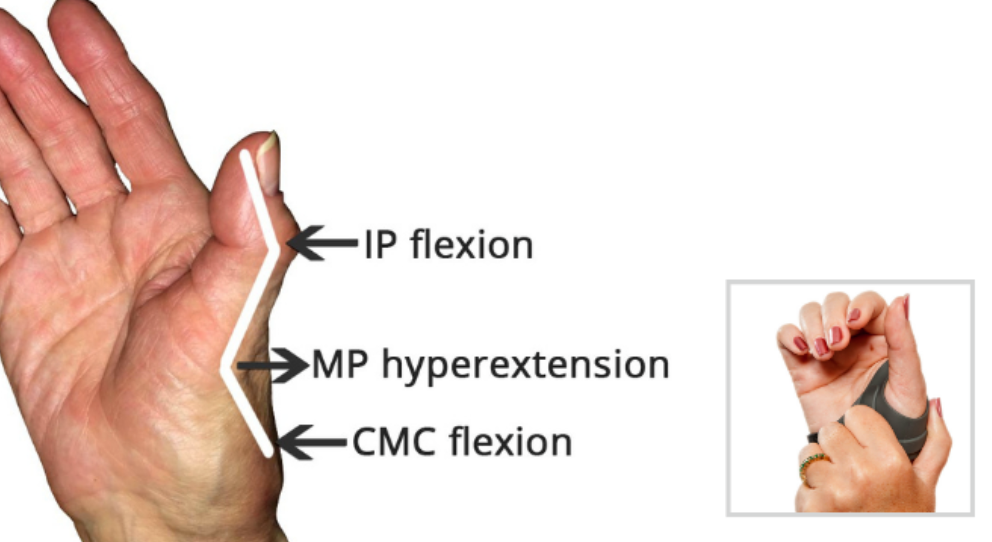
- Rheumatoid deformity w/ ulnar deviation - Z shape thumb, fixed not correctable - ((swan neck vs boutonniere??))
- Sweaty; Hyper
- Thick: Depature contracutre???, hypothyroidism
- Dry: hypo
-
Clubbing - window test
-
Capillary refill
-
Pulse: (rate | rhythm | character | volume | comparison | radioradial delay)
- Dorsalis pedis
- Medial Malleolus
- Popliteal arteria
-
water hammer pulse
-
Vital signs - BP, RR, Temp, Pulse, saturation, - mention need to check
-
Face & Neck: head to neck
- general appearance
- Hair: normal hair distribution
- eye: no pallor/jaundice
- Nasal: no nasal discharge
- Mouth: oral hygiene, central cynosis, oral ulcers
- Neck: no obvious thyroid LN JVP, cyst, swallow - want me to examine?
-
Abdomen: general palpation -
-
Lower Limb: Edema - thumb
Edema Grading- GRADE I: edema from dorsum of foot & then behind medial malleolus bilateral;
- GRADE II: Tibial
- GRADE III: Pinching, catching fold of skin on thigh to check edema
- GRADE IV: Antero-Abdominal wall; peduea orange appearance, thick, red +++ Sacral edema; ascites ((generalized anasarca?))
3- Specific system exam
… revise https://medatlax.com/Clinical/Level-8/Clinical-Medicine/Clinical-Medicine
4- thank patient, then document it
5- Summary
old age gentlemen comfortable in bed not in resp distress positive
central cynosis, decrease air entry on right side, lower limb edema
Other notes?
-
Giddiness; sense of blackout when standing up
-
Extrasystole? - af? - irregular ireggularities>
-
leg swelling; edema, SOB; dyspnea
-
smell sputum abcess foul, productive
-
Severe mitral stenosis might present with hemoptysis
-
Aortic Regurge collapsing pulse/ nodding sign
- anemia, paggets disease, pregnancy, thyrotoxicos
- av shunt
-
MCV type of anemia?
-
Platelet count thrombocytopenia; skin rash bleeding tendency
-
ITP, Heparin induced, SLE, Von wil dis, TTP
-
check edema
-
Grades of edema
-
causes of unilateral
-
causes of bilateral: renal, liver, heart…
-
infection, malignancy, autoimmune
-
ROutine Labs - signs each cbc
Examination
A- Cranial Nerve Examination
5th 7th 8th most commonly appears in exam
Cranial Nerves
CN I - Olfactory;
Smell test, close one nostril, test the other. Disease that effect it: - COVID 19, Cold, flu - Meningioma - Truama - Surgery - Frontal Lobotomy - Congenital - Kallman’s syndrome -FSH LG = Hypogonad, anosmia
CN II - Optic Nerve
Disease that effect it: - Multiple Sclerosis - Diabetes - Pituitary Tumor
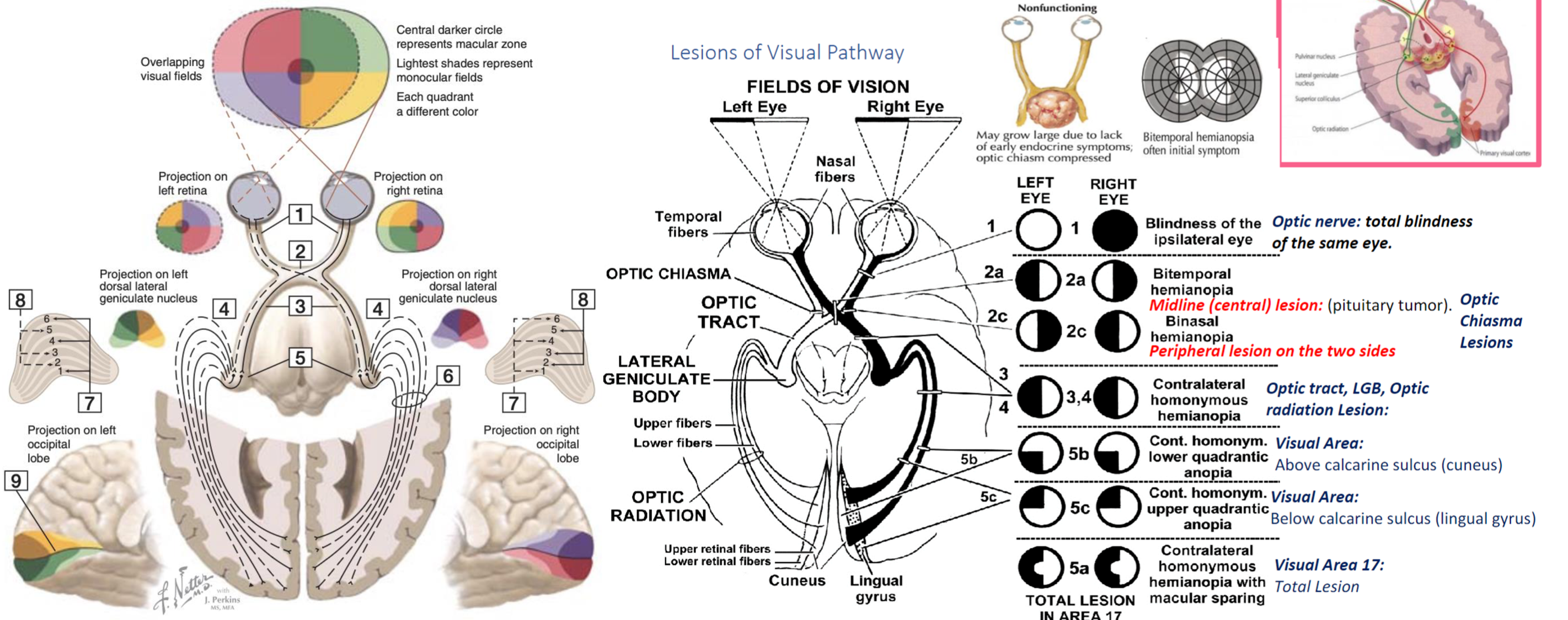
Examination - Visual acuity - (snellen chart) - 6 meters, if negative, test with numbers of fingers, then movement of hand, then light stimulation otherwise the patient is light blind. - Ischehara test - Color blindness related conditions; (X-Linked, Digoxin or anti-tuberculosis; Ethambutol) - Visual Field - Confrontation test - stay in same level to the patient, test one eye, close the other same as you - let the patient stare at your eyes without any movement. pull your finger towards center to confirm first sight with finger shaking, use your visual field as reference point. - testing temporal outer and nasal from central
Its important to know diseases related to the damaged lesion; Aforementioned in this graph
Other Tests includes
Indirect Light Reflex Testing:
- Use a dim torch as a light source rather than a phone to avoid excessive brightness.
- optic nerve, following its pathway to the midbrain and the Edinger-Westphal nucleus, which relays information to the oculomotor nerve, resulting in pupillary constriction.
Accommodation Reflex:
- Observes pupillary constriction when focusing on an object moving from a far to a near distance, assessing the accommodation ability of the eye.
Funduscopy:
- For a direct examination of the patient’s fundus, align your eye with to the patient’s right eye - your left arm on left shoulder of patient.
- Close your own opposite eye to avoid distraction and move closer progressively until you identify the yellow optic disc area surrounded by blood vessels.
- During this examination, observe the light reflex, which can provide additional information on the reflective properties and health of the optic nerve and retina.
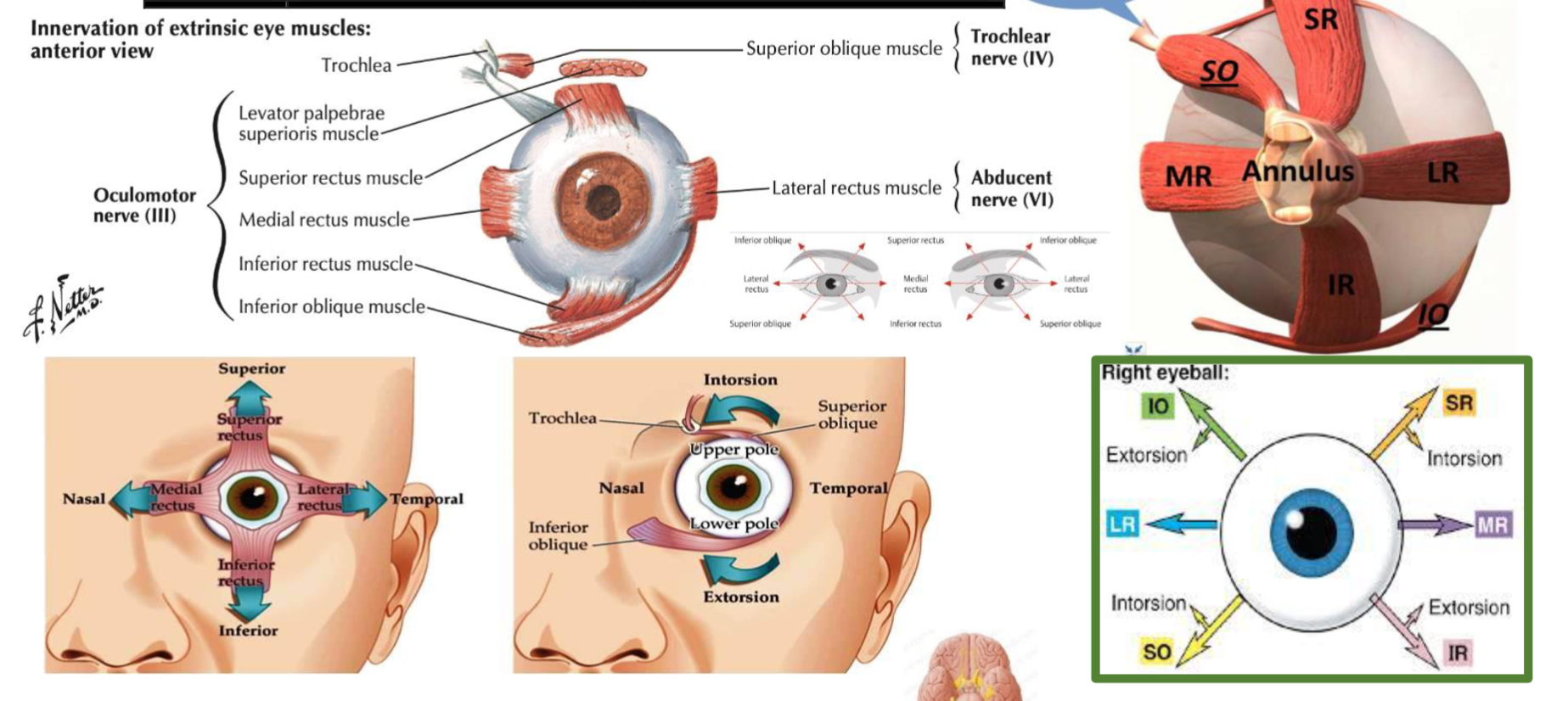
CN III, IV, VI -
Superior orbital fissure Signs: - Look at your nose to test Trochlear alone if both eyes look towards nose - if to test the other eye, ask patient to look on left or right side to find lateral rectus lesion - H test switch fingers at middle - to test otherwise
Occulomotor nerve palsy: - SLE , - Diabetes, - Tumor from outside emergency for surgery - if no papillary reflexes - cavernous sinus thrombosis
| Muscle | Innervation | Action |
|---|---|---|
| Superior Rectus | Oculomotor nerve (CN III) | Elevates, adducts, and medially rotates the eyeball |
| Inferior Rectus | Oculomotor nerve (CN III) | Depresses, adducts, and laterally rotates the eyeball |
| Medial Rectus | Oculomotor nerve (CN III) | Adducts the eyeball |
| Lateral Rectus | Abducens nerve (CN VI) | Abducts the eyeball |
| Superior Oblique | Trochlear nerve (CN IV) | Depresses, abducts, and medially rotates the eyeball |
| Inferior Oblique | Oculomotor nerve (CN III) | Elevates, abducts, and laterally rotates the eyeball |
| Levator Palpebrae Superioris | Oculomotor nerve (CN III) | Elevates the upper eyelid |
 | ||
| ![[Note Pyramidal System-20240426004827251.webp | 292]] |
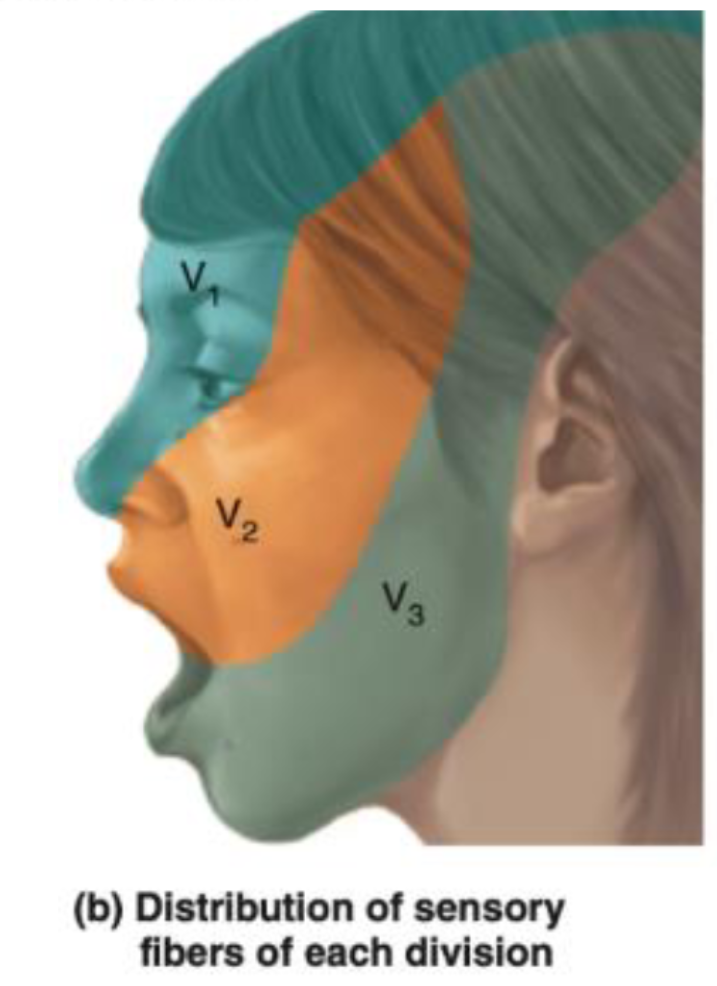
CN V – Trigeminal Nerve
-
Ophthalmic (V1) - Passes through the superior orbital fissure.
- Supplies: Sensation to the forehead, upper eyelid, and cornea.
- Involved in the corneal reflex: The afferent limb (sensory input) of the corneal reflex is through the ophthalmic branch of the trigeminal nerve. The efferent limb (motor output, which closes the eye) is via the facial nerve (CN VII).
-
Maxillary (V2) - Passes through the foramen rotundum.
- Supplies: Sensation to the middle part of the face, cheek, upper lip, and upper teeth.
-
Mandibular (V3) - Passes through the foramen ovale.
- Supplies: Sensation to the lower part of the face, lower lip, and lower teeth. It also carries motor fibers to the muscles of mastication.
- The anterior two-thirds of the tongue receives general sensation (not taste) via the lingual nerve, a branch of the mandibular division.
- Taste from the anterior two-thirds of the tongue is carried by the chorda tympani nerve (a branch of the facial nerve, CN VII), not the trigeminal nerve.
Examination process
-
Sensory Testing:
- Cotton Test: Use a soft piece of cotton to lightly touch different areas of the face. This tests the sensory function of all three branches of the trigeminal nerve. The patient should have their eyes closed during the test to rely solely on their sensory perception. Specifically, test:
- The forehead, upper eyelids, and cornea (ophthalmic branch).
- The cheeks, upper jaw, and upper teeth (maxillary branch).
- The lower jaw, lower teeth, and part of the tongue for general sensation (mandibular branch).
- Cotton Test: Use a soft piece of cotton to lightly touch different areas of the face. This tests the sensory function of all three branches of the trigeminal nerve. The patient should have their eyes closed during the test to rely solely on their sensory perception. Specifically, test:
-
Motor Testing: power (Medial and Lateral pterygoid, temporalis, masseter)
- Mandibular Movements:
- Ask the patient to clench their jaw to test the muscles of mastication, assessing the motor function of the mandibular branch (V3).
- Have the patient open their mouth and then move their jaw side to side, observing for any deviations or difficulties, which might indicate an issue with trigeminal motor function or asymmetrical muscle weakness.
- Mandibular Movements:
buccinator supplied by facial
-
Reflex: Jaw Reflex (afferent efferent) - Pure reflex Gently tap the jaw with the mouth slightly open to check the reflex. A normal response would be a slight and quick involuntary clenching of the jaw. An exaggerated response might suggest abnormalities in the reflex arc, which is primarily controlled by the sensory and motor roots of the mandibular branch.
Corneal reflex (Afferent Opthalmic - efferent by facial)
CN VII - Facial Nerve
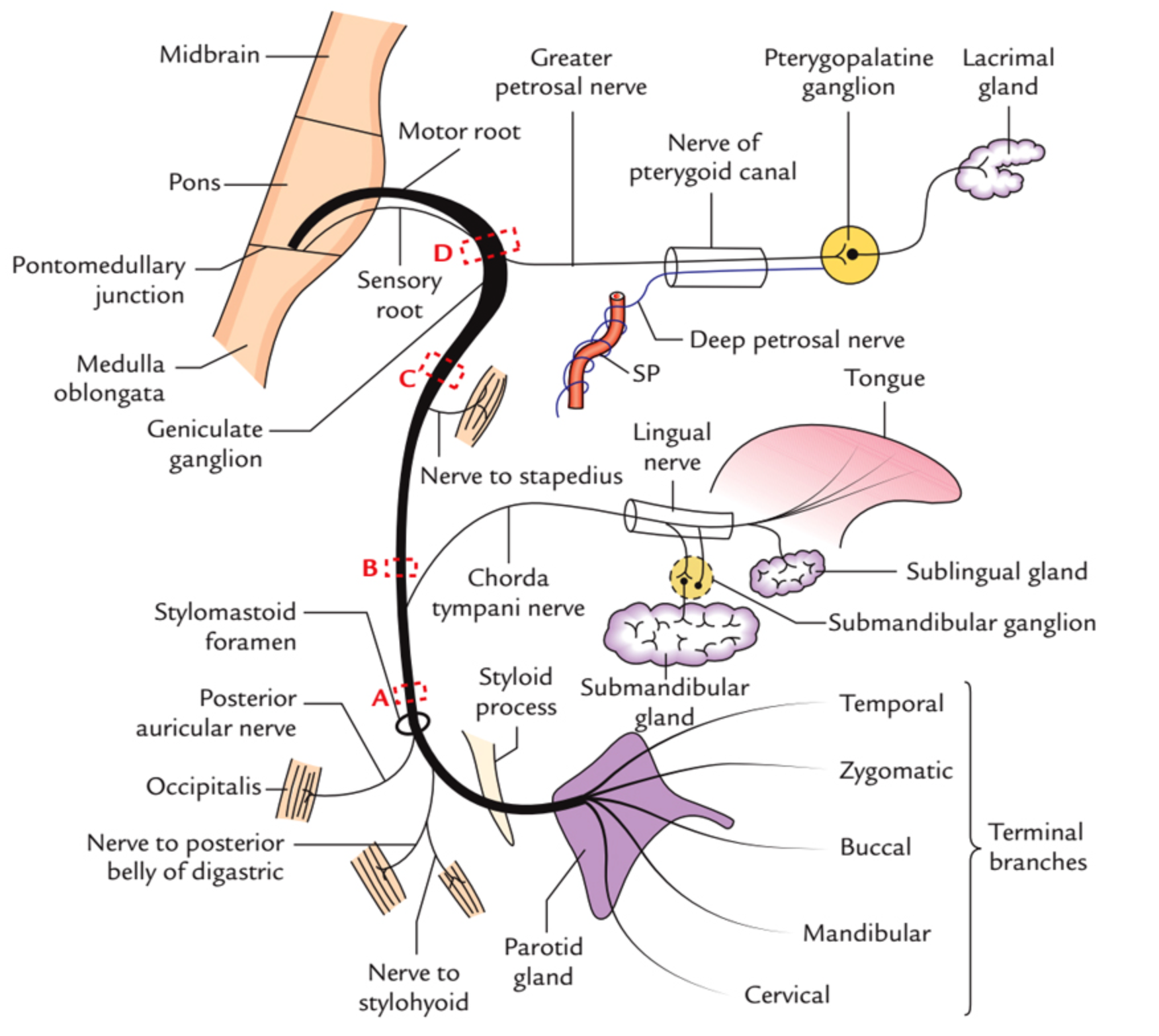 Course???
Course???
in middle ear gives two branches to chorda tympani & Stapedius (ear distrubance)
Innervations - External acoustic meatus - for sensation of ear - Motor - Movement of the face - Sternomastoid - branches nerve to stapedius - Loud sounds middle ear - & nerve to chorda tympani - Parasympathatic Submandibular & Sublingual gland
Tests
- Temporalis - raise eye brows (dont use hands )
- Orbicularis Oculi - check for resistance when eyes close
- Buccinator - Blow (palpate)
- Levator Anguli Superioris - smile
- Orbicularis Oris - whistle
- Taste anterior 2/3
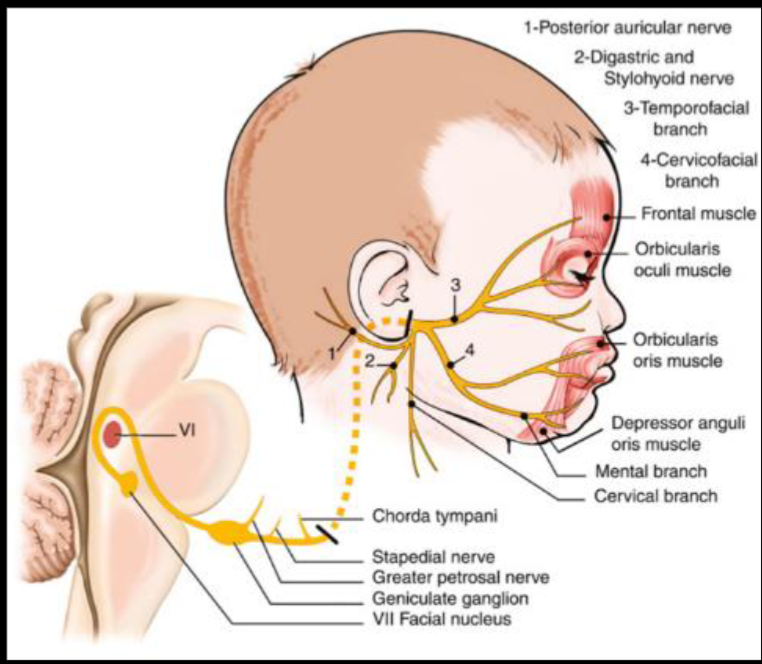 UMN Palsy - Causes Includes; (hyperreflexia)
- stroke
- MS
- trumours
- Internal capsule palsy
- Eyebrow raise is normal - if botox, contraindicated for the test
UMN Palsy - Causes Includes; (hyperreflexia)
- stroke
- MS
- trumours
- Internal capsule palsy
- Eyebrow raise is normal - if botox, contraindicated for the test
LMN Palsy - Causes includes
- Bells palsy
- Cavernous sinus thrombosis
- Fracture (truama) base of skull
- Acoustic neuroma
- Shingles
- Ramsay Hunt Syndrome with skin lesioned shingles on face and ear due to varicella ,
- Eyebrow doesn’t raise compared to contra-lateral
Bilateral facial nerve palsy - Sarcoidosis - Guillain-Barré Syndrome - Lyme disease
other notes botox mask symptoms of UMNL of facial nerve
most common causes of stroke? DVT - Stroke may transfer DVT to brain ASD - ventricular - patent foramin ovale
CN VIII - Vestibulocochlear
internal acoustic meatus enters to the skull depolization through potassium -
Cochlear division;
-
Whisper on ear while other is closed - tell him to repeat to confirm.
-
Rinne Test:
- This test compares air conduction to bone conduction. A tuning fork is used initially to assess bone conduction by placing it on the mastoid process. It is then held near the ear canal to assess air conduction.
- A positive Rinne test (air conduction is better than bone conduction) indicates normal hearing or sensorineural hearing loss.
- A negative Rinne test (bone conduction is better than or equal to air conduction) suggests conductive hearing loss.
-
Weber Test:
- This test assesses bone conduction using a tuning fork, which is placed on the center of the forehead.
- The purpose is to determine the lateralization of sound. Sound lateralization to one ear typically indicates sensorineural hearing loss in the opposite ear or conductive hearing loss in the ear to which sound is lateralized.
sensorineural causes - Neurofibromatosis type 2 - Noise pollution - Aminoglycosiedes - Gentamycin - Test, with ringing on frontal head - check for which ear hears most = laterilzation of normal side - Pendred Syndrome = Goiter + hearing loss (thyroid manifestations are rare, but may be presentaiton)
Conductive deafness - Wax / foreign objects - Otitis Media - - Tympanic membrane rupture - Otosclerosis. - Swimmers ear - Foreign body
Note
Fracture at the base of the skull can cause sensorineural hearing loss and bleeding, with lateralization. This is a result of conductive deafness, as the vestibulocochlear nerve passes through the petrous part of the temporal bone.
CN IX - Glossopharyngeal
Tests for Gag reflex Jugular foramen - Upper motor neuron palsy - glossopharyngeal special sense, pain and temperature autonomic to the parotid
examination by gag reflex with Glossopharyngeal & Vagus open mouth check uvula for Vagus for the tongue Hypoglossal
Main Causes - Neuralgias - Compression - Surgical
CN X - VAGUS
Cough, Gag reflex -
UML pseudobulbar palsy, - hot potato speech
bulbur palsy; LML - appear as nasal speech
9,10,11,12 bulbar palsy - by speech
CN XI - Accessory
-shrug, head switch
XII - Hypoglossal
-
All intrinsic and extrinsic muscles of tongue except palatoglossus by vagus
-
UML - Pseudobulbar palsy; Hot potato; Spastic
-
LML Bulbar Palsy; Nasal speech, appear as Fasucilation; Flaccid
-
Tongue goes to the side which is damaged
-
then check power of intrisic muscles of the tongue
B- Rheumatoid Arthritis Examination
https://www.youtube.com/watch?v=GhQVp_xdGVA
Scenario: A young female patient presents with symptoms suggestive of Rheumatoid Arthritis (RA).
- Anti-TNF-α: Infliximab (screen for latent TB and opportunistic infections before starting; consider interferon-gamma release assay). Adalimumab is another anti-TNF agent.
- Anti-IL1: Other agents in this group include anakinra, canakinumab, and rilonacept.
Notes:
- Rifampicin can cause discoloration and affects RNA synthesis.
- Jones criteria are used for the diagnosis of rheumatic fever, not RA.
Investigations
- Complete Blood Count (CBC)
- Erythrocyte Sedimentation Rate (ESR)
- C-Reactive Protein (CRP)
- Joint X-ray
Pathophysiology (5 points)
- Synovial inflammation and proliferation
- Soft tissue swelling
- Narrowing of joint spaces
- Bone erosion
- Deformity and functional impairment
Characteristic Features:
- Migratory polyarthritis
- Primarily affects small joints of the hands, especially the proximal interphalangeal (PIP) joints, but spares the distal interphalangeal (DIP) joints.
- Rheumatoid factor (RF) is often positive but may be negative in early disease.
Differential Diagnosis
- Psoriatic arthritis (may precede skin manifestations by 10 years; differentiate with X-ray)
- Systemic Lupus Erythematosus (SLE)
- Reactive arthritis (formerly known as Reiter’s syndrome; often follows an infection)
- Osteoarthritis (more common in older individuals; can occur in younger individuals with repetitive joint use, e.g., piano players)
Initial Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids (oral or intra-articular injections to control flares)
Approach to Examination
- Be mindful of patient comfort: Offer a pillow for support and avoid shaking hands if the patient is experiencing joint pain.
- Mnemonic (DAF):
- Deformity: Inspect the hands systematically, moving from medial to lateral and distal to proximal.
- Ulnar deviation
- Swan neck deformity (hyperextension of PIP joint, flexion of DIP joint)
- Boutonniere deformity (flexion of PIP joint, extension of DIP joint)
- Z deformity of the thumb
- Guttering (loss of muscle bulk between metacarpals, tendor clear)
- Palmar erythema; Thenar eminence atrophy
- Scars from previous surgeries or joint injections
- Rheumatoid nodules
- psoriatic rash same as RA
- Activity: Assess disease activity (e.g., presence of flares, joint tenderness, swelling, warmth, tighness). four t’s and one s - if patient has frequent flares we give steroids - will break down collagen/ellastin - become like paper ++ cushing - sometimes skin is tight glued to the skin - systemic scleroderma - mixed connective tissue disease
- Gently palpate the joints for tenderness,
- swelling (RING TEST),
- tapping and
- warmth/temp (from forearm, distal, forarm, phalanges.), avoid affected joints
- Function of hand: Evaluate hand function (e.g., grip strength, ability to perform fine motor tasks). - special tests
- Thumb opposition: Ask the patient to touch the tip of their thumb to the tip of each finger. Z TASBEEH
- OK SIGN median nerve compensation
- COIN TEST; pencil grip - abnormal with compensation due deformities
- Phalen’s test and Tinel’s sign: to assess carpal tunnel syndrome (median nerve compression) dorsum to dorsum dorsal to dorsal arm - results in parathesia - dont do it if he has this previous symptom
- Deformity: Inspect the hands systematically, moving from medial to lateral and distal to proximal.
tapping; parathesia around distribution of hand (induce pain, never do in exam) (do you feel pain when you tap here before?)
Ask patient consent before going his back for interscapular pad of fat for cushing
Systemic Examination
-
General inspection: Look for signs of:
-
Jaundice (scleral icterus)
-
Pallor (conjunctivae); due Anemia, hemolytic anemia, methotrexate folate defieciency; megaloblastic anemia
-
Butterfly rash (malar rash characteristic of SLE)
-
Round face (Cushing’s syndrome) - interscapular cushing pad, previous surgery scar antoatlial sublaxation (spastic paraperesis in lower limb)
-
Smooth tongue (iron deficiency anemia or oral candidiasis; inhaled corticosteroids)
-
Peripheral edema (pitting edema in the lower extremities)
-
-
Cardiovascular: Auscultate for murmurs and signs of pulmonary hypertension (e.g., loud P2).
-
Respiratory: Auscultate the lungs for crepitations/Fine Crackles (suggestive of interstitial lung disease).
-
Gastrointestinal: Palpate the abdomen for hepatomegaly (liver enlargement).
-
Musculoskeletal: Examine other joints for signs of arthritis (e.g., knees, ankles).
Potential Complications and Considerations for General Examination
- Anemia: Can be caused by iron deficiency (due to gastrointestinal blood loss from NSAID use), chronic disease, or autoimmune hemolytic anemia (Jaundice * & Methotrexate & Autoimmune hepatitis due nature of autoimmunity) - could be also due gastric ulceration loss of blood +++ B12 deficiency anemia; depleted folate
- Methotrexate toxicity: Monitor liver function tests and complete blood counts.
- Infection: Increased risk due to immunosuppressive medications.
- Scleritis and episcleritis: Inflammation of the eye.
- Cushing’s syndrome: Due to prolonged corticosteroid use resulting in PROXIMAL MYOPATHY.
- Osteoporosis: Due to chronic inflammation and corticosteroid use.
- Cardiovascular disease: Increased risk in patients with RA.
- Amyloidosis: Can lead to nephrotic syndrome.
- Analgesic nephropathy: Chronic kidney disease due to long-term NSAID use.
fletus syndrome; development of spleenomegaly due RA - destroyed RBCs resulting Anemia
Further Investigations (if indicated)
- Renal function tests
- Liver function tests
- Serum creatinine
- Urinalysis
- Chest X-ray (Multiple nodules in periphery of the lung - looks like rheumatoid - bilateral homogenous circumscribed nodules; most like pneuomocoisosis; coal worker; caplan syndrome, and RA)
- Echocardiogram
psoaritic rash can be find behind the eye + sublixation + elbow الصدفيه loud s2
Examination of a Patient Potentially with Rheumatoid Arthritis and Complications
Cardiovascular:
- 2nd LT ICS - Loud S2: This finding suggests pulmonary hypertension. Pulmonary hypertension can be a primary condition or secondary to another underlying issue, such as interstitial lung disease (a potential complication of rheumatoid arthritis).
- Right sided HF = pulmonary HTN - Edema - associated with Hepatomegaly (Methotrexate)
Abdomen:
- Hepatomegaly: Enlarged liver. Several potential causes are listed, reflecting the complexity of this patient’s case:
- Methotrexate: A common medication for RA, it can cause liver toxicity.
- Right-sided Heart Failure: Pulmonary hypertension can lead to right-sided heart failure, causing congestion in the liver.
- Autoimmune Hepatitis: RA is an autoimmune disease, and other autoimmune conditions, like autoimmune hepatitis, can co-occur.
Fever:
- Azathioprine-induced Neutropenia: Azathioprine, another immunosuppressant used in RA treatment, can cause neutropenia (low neutrophil count), increasing the risk of infection and fever.
Felty’s Syndrome:
- Splenomegaly, Pancytopenia, Pallor: Felty’s syndrome is a rare complication of long-standing RA characterized by an enlarged spleen, decreased red blood cells, neutrophils, and platelets. The reduced red blood cell count can result in pallor, which might be visible on eye examination.
Renal:
- Amyloidosis: Amyloidosis is a rare but serious complication of chronic inflammatory diseases like RA. It can lead to nephrotic syndrome, characterized by proteinuria and edema. Ballottement of the kidney may be a sign of an enlarged kidney due to amyloid deposits.
- NSAID-induced Nephropathy: Long-term use of NSAIDs for pain relief can contribute to kidney damage (analgesic nephropathy), especially in patients with pre-existing renal issues.
Musculoskeletal:
- Joint Crepitus (Knee): Crepitus is a grating or crackling sound or sensation in a joint, often associated with arthritis. Further examination, including range of motion assessment (e.g., flexion), is needed.
Lower Limbs:
- Edema: Swelling, likely in the lower extremities, suggesting right-sided heart failure secondary to pulmonary hypertension. + amyloidosis
Endocrine:
-
Suspected Cushing’s Syndrome: The notes suggest concern about possible Cushing’s syndrome, likely due to the patient’s clinical presentation or long-term steroid use for RA.
- Dexamethasone Suppression Test:
-
Low-dose: This is the initial screening test to confirm elevated cortisol levels.
-
High-dose: If the low-dose test is abnormal, a high-dose test can help differentiate between Cushing’s disease (pituitary tumor causing excess ACTH) and other causes of Cushing’s syndrome (e.g., adrenal tumor, ectopic ACTH production).
-
-
24-Hour Urinary Free Cortisol Test
-
Late-Night Salivary Cortisol Test
- Dexamethasone Suppression Test:
-
Differential Diagnosis: The differential diagnosis for elevated cortisol includes Cushing’s syndrome, pseudo-Cushing’s syndrome (often seen in conditions like alcoholism or depression), and exogenous steroid use.
Further Investigations:
This patient requires further investigations to confirm the diagnoses and assess the severity of their conditions. This may include:
- X-ray of joint - most importantly
- Echocardiogram: To assess the severity of pulmonary hypertension and right heart function.
- Pulmonary Function Tests: To evaluate lung function and identify any underlying lung disease.
- Liver Function Tests: To assess liver health and monitor for methotrexate toxicity.
- Kidney Biopsy: To confirm amyloidosis and assess the extent of kidney damage.
- Imaging (e.g., CT/MRI): To evaluate the spleen, liver, kidneys, and adrenal glands.
- Autoantibody Testing: To look for specific autoantibodies associated with autoimmune hepatitis and other autoimmune conditions.
Treatment
DMARDS - corticosteroid as bridging treatment
Disease-Modifying Antirheumatic Drugs (DMARDs)
- Methotrexate
- Azathioprine (Isiosyprine is likely a typo); inhibit synthesis of purine - adverse; neutropenia
- Hydroxychloroquine; adverse; retinal deposits
- Gold compounds; nephrotic, skin pigmentation, encephalitis,
- Leflunomide; pyrimidiine synthesis inhibitor - only for RA - results in tachycardia.
Treatment Strategy:
- Corticosteroids + Methotrexate for 6 months initially. ??? CC
- If acute disease persists, consider adding a biologic agent (e.g., anti-TNF-A (Infliximab & another mab) or anti-IL1).
- If no response to DMARDs, administer biological agents (antibodies, cytokines).
Screen TB before giving ANTI-TNF-A medications
other notes? etanrecept - sodium + receptor
immunosuppresant Sulfanaizizine???? - IBD - saliciylte + sulpha
- low dose dexamehtasone supression test -
- in order diagnose cushing
- overnight to proove increased cortisol
high dose? - alcohol, stress, …
alcoholic, cushing,
- auscultate lung from back (methotrexate cause basal crepititation intestinsal lung disease - Risk factor also for RA) scapular syndrome chest x-ray
C- Chest auscultation
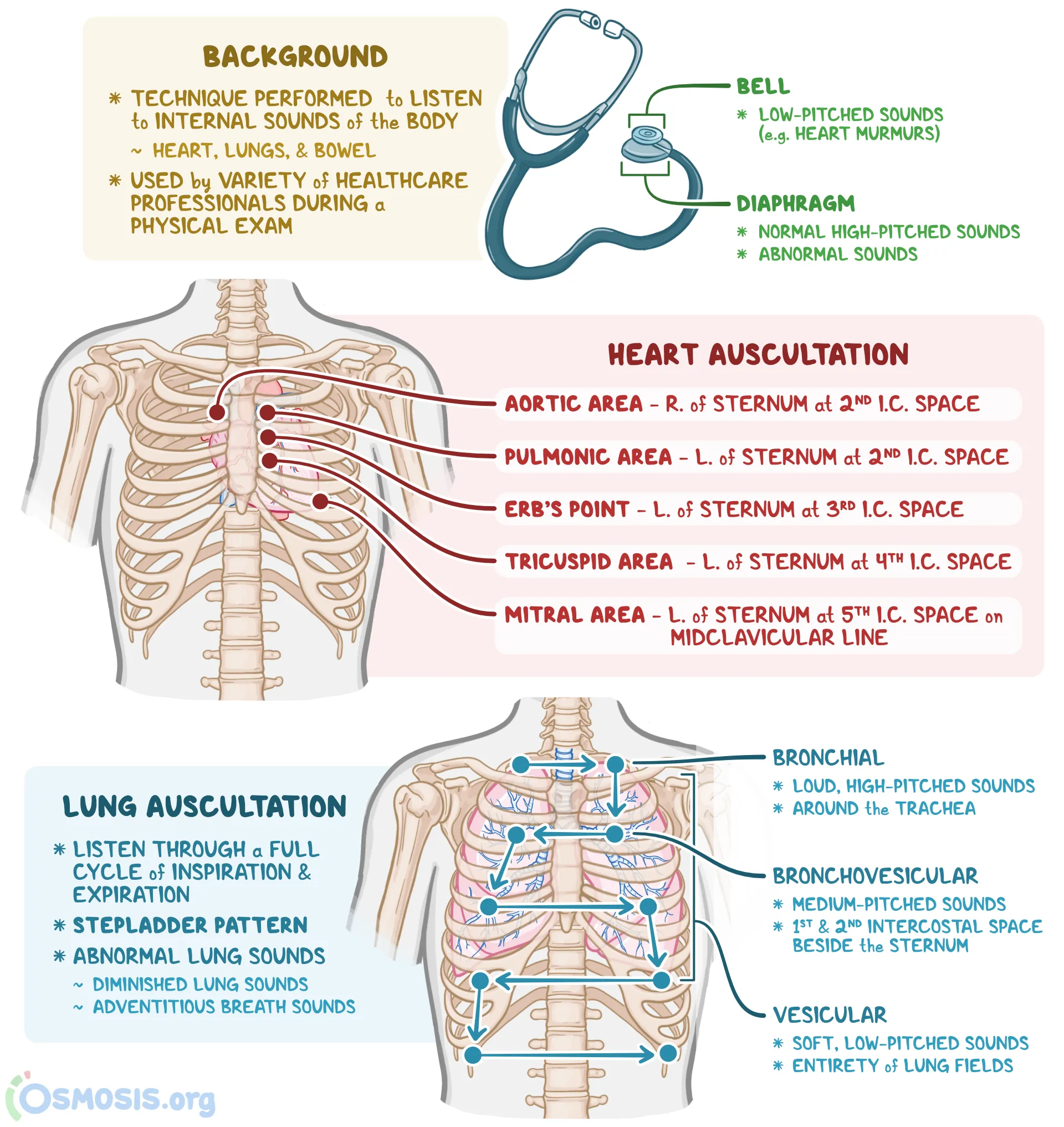
CVS
introduce your self, explain the procedure, take consent, position and exposure make sure to remove clothing, avoid snake stethoscope
https://www.youtube.com/watch?v=gRWSyqatWQQ&t=156s Auscultate all areas starting from mitral - both diaphragm and bell - then auscultate Carotid & Axilla - sync with radial while auscultating
Heart Sounds
S1 -(Systolic)- S2 —> (Diastolic) —> S3,S4 —> S1 heard after S1 is systolic, after S2 is diastolic
Systole Murmur - aorta open Valvular stenosis
- Aortic stenosis
- crescendo-decrescendo
- heard best over the aortic area and often radiating to the carotids.
Diastolic Murmur -
-
Mitral stenosis - characterized by a mid-diastolic rumbling murmur, best heard at the apex with the patient in the left lateral decubitus position.
-
Aortic Regurgitation and Tricuspid Stenosis: Aortic regurgitation typically results in a “blowing” early diastolic murmur heard best along the left sternal border.
-
left atrial myxoma & tricuspid
Opening snap; indicating leaflet is still moving and is still not calcified
Radiation
-
Aortic stenosis; Typically causes a systolic murmur that can radiate to the carotid arteries. The presence of aortic calcification, which can be associated with aortic stenosis, does not necessarily cause pain but can contribute to the severity of the stenosis detectable via imaging or echocardiography.
-
Mitral regurgitation; have pansystolic murmur that radiates to the axilla. The murmur starts with S1 and extends up to S2, indicating the backward flow of blood from the left ventricle to the left atrium throughout systole.
Sound Differentiation
- Tricuspid Regurgitation - swoosh dub murmur - RT. V. Hypertrophy
- Mitral Stenosis - LUB dub -
| Systolic Murmurs | Diastolic Murmurs/Sounds |
|---|---|
| AS = aortic stenosis | AR = aortic regurgitation |
| MR = mitral regurgitation | MS = mitral stenosis |
| HCM = hypertrophic cardiomyopathy | S3 = third heart sound |
| PS = pulmonary stenosis | PR = pulmonary regurgitation |
| VSD = ventricular septal defect | PDA = patent ductus arteriosus (continuous murmur) |
| I = innocent murmur | - |
Localization of Heart Sounds
Mitral Stenosis: This condition is best evaluated by listening over the mitral area, which is generally found over the apex of the heart, toward the left side of the chest.
Austin Flint Murmur of Aortic Regurgitation: S1 (first heart sound) is typically best heard in the aortic area, which is the right second intercostal space near the sternum. It is best felt in the pulmonary area, which refers to the left second intercostal space adjacent to the sternum.
Tricuspid Stenosis: This is best heard over the tricuspid area, located at the lower left sternal border of the chest.
Left Atrial Myxoma: Suspected when a tumor in the left atrium causes a sound, which can often be best detected near the heart’s apex.
Diastolic Murmurs: These murmurs are generally quiet and can be challenging to hear. It is advisable for the patient to sit forward and hold their breath after exhaling to enhance the audibility of these murmurs.
RESP
introduce your self, explain the procedure, take consent, position and exposure make sure to remove clothing, avoid snake stethoscope
-
To assess breath sounds, ask the patient to breathe in and out slowly and deeply through the mouth.
-
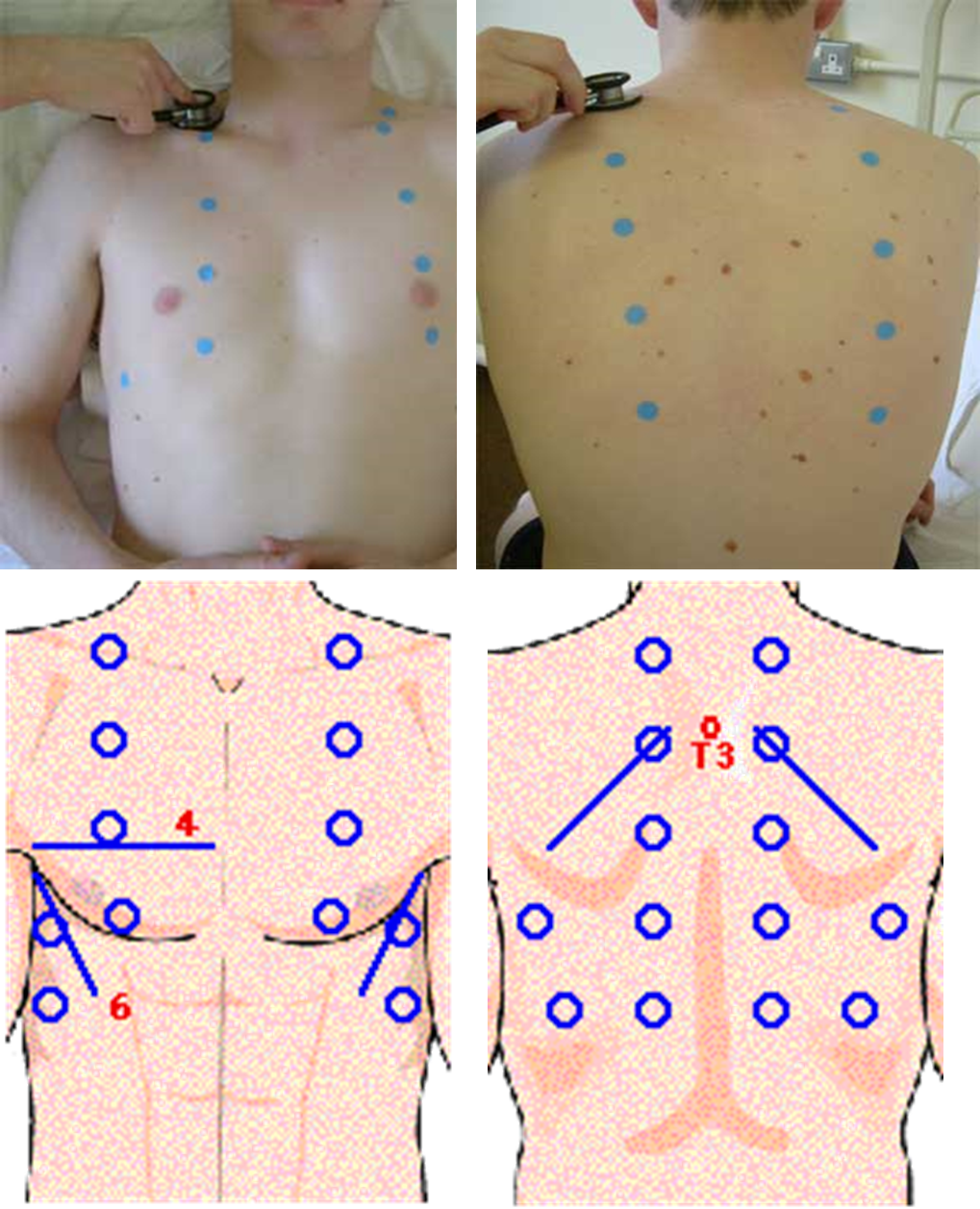
Begin at the apex of each lung and zigzag downward between intercostal spaces. Listen with the diaphragm portion of the stethoscope.
Process
- Using the diaphragm of a stethoscope & comment on the following:
- Breath sounds (BS)
- Intensity: Normal or ↓ as in (consolidation, collapse, pleural effusion, pneumothorax, lung fibrosis)
- Quality: Vesicular or bronchial
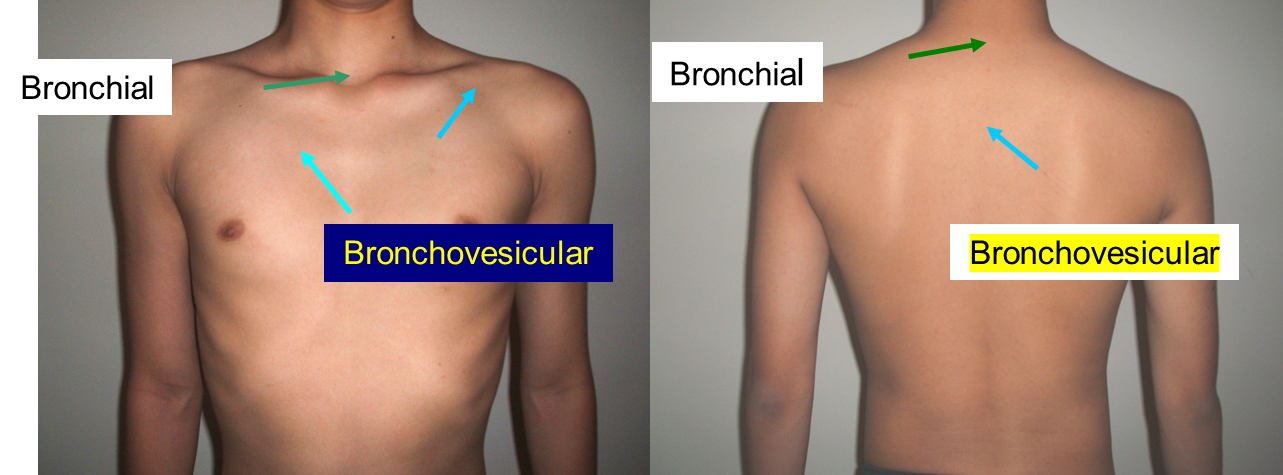
- Differentiation between vesicular & bronchial
- Vesicular: louder & longer on inspiration & has no gap between the 2 phases
- Bronchial: louder & longer on expiratory & has a gap between the 2 phases
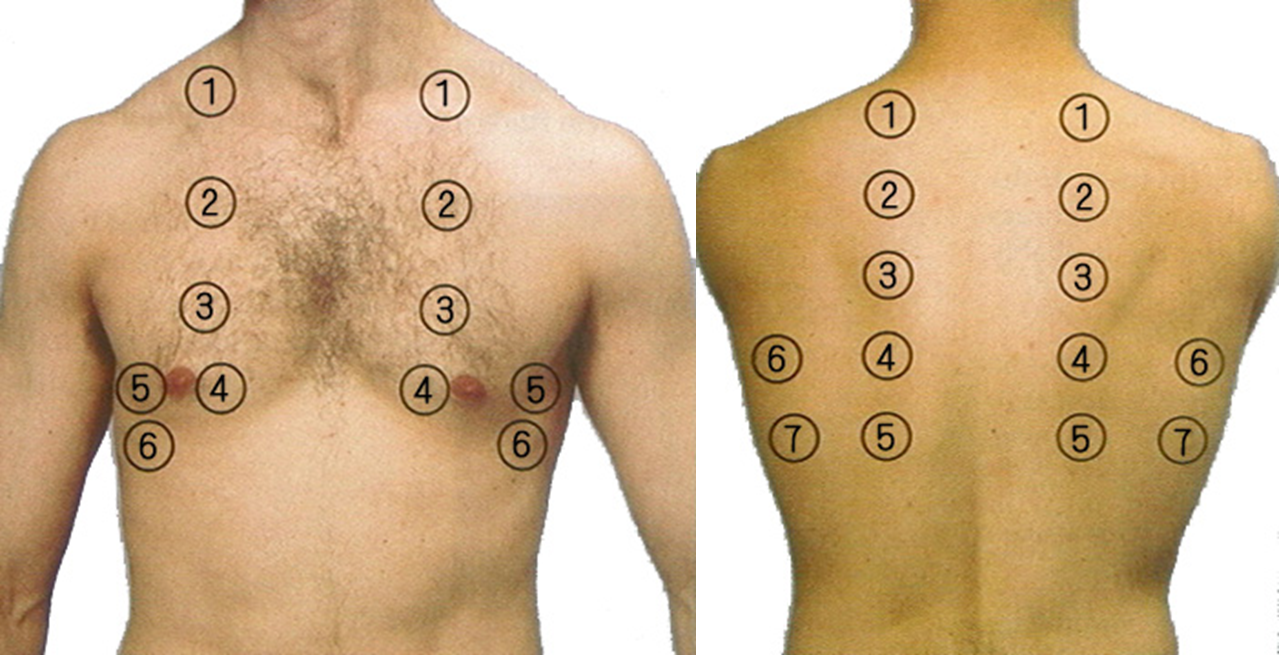
Order of auscultation
Breath sound
| Sound | Description | Common Causes |
|---|---|---|
| Vesicular | Soft, low-pitched, normal over most lung fields | Normal lung function |
| Bronchial | Loud, high-pitched, normal over trachea - Larynx, suprasternal fossa, around 6th, 7th cervical vertebra, 1st, 2nd thoracic vertebra | Normal over trachea, abnormal if heard elsewhere |
| Bronchovesicular | Intermediate pitch, normal near sternum/scapulae 1st, 2nd intercostal space beside of sternum, the level of 3rd, 4th thoracic vertebra in interscaplar area, apex of lung | Normal lung function |
| Crackles (Rales) | Discontinuous, popping sounds (fine or coarse) | Pneumonia, heart failure, fibrosis, bronchiectasis |
| Wheezes | Continuous, high-pitched, musical | Asthma, COPD, bronchitis, airway obstruction |
| Rhonchi | Low-pitched, snoring or gurgling | Chronic bronchitis, pneumonia, cystic fibrosis |
| Stridor | High-pitched, harsh, inspiratory sound | Upper airway obstruction (croup, epiglottitis, tumor) |
| Pleural Rub | Creaking or grating sound | Pleuritis, pulmonary embolism, pneumonia |
| Absent/Diminished | Reduced or absent breath sounds | Pneumothorax, pleural effusion, atelectasis |
| Egophony | ”E” sounds like “A” | Lung consolidation (pneumonia) |
| Bronchophony | Increased clarity of spoken words | Lung consolidation (pneumonia) |
| Whispered Pectoriloquy | Increased clarity of whispered words | Lung consolidation (pneumonia) |
Station Procedure Lumbar Puncture
Lumbar Puncture CSF fluid
Prerequisites
- Obtain a thorough medical history, paying attention to bleeding tendencies, atrial fibrillation, and anticoagulant use (e.g., warfarin).
- Perform a CT scan if a space-occupying lesion (SOL) is suspected.
- Obtain informed consent from the patient.
Contraindications
- Space-Occupying Lesion (SOL): Risk of tonsillar herniation.
- Bleeding Disorders: Conditions such as hemophilia.
- Anticoagulant Use: Patients on anticoagulants (e.g., warfarin).
- Thrombocytopenia: Low platelet count.
- Vertebral Abscess: Risk of infection.
- Spinal Deformities: Conditions like scoliosis; consider ultrasound guidance.
- Phenytoin Use: Risk of spina bifida.
Diagnostic Indications
- Meningitis: Lumbar puncture is used to diagnose infections like bacterial, viral, or tuberculous meningitis.
- Encephalitis
- Neurosyphilis
- MS , GBS
- Subarachnoid Hemorrhage
- Carcinomatous Meningitis
- Monitoring Hydrocephalus
Other Therapeutic Uses
- Antibiotic Administration
- Anesthesia (e.g., spinal anesthesia)
Complications
- Headache (most common)
- Epidural or subarachnoid hematoma
- Spinal cord trauma
- Infection
- Back pain (most common)
- Hypotension, bradycardia.
Risk Factors
- Papilledema: Risk of blindness due to idiopathic intracranial hypertension if not properly managed.
Position The preferred position is lying on their side (left lateral) with the patient’s legs flexed at the knee and pulled in towards their chest, and upper thorax curved forward in an almost fetal position.
The second position is the upright or sitting position. Sit the patient on the edge of bed, with their legs resting on a stool or chair, ask them to roll their shoulders and upper back forwards and the chair is positioned to bring the thighs up towards the abdomen. Full Procedure introduce yourself, explain procedure, take consent, wear sterile gloves, exposure and position - ready equipment (LP Tray)
-
Feel the pelvis after position - iliac crest will pass by L4 - then trace your fingers downwards by one process for L3. then mark it -
-
Start sanitizing the area three times from Inside to outside best circular motion - start centrally then peripherally
-
use sterile paper drape after sanitizing the whole back - centrally to the mark
-
Anesthesia: Apply lidocaine for local anesthesia Inject Subcutaneous (30 degree) anaesthetics (lidocaine) to the area. Avoid lidocaine in patients with liver cirrhosis; consider using ether-based anesthetics in such cases (Isoflurane, desflurane, and sevoflurane)
-
Needle Insertion: with spinal needle Insert the needle between the marked L3-L4 at 15 degree from 90 degree angle until pop is felt. dont pull puncture until its fully secured to prevent complications
-
Sample Collection: Collect 4 samples for:
- Chemistry
- Cytology
- Microbiology
- fourth-fifth just incase for other labs
LP Tray includes
- Spinal needle
- Three-way stopcock
- Manometer
- specimen tubes
- Local anesthesia such as: Xylocaine /lidocaine 1%
- Betadine: (Povidone-iodine) solution & sponge wand.
- Drapes, gauze, and bandage
Note Subarachnoid Hemorrhage: If the sample is red, it may indicate a subarachnoid hemorrhage.
Look for xanthochromia (yellow discoloration) in the CSF.
Post-Procedure Counseling
- Advise the patient to rest on their back and drink coffee to help prevent post-LP headaches.
- If a severe headache occurs, consider performing a blood patch to equalize CSF pressure.
How to minimize the headache?
- choice of needle standerd Quinck versus atraumatic .
- decrease the number of attempts.
- reinsersion of the stylet.
- bed rest after the procedure.
CSF Analysis
| Parameter | Bacterial Meningitis | Tuberculous (TB) Meningitis | Viral (Aseptic) Meningitis |
|---|---|---|---|
| Appearance | Turbid, cloudy | Slightly turbid or clear | Clear |
| Opening Pressure | Elevated (200-500 mm H₂O) | Elevated (200-300 mm H₂O) | Normal or slightly elevated |
| White Blood Cell (WBC) Count | Elevated (1,000-5,000 cells/µL) | Elevated (100-500 cells/µL) | Elevated (10-500 cells/µL) |
| WBC Differential | Predominantly neutrophils (PMNs) | Predominantly lymphocytes | Predominantly lymphocytes |
| Protein | Elevated (100-500 mg/dL) | Elevated (100-300 mg/dL) | Mildly elevated (50-100 mg/dL) |
| Glucose | Decreased (<40 mg/dL or <40% of serum) | Decreased (<45 mg/dL or <40% of serum) | Normal or slightly decreased (>45 mg/dL) |
| CSF/Serum Glucose Ratio | Low (<0.4) | Low (<0.4) | Normal (>0.6) |
| Lactate | Elevated (>3.5 mmol/L) | Elevated (2.5-4 mmol/L) | Normal (<2 mmol/L) |
| Culture | Positive for bacterial pathogens | Positive for Mycobacterium tuberculosis | Negative |
https://medatlax.com/Clinical/Level-8/Skill/Topics/Lumbar-Puncture/Lumbar-Puncture
https://medatlax.com/Clinical/Level-8/Skill/Topics/Lumbar-Puncture/Lumbar-Puncture-Procedure
Station Counseling
Case 1: - Post Mi Counseling
introduce your self, what you do, explain about their situation. take Hx necessary for effective counseling
Introduction:
- Begin by discussing the patient’s current situation. Ask if they recall any events or symptoms leading up to the episode. Specifically, inquire if they experienced unconsciousness or any other significant symptoms before the MI.
Diagnosis and Management:
- Explain that the patient has been diagnosed with a myocardial infarction (heart attack) and that appropriate management has been initiated.
- Ask the patient if they understand their diagnosis and provide a brief explanation of the condition, including: - Pathophysiology - Risk factors (e.g., smoking, high blood pressure, high cholesterol, diabetes). - Symptoms (e.g., chest pain, shortness of breath, fatigue). - Protective factors (e.g., lifestyle changes, medications). - Effect of medications (e.g., aspirin, beta-blockers, statins) and how they help prevent future episodes.
History and Lifestyle:
- Take a detailed history, including:
- Medication use (e.g., aspirin).
- Smoking history (e.g., 1 pack per day for 15 years, attempts to quit).
- Exercise
- Travel
- Discuss the importance of lifestyle changes, such as smoking cessation, diet, and exercise.
Activity and Restrictions: Discuss the patient’s ability to return to normal activities, including:
- Driving: No driving for 2 weeks, and if the patient is a large veichle driver, they should avoid driving for 6 weeks.
- Travel: Delay travel for 1 week post-PCI (Percutaneous Coronary Intervention) with stent placement.
- Exercise: Encourage light exercise, such as going to the gym, but advise avoiding excessive strain.
- Thrombolytic therapy: If applicable, explain that they should avoid strenuous activities for 2 weeks after receiving thrombolytic therapy such as contact sport.
Follow-Up and Monitoring:
- Schedule follow-up appointments for screening and management of conditions such as diabetes (DM) and hypertension (HTN).
- Provide written instructions for the patient to refer to later.
Questions and Patient Understanding:
- Throughout the conversation, ensure that the patient understands the information being provided. Establish clear communication and ask if they have any questions on every point you go over
- Reassure the patient that they may need to take time off work (three weeks to one month) and discuss any concerns they may have about their job or recovery.
Conclusion:
- Provide the patient with a leaflet summarizing the key points discussed, including lifestyle changes, medication instructions, and follow-up care.
- Ask if they have any final questions or concerns before concluding the session and thank the patient
Case 2: - Post-HIV Diagnosis Counseling
Introduction:
- Begin by creating a supportive and non-judgmental environment. Acknowledge that receiving an HIV diagnosis can be overwhelming and that you are here to provide information, support, and guidance.
- Ask the patient how they are feeling and if they have any immediate concerns or questions about their diagnosis.
Diagnosis and Understanding HIV:
- Explain the diagnosis clearly and ensure the patient understands what HIV is:
- HIV (Human Immunodeficiency Virus) is a virus that attacks the immune system, specifically the CD4 cells (T cells), which are crucial for fighting infections.
- Without treatment, HIV can lead to AIDS (Acquired Immunodeficiency Syndrome), the final stage of HIV infection, where the immune system is severely compromised.
- Reassure the patient that HIV is a manageable chronic condition with proper treatment and care.
- Discuss the importance of early treatment and how modern antiretroviral therapy (ART) can help them live a long, healthy life.
Transmission and Prevention:
- Explain how HIV is transmitted (e.g., through unprotected sex, sharing needles, from mother to child during childbirth or breastfeeding) and how it is not transmitted (e.g., through casual contact, hugging, sharing food).
- Discuss prevention strategies to avoid transmitting the virus to others
Treatment and Management:
- Introduce the concept of antiretroviral therapy (ART):
- ART is a combination of medications that help control the virus and prevent it from replicating.
- Emphasize the importance of adherence to the medication regimen to maintain a low viral load and prevent drug resistance.
- Explain that ART can help the patient achieve an undetectable viral load, which significantly reduces the risk of transmission and helps maintain a healthy immune system.
- Discuss potential side effects of ART and reassure the patient that most side effects are manageable and that their healthcare team will work with them to find the best treatment plan.
Monitoring and Follow-Up:
- Explain the importance of regular follow-up appointments to monitor their health:
- CD4 count: To assess the strength of their immune system.
- Viral load: To ensure the virus is well-controlled.
- Screening for other infections: Such as tuberculosis, hepatitis, and sexually transmitted infections (STIs).
- Encourage the patient to maintain a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking or excessive alcohol use.
Disclosure and Support:
- Discuss the sensitive topic of disclosure:
- Explain that they are not legally required to disclose their HIV status to everyone, but they should inform sexual partners and healthcare providers.
- Offer guidance on how to have these conversations and provide resources for support.
- Encourage the patient to seek emotional support from trusted friends, family, or support groups. Offer information about local or online HIV support groups and counseling services.
- Reassure the patient that they are not alone and that there are many resources available to help them navigate life with HIV.
Lifestyle and Mental Health:
- Address the potential emotional and psychological impact of an HIV diagnosis:
- Acknowledge that it is normal to feel a range of emotions, including fear, anger, sadness, or confusion.
- Encourage the patient to seek mental health support if needed, such as counseling or therapy, to help them cope with their diagnosis.
- Discuss the importance of maintaining a positive outlook and focusing on their overall well-being.
Questions and Patient Understanding:
- Throughout the conversation, check in with the patient to ensure they understand the information being provided.
- Ask if they have any questions or concerns about their diagnosis, treatment, or lifestyle changes.
- Provide reassurance and emphasize that they can reach out to their healthcare team at any time for further support.
Conclusion:
- Provide the patient with written materials (e.g., leaflets or brochures) that summarize the key points discussed, including information on ART, transmission prevention, and support resources.
- Offer to schedule a follow-up appointment to discuss any additional concerns or to provide further education.
- End the session by asking if they have any final questions and reminding them that they are not alone in this journey.
warfarin
Warfarin and Anticoagulation Counseling
Introduction:
- Begin by explaining that the patient has been prescribed warfarin, a blood thinner (anticoagulant) used to prevent blood clots. Warfarin helps reduce the risk of conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), or stroke in patients with conditions such as atrial fibrillation or after certain surgeries.
Mechanism of Action:
- Anticoagulant that works by inhibiting the synthesis of vitamin K-dependent clotting factors in the liver. Specifically, it inhibits the enzyme vitamin K epoxide reductase (VKORC1), which is responsible for recycling vitamin K into its active form to prevent clotting
Dietary Considerations:
- Vegetarian Diet and Vitamin K:
- If the patient follows a vegetarian diet, explain that certain vegetables (especially leafy greens like spinach, kale, and broccoli) are high in vitamin K, which can reduce the effectiveness of warfarin.
- Advise the patient to maintain a consistent intake of vitamin K rather than avoiding it completely. Sudden changes in vitamin K intake can affect how warfarin works.
- If needed, provide a list of foods high in vitamin K and suggest they monitor their intake.
Exercise and Activity:
- Exercise Recommendations:
- Encourage the patient to stay active, but advise them to avoid contact sports or activities that could lead to injury, as warfarin increases the risk of internal bleeding.
- Low-impact exercises like walking, swimming, or cycling are generally safe, but they should avoid activities that could result in falls or trauma.
Medication Regimen:
- Warfarin and Heparin:
- Explain that warfarin takes a few days to reach its full effect. Therefore, the patient may be started on heparin (a fast-acting anticoagulant) for the first few days until warfarin becomes effective.
- Typically, heparin is given for 3-5 days, and once the INR (International Normalized Ratio) is within the target range, heparin can be stopped, and the patient will continue with warfarin alone.
Monitoring and Follow-Up:
- INR Monitoring:
- Warfarin requires regular blood tests to monitor the INR, which measures how long it takes for the blood to clot. The target INR range depends on the condition being treated (usually between 2.0 and 3.0 for most conditions).
- Initially, the patient may need to have their INR checked every 2-3 days until it stabilizes. Once stable, follow-up can be reduced to once every 3 weeks and eventually once per month.
- Emphasize the importance of attending these follow-up appointments to ensure the medication is working properly and to adjust the dose if necessary.
Medication Adherence:
- Taking Warfarin:
- Stress the importance of taking warfarin at the same time every day, preferably after a meal to reduce stomach upset.
- Missing doses or taking extra doses can lead to serious complications, such as bleeding or clotting.
- If the patient misses a dose, they should take it as soon as they remember, but never double up on doses. If they miss a dose for an entire day, they should contact their healthcare provider for advice.
Potential Side Effects and Warning Signs: Bleeding Risks:
- Explain that warfarin increases the risk of bleeding. The patient should watch for signs of excessive bleeding, such as:
- Unexplained bruising.
- Prolonged bleeding from cuts.
- Blood in urine or stool (black, tarry stools).
- Nosebleeds or bleeding gums.
- Severe headaches or dizziness (which could indicate internal bleeding).
- If they experience any of these symptoms, they should seek medical attention immediately.
Drug Interactions:
- Warfarin interacts with many medications, including over-the-counter drugs like aspirin, ibuprofen, and certain antibiotics. Always check with a healthcare provider before starting any new medications or supplements.
- Alcohol can also affect warfarin, so advise the patient to limit alcohol intake and avoid binge drinking.
Questions and Patient Understanding:
- Throughout the conversation, check in with the patient to ensure they understand the information being provided.
- Ask if they have any questions or concerns about their medication, diet, or lifestyle changes.
- Reassure the patient that they can always contact their healthcare provider if they have any doubts or experience any side effects.
Conclusion:
- Provide the patient with written materials summarizing the key points discussed, including dietary guidelines, medication instructions, and warning signs of complications.
- Remind the patient to take their medication every day and to attend all follow-up appointments for INR monitoring.
- Ask if they have any final questions and offer reassurance that with proper management, they can safely take warfarin to prevent blood clots.
Other cases?
Case 1
Find compromises without risking patients life when asked to cover shift - for example being in same hospital when complicated case appears or the student/resident doesnt know how to approach it etc.. be nice i guess
Case 2
Give blood to the child’s jehova witness and potentially go to jail after court
make sure to give signature first if denied just do it :)