What is medical history?
Medical history is a chronological record or account of the patient’s symptoms from the onset (start) of their illness until the time of presentation to his doctor
It includes the significant past illnesses, and the effects of the social, family and occupational environments on the present’s illness (and vice versa), in addition to previous therapeutic procedures and current drugs taken
History helps in:
-
Establishing a rapport (mutual trust and respect) with the patient.
-
Reaching a diagnosis of patient’s health problem Or listing possible causes of his problem (differential diagnosis)
-
Guiding focused examination, investigations and even the plan of management
-
Assessment of the impact of disease on the patient’s family
Introduction
- Skilled history taking is reported to be declining.
- core art of patient care
- vital piece of the physician-patient encounter
- Helps lead to the final diagnosis about 75% of the time
- Listening is in and of itself a major therapeutic act and the physician himself is a great therapeutic instrument.
- What triggers patients to come?
Present yourself as a caring, competent, and confident health care professional.
Building Trust & Patient Rapport When you introduce yourself to the patient, shaking hands or offering a comforting touch will help build trust.
Angry doctor
- Use appropriate language.
- Use an appropriate level of questioning, but do not appear condescending.
- When encountering communication barriers, try to enlist someone to help.
- Actively listen.
1. Clinician-centered approach
-
The clinician dictates the interaction to meet his or her own needs – eliciting symptoms and other data to facilitate making a diagnosis.
-
Using closed-ended questions.
Deficiencies includes
- Failing to allow patients to express personal concerns.
- Patients do not have the opportunity to lead the encounter (meeting/interview).
- Patients are interrupted.
2. Patient-centered approach
Validating Validating the importance of a patient’s concerns.
Allowing Allowing the patient to develop comfort with the provider as he/she leads the conversation.
3. Integrated approach
- Personal data
- chief complaint
- history of present illness
- past medical history
- past surgical history
- past obstetric and gynecologic history
- Family history
- Drug history
- Social history
- other health issues/behaviours /hazards,
- Review of systems.
Skills of patient-centered communication
- open-ended questioning.
- non-verbal communication skills such as purposeful silence or non-verbal encouragement.
- Attentive listening.
- summarizing or paraphrasing.
The “Five-Step” model (for patient-centered communication)
| Steps | Description | Actions to be taken |
|---|---|---|
| 1 | Set the stage for the interview | •Welcome patient, use patient’s name, clinician introduction of him/herself. •Ensure patient readiness and privacy •Remove communication barriers. •Establish patient comfort. |
| 2 | Elicit (work out) the chief complaint and set an agenda for the visit. | •Indicate available time. •Obtain list of issues patient wants to discuss. •Summarize/finalize agenda, prioritize items for current encounter versus future encounter. |
| 3 | Open the history of present illness (non-focused) | •Ask open-ended questions to elicit problems. •Use active listening, which includes silence and non-verbal encouragement. |
| 4 | Continue the patient-centered history of present illness (focused) | •Use focused (clear), but open-ended, questions to obtain description of physical symptoms. •Explore patient description of symptoms, emotional or social context of symptoms. |
| 5 | Transit to the clinician-centered process | •Summarize conversation, confirm accuracy of information •Inform patient that style of questioning will now change (“I’m now going to ask you several specific medical questions about your symptoms”) |
History Process
A- Preliminary Data: Demographic
- Date and time
- Age
- Sex
- Race
- Birthplace
- Occupation
- DOA
B- Components of History Y
- Establishing rapport.
- Demographic data.
- Chief - Presenting complaint. Z
- History of the present illness. Z
- Past medical history. Z
- Family history
- Drug history
- Psychosocial history- Allergy
- Review of systems. Z
C- ideas, concerns, expectations
- Do you have any other information for me?
- Do you have any questions for me?
Special Challenges
- Silence
- Over talkative
- Multiple symptoms
- Anxiety
- Depression
- Sexually attractive or seductive patients
- Confusing behaviors or symptoms
- Patients reassurance
- Anger and hostility
- Intoxication
- Crying
- Language barriers
- Limited intelligence
- Hearing problems
- Blindness
- Talking with families or friends
-
Patient unable to talk!!!!
Complete the questions using the words or phrases in the slide below.
Symptoms, major health problem, in hospital, up–to–date, childhood diseases
- Have you ever had any …like measles or chicken pox?
- Have you ever been …for more than a week?
- Do you have a …such as diabetes or high blood pressure?
- Are you …with your immunizations?
- What were the first …of your overactive thyroid?
Which question from each pair is more polite?
1- A: Is there anyone in your family who is crazy? B: Is there anyone in your family who suffers from mental illness? 2- A: At what age did your father die? B: How old was your dad when he popped off?
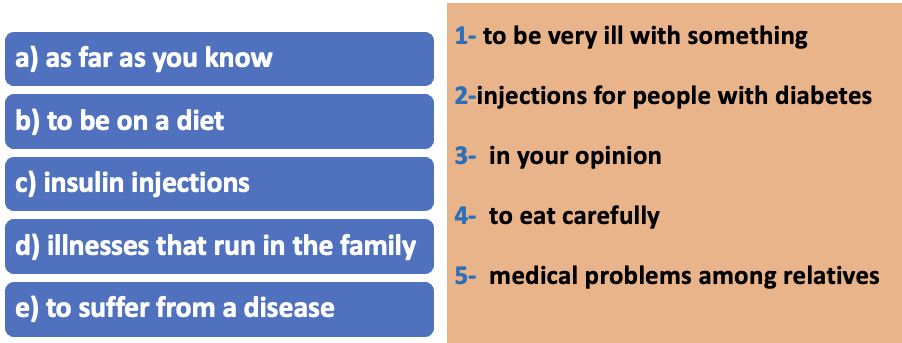
Match up those phrases which have the same meaning.