The term “Aminoglycoside” stems from their structure— two amino sugars joined by a glycosidic linkage to a central hexose nucleus.
- Narrow therapeutic index,
Drugs includes the following:
- Streptomycin: Family prototype tuberculosis & TB meningitis (intrathecal), also plague, tularemia and brucellosis.
w/ BENZYL PENICILLIN treatment of Streptococcal viridans and Enterococcal endocarditis infections and as prophylaxis in persons with known valvular disease undergoing surgery. & septicemia; anaerobes are thought to be present (e.g. peritonitis)
-
Neomycin & Gentamicin: Used in treatment regimens Topical: (Skin, Eye, Ear) + POLYMYXINS B + Bacitracin + Adrenal corticosteroids to reduce resistance. Orally: Sterilization of intestine before surgery, Bacillary Dysentery and Watery Diarrhea, Hepatic Coma, also Plaque, Tularemia, and Brucellosis
-
Tobramycin: pseudomonas + Genta resistance
-
Amikacin & Netilmicin: Less potent but BROAD + Genta resistance
-
Paromomycin: Very ototoxic & Intestinal amoebiases + same as neomycin
-
Spectinomycin: N. gonorrhoea + penicillin resistance/sensitivity
MOA: Cidal
Drug positive charge allows them to bind to the negatively charged outer membrane with formation of transient holes through which antibiotic molecules move.
It diffuse through porin channels in the outer membrane of susceptible organisms. These organisms also have an oxygen-dependent system that transports the drug across the cytoplasmic membrane. Inside the cell, they bind the 30S ribosomal subunit, causing misreading of the genetic code, leading to incorrect protein formation and interruption of protein synthesis.
Antimicrobial spectrum:
- All aminoglycosides have a similar spectrum of antimicrobial action. They are most active against aerobic gram negative bacilli.
- Mycobacterium tuberculosis is susceptible to streptomycin, kanamycin.
The bactericidal effect of aminoglycosides is: The higher dose, the better effect. - its effects persists for days when drug is stopped
-
Concentration dependent; that is, efficacy is dependent on the maximum concentration (Cmax) of drug above the minimum inhibitory concentration (MIC) of the organism. For aminoglycosides, the target Cmax is 8-10 times the MIC.
-
They also exhibit a post-antibiotic effect (PAE), which is continued bacterial suppression after the drug levels fall below the MIC. (The larger the dose, the longer the PAE.
Because of these properties, extended interval dosing (a single large dose given once daily) is now more commonly utilized than divided daily doses. This reduces the risk of nephrotoxicity and increases convenience
These drugs have a narrow therapeutic window, and improper dosing carries the risk of inflicting significant toxicity (primarily nephro- and ototoxicity) on your patients.
Once-daily or extended-interval aminoglycoside dosing leverages the concentration dependent killing of the drugs to create an equally effective, more convenient, and possibly safer dosing regimen.
Resistance to aminoglycosides occurs via:
- Efflux pumps.
- Decreased uptake, and/or
- Modification and inactivation by plasmid associated synthesis of enzymes. Each of these enzymes has its own aminoglycoside specificity; therefore, cross-resistance cannot be presumed.
[Note: Amikacin is less vulnerable to these enzymes than other antibiotics in this group]
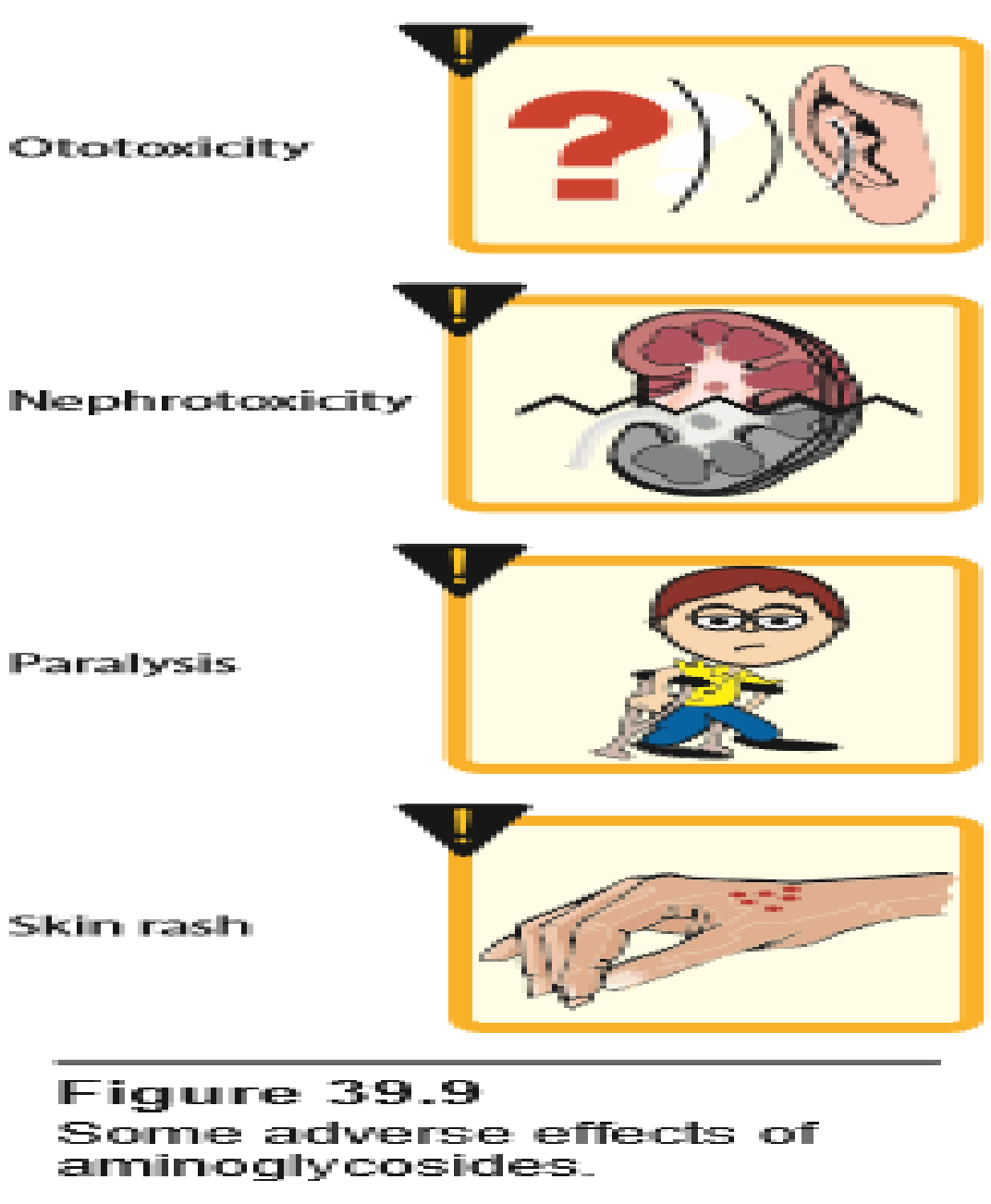
Kinetics:
- They are water-soluble and do not readily cross any lipoprotein tissue barrier , thus intestinal absorption is poor, and penetration to CSF is very limited.
- They can cross the placental barrier and may accumulate in fetal plasma causing congenital deafness.
- Plasma binding is low (30%)
- They are eliminated by glomerular filtration. Accumulation occurs in patients with renal function, and dose adjustments are required.
- They are more active in alkaline medium in cases of urinary tract infection.
More than 90% of the parenteral aminoglycosides are excreted unchanged in urine .
- Absorption: Not easily absorbed Orally
- Distribution: BBB: Do Not Cross; Placenta: Can Cross placenta (Congenital Deafness) but safely used with breast feeding.
- Metabolism: By liver
- Excretion: Excreted by kidney & high concentrated in urine especially alkaline (UTI)
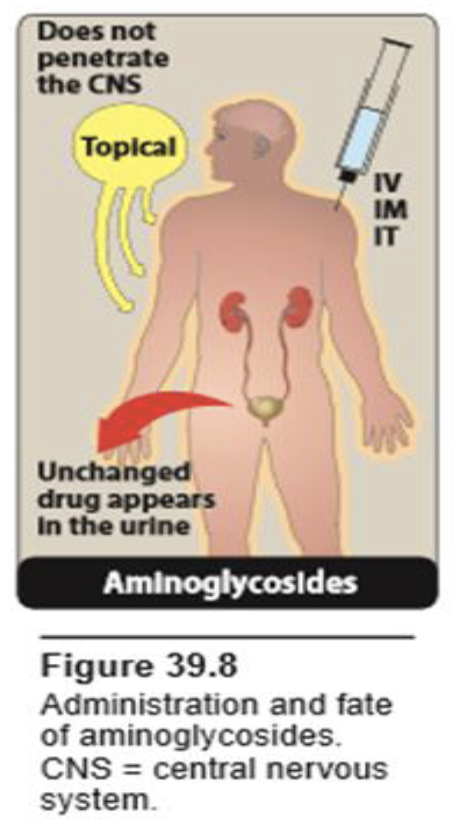
Adverse Effects: (Narrow Index)
- Nephrotoxicity: Reversible Tubular Damage
- ototoxicity: (Cochlea or Vestibule): ++ risk with age, renal disease, preexisting hearing defect, usage of aminoglycosides or diuretics.
- Neuromuscular Blocakde: especially if given with anesthesia or muscle relaxants
- Malabsorption: with Oral preparation of (Neomycin, Kanamycin, Paromomycin) It is due to: *Neomycin binds with bile salts and inhibits pancreatic lipase with failure of fat digestion and absorption leading to steatorrhoea and diarrhoea. & Decreased intestinal lactase activity lead to malabsorption of lactose, which by osmotic action makes gut content more fluid and more easily eliminated.
- Allergic Reactions: Contact dermatitis is a common reaction to topically applied neomycin
Drug Interactions:
- With Antibiotics: • -With cephalosporins nephrotoxicity increases. -Anti-pseudomonal penicillins, and cephalosporins decrease the antibacterial effect of gentamicin if combined together in the same syringe because penicillins are acidic and aminoglycosides are alkaline.
- Skeletal muscle relaxants: minoglycosides increase the effect of non-depolarizing NMB agents .It could be reversed by neostigmine and calcium gluconate. Aminoglycosides should be administered with great caution during surgery or in the post-operative period.
- Diuretics and Antihistamines: Furosemide, Mannitol and antihistamins potentiate ototoxicity of aminoglycosides.