Pediatrics
ACUTE PHARYNGITIS AND TONSILLOPHARYNGITIS (SORE THROAT)
-
Pharyngitis is redness, pain, and swelling of the throat (pharynx).
-
Tonsillitis is inflammation of the tonsils.
-
Children may have pharyngitis, tonsillitis, or both (pharyngotonsillitis).
-
Pharyngitis is part of most common URIs; however, in the strict sense, acute pharyngitis refers to conditions in which the principal involvement is in the throat.
ETIOLOGY
In Children < 2 Years:
Mostly viral (rhinovirus, adenovirus, coronavirus, enterovirus).
In Children 5-15 Years:
Bacterial, group Aβ hemolytic streptococci (GABHS) is quite common.
N.B. Don’t forget other causes:
- Epstein-Barr virus (infectious mononucleosis) as a cause.
- Viruses.
- Mycoplasma.
CLINICAL PICTURE
GENERAL SYMPTOMS AND SIGNS:
- Fever, sore throat, dysphagia.
- Abdominal pain (due to mesenteric adenitis), vomiting.
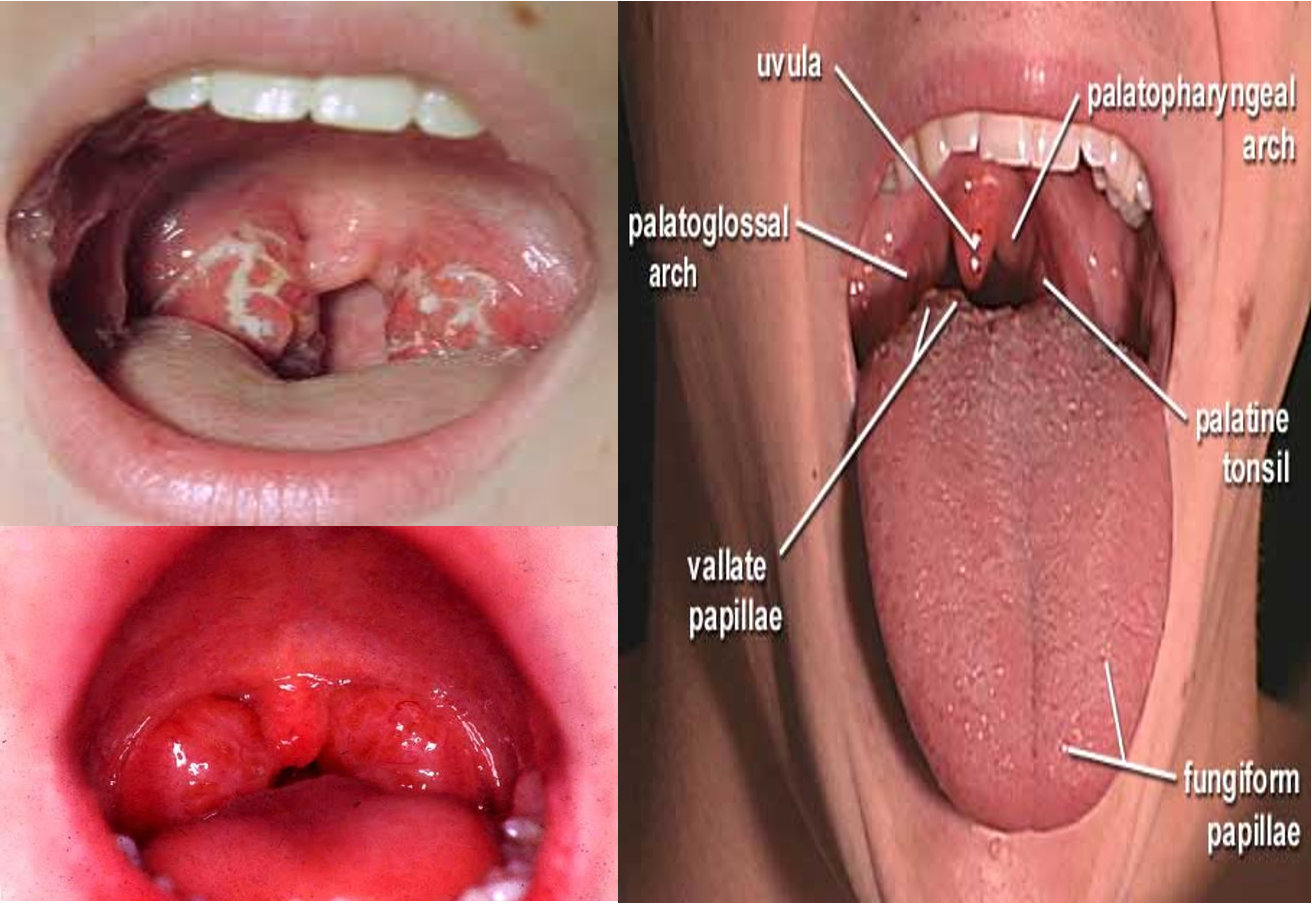
- Throat erythema (redness), palatine petechiae.
- Enlarged tonsils, exudates.
- Anterior cervical lymphadenopathy.
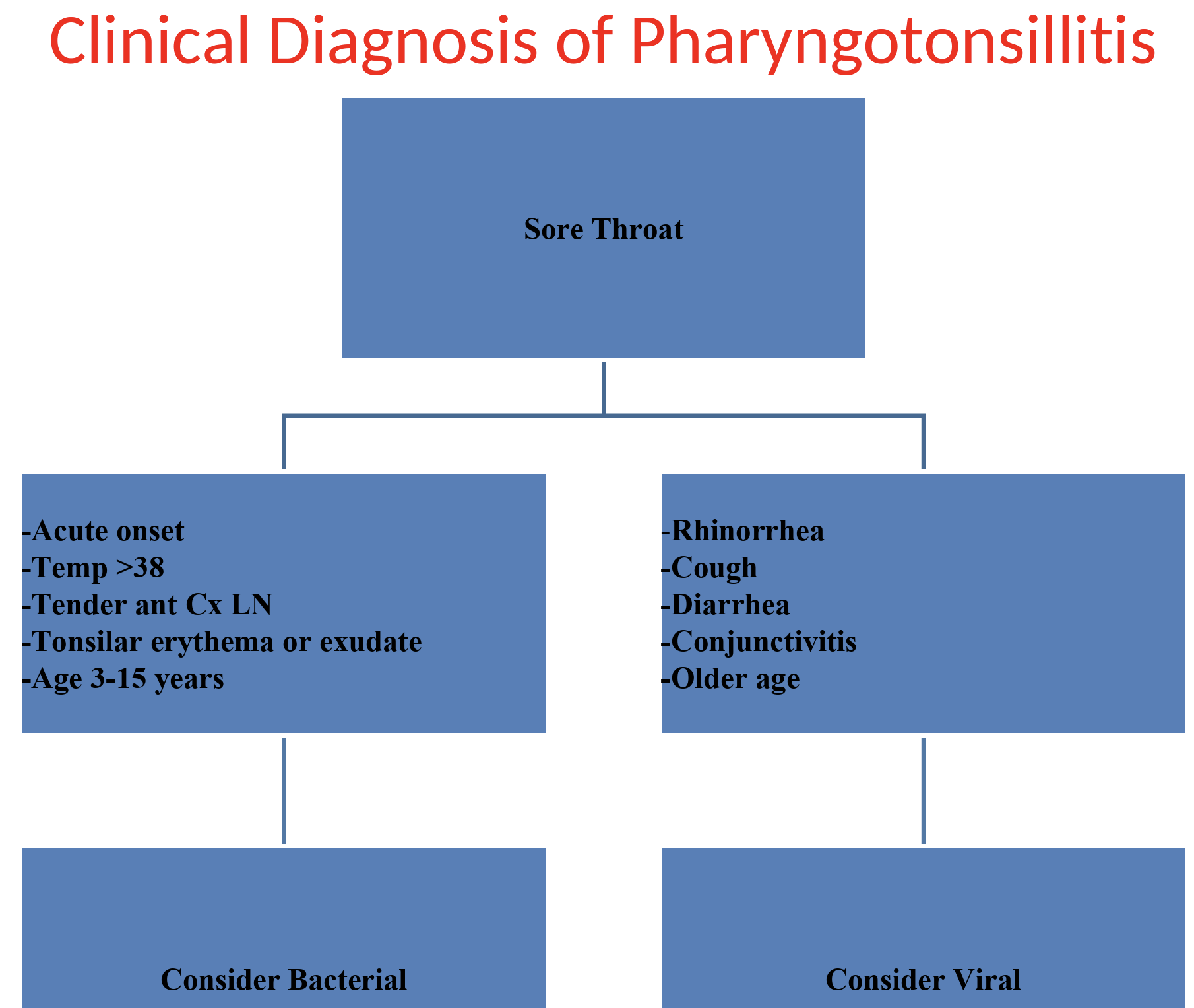
*It is often impossible to distinguish clinically between streptococcal and non-streptococcal sore throat. *
-
The Centor Clinical Scoring System can help to identify those children who have a greater chance of having GAS infection.
-
To calculate the Modified Centor Score, assign points using the following criteria. This can be applied to patients greater than three years of age to assist the clinician regarding the prescription of antibiotics and if this is likely to be beneficial.
Antibiotic treatment is indicated for scores four and above. 2-3 points:
- Rapid antigen test, consider treatment.
Less than 2:
- No need for antibiotics treatment.
| Criteria | Points |
|---|---|
| Temperature > 38°C | 1 |
| No cough | 1 |
| Tender anterior cervical adenopathy | 1 |
| Tonsillar swelling or exudate | 1 |
| Age 3 – 14 years | 1 |
FeverPAIN Scoring System
- Score 0-1: 13-18% streptococci, use NO antibiotic strategy.
- Score 2-3: 34-40% streptococci, use 3-day back-up antibiotic.
- 4 or more: 62-65% streptococci, use immediate antibiotic if severe, or 48hr short back-up prescription.
FeverPAIN is Best Predictor of Streptococcus A/C/G From 2 UK Cohorts:
- F ever last 24h
- Pus on tonsils
- Attend rapidly (3 or less days)
- severely Inflamed tonsils
- No cough or coryza (i.e. pharyngeal illness) = univariate and multivariate in both cohorts
Little P, Moore M, Hobbs FD, et al. Primary care Streptococcal Management (PRISM) study. BMJ Open. 2013;3(10):e003943
DIAGNOSIS OF GROUP Aβ-HEMOLYTIC STREPTOCOCCI
The goal of specific diagnosis is to identify GABHS infection to start prompt and adequate treatment.
THROAT SWAB
- IF +VE: etiology is β-hemolytic.
- IF -VE: do a throat culture.
COMPLICATIONS OF STREPTOCOCCAL PHARYNGITIS
IMMEDIATE:
- Sinusitis.
- Acute Otitis Media
- Peritonsillar abscess.
- Meningitis.
DELAYED:
- Acute post-streptococcal glomerulonephritis.
- Rheumatic fever.
TREATMENT OF ACUTE PHARYNGITIS
GENERAL MEASURES:
- Bed rest.
- Antipyretics e.g. paracetamol or ibuprofen for fever and pain.
- Gargles with warm saline.
- Cool blank liquids.
- Very soft foods.
SPECIFIC TREATMENT FOR BACTERIAL INFECTION:
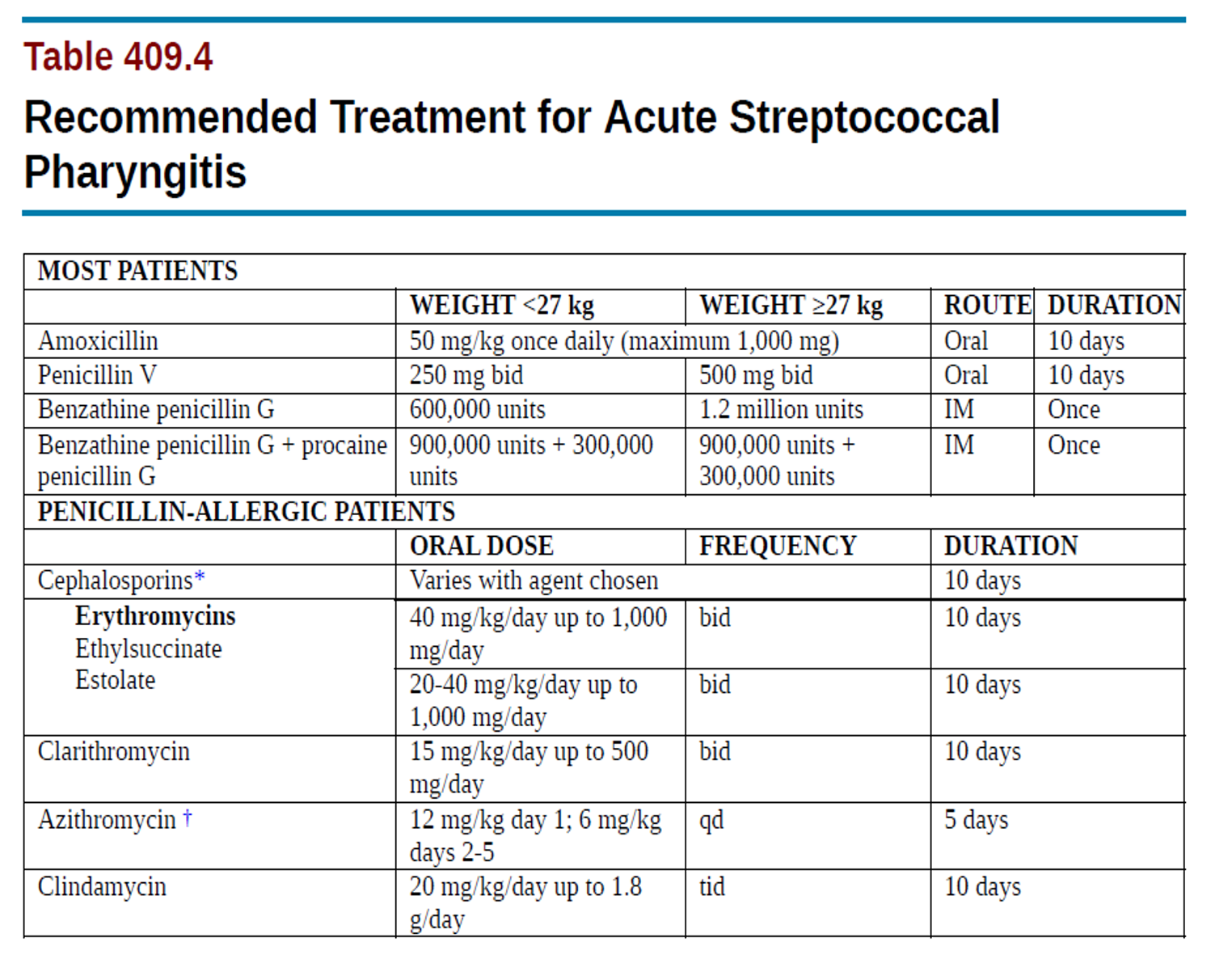 Penicillin V & Oral Peniccilin, benz can be used.
always do sensitivity test prior to administration even if patient was administered before
Penicillin V & Oral Peniccilin, benz can be used.
always do sensitivity test prior to administration even if patient was administered before
second line treatment cephalosporins eryhtromycin clathrio azithro clinda
Therapeutics
Treatment of acute pharyngitis
The primary benefit of treatment is the prevention of acute rheumatic fever,
-
Penicillin V is given bid or tid for 10 days: 250 mg/dose
-
Oral amoxicillin A once-daily 750 mg dose of amoxicillin given orally for 10 days
- A single intramuscular dose of benzathine penicillin (600,000 U)
- for children <27 kg [50 lb]; 1.2 million U for larger children and adults)
-
Erythromycin: 40 m{kglday divided bid, tid, or qid orally for 10 days; for patients allergic to B-lactam antibiotics
-
Eradicating streptococcal carriage is clindamycin, 20 mglkglday divided in 3 doses orally for 10 days.
Long duration of therapy in children is to prevent severe complication of rheumatic heart disease
- Symptomatic treatment
-
Oral analgesic, antipyretics such as acetaminophen or ibuprofen to relieve fever and sore throat.
-
Gargling with warm salt water is often comforting
-
Local anesthetic sprays may provide local relief especially in ulcerative stomatitis.
Surgical Care in Pharyngitis
Indications for tonsillectomy:
- 4-5 confirmed group A streptococcal infections in a single year.
- Chronic sore throat with adenopathy that is not responsible to treatment over 6 months.
- Hypertrophied tonsils with obstruction of breathing or deglutition
Home message
-
Up to 90% of URTI are of viral etiology.
-
Throat congestion, exudate and tender anterior cervical adenopathy in children > 2 years are suggestive of streptococcal etiology
-
Penicillin for 10 days is the drug of first choice in streptococcal sore throat infection.
-
ARF and PSGN are important late sequelae of maltreated GAS throat infection.
-
Viral causes:
- -Rhinoviruses (> 100 serotypes).
- -Influenza
- -Parainfluenza
- -RSV
- -Coronavirus
- -Adenoviruses
- -Enteroviruses
- -Epstein-Barr
- -Herpes simplex
-
Bacterial causes:
- -Group A beta hemolytic Streptococci (GAS) (Most common)
- —Mycoplasma pneumoniae
- -N. gonorrhea
- -Corynebacterium diphtheriae
- -Bacteria as Streptococcus pneumoniae, Haemophilus (?)
Etiology of Acute Pharyngitis
A variety of bacteria & viruses can cause infection in the pharynx. But the etiology is mostly viral.
5-30% are bacterial usually caused by a classic bacterial infection causing sore throat is: Streptococcus pyogenes (GABHS), which can cause abscesses on the tonsils. in children may reach to 10 days in children - major complication rheumatic heart disease
GABHS infection is usually self-limited and therapy is usually indicated to prevent late sequelae as AGN or ARF.
Non infectious causes include allergy or physical irritation
Infection occurs through contact with infected secretions and can be interrupted through hand hygiene.
GAS infection is uncommon before 2-3 y and peaks in early school years and occurs most often in winter and spring.
Clinical picture:
1) streptococcal pharyngitis
- Sore throat,
- Red pharynx, enlarged tonsils and classically covered with a yellow, blood-tinged exudate.
- petechiae on the soft palate and posterior pharynx.
- enlarged , tender anterior cervical lymph nodes.
- The incubation period is 2-5 days.
Hallmarks of STREP sore throat
- •Group A streptococcal infections affect all ages but peak incidence at 5-15 years of age
- •Tender lymph nodes
- •Close contact with infected person
- •Scarlet fever rash
- •Tonsillar exudates in older children
- •Abdominal pain
- •GOLD STANDARD: POSITIVE THROAT CULTURE

2) Viral pharyngitis
- Gradual onset , rhinorrhea, cough, and diarrhea.
- A viral etiology is suggested by the presence of conjunctivitis, hoarseness, and cough.

Complications Y
- Viral infections may predispose to bacterial middle ear infections.
- Streptococcal pharyngitis
local suppurative complications, as parapharyngeal abscess, sinusitis, otitis media and adenitis
nonsuppurative illnesses, as acute rheumatic fever and acute post infectious glomerulonephritis.
Differential diagnosis: Y
- Pneumococcal or H influenza
- membranous exudate: diphtheria, EBV
- Agranulocytosis: ulcerative lesion