Neurological Cases
Neurological Case 1
A 3-year-old boy brought to ER by his mother, she noticed that the child is c/o abnormal sensation in the lower limbs (pins and needles sensation) and he had a Hx of common cold preceding these symptoms by 1 week. And he’s polio-immunized (he took his full vaccines). There’s nothing specific in the history, and on examination he looks completely well apart from that his complaint of the pins and needles abnormal sensation in his LLs.
- What relevant questions you should ask the mother which can help you reach the diagnosis? (2 Qs)
- Fever
- Joint pain
- Skin rash
- Vomiting
- Diarrhea
- FHx of poliomyelitis
- What physical examination you should do?
- Vital signs (BP, temperature, RR)
- Lower limb (power, tone, reflexes).
- What investigations you should order?
- CSF (LP).
- Blood culture
- EMG
- Nerve conduction velocity
- What’s your DDx?
- Head trauma
- GBS
- Poliomyelitis
- Peripheral neuropathy
- Vitamin deficiency
- What’s your management?
- Monitoring vital signs (BP and O2 sat.)
- Assess respiratory system (with GBS).
- Antipyretic if febrile.
Neurological Case 2
13 month old child brought to ER with history of two attacks of convulsion 40 minutes before arrival to ER. He had fever and cough for one day .immunization was according to national schedule and received MMR 2 days prior to ER visit .
The infant had been born at term by normal vaginal delivery, discharged form hospital next day and his development was normal. he had normal vital signs. Chest and CVS examination was normal. Abdomen :The spleen was palpable 2 cm below the left costal margin. joints examination was normal
- a- Write 2 relevant questions, to ask the mother?
- b- What 2 specific signs you should look for during examination of this child?
- C- What 2 important investigations?
- d- What is the most likely diagnosis and give two differential diagnosis?
- e- Mention two important points in the management plan?
Answers:
-
A: did he has seizure episodes before? Is there a family history of seizure?
-
B: tongue biting, if level of consciousness is affected, signs of dehydration.
-
C: blood glucose level, midstream urine sample, CT and MRI.
-
D: diagnosis is febrile seizure
- DDx is drug intoxication, head trauma, epilepsy.
-
E:
- Termination of seizure by rectal Diazepam.
- Reassure and education as giving antipyretics and tell the parents about the sign of dehydration because it can be a cause of seizure, also prevent accidental injury when falling during the attack.
Neurological Case 4
An 8 years old boy, suddenly got tonic clonic convulsion ,eyes rolling, when he woke he was : lethargic, unconscious disoriented, temp:38 And recently he has URTI
- Q1: what would you like to ask the mother about ?
- Q2: mention 2 important investigations ?
- Q3: give two important management ?
- Q4: what is the diagnosis ? Encephalitis
- Q5: what is the type of isolation ? Air borne
^sorry, I didn’t write the answers because I’m not sure, but the doctor said it’s Encephalitis not Febrile seizure .
- Q1) Did it start in one side of the body and spread elsewhere Later? Family history of epilepsy & Immunization history? any other neurologic symptoms?
- Q2) Blood glucase - Blood gases - Electrolytes - Calcium , Mg , Phosphorous - CT , MRI - LA
- Q3) Antipyretics - Anticonvulsants - Iv Antibatic
- Q4) Generalized tonic - clonic Seizure due to encephalitis
Neurological Case 5
7 year old Saudi girl brought to ER with complaints of pins and needles” sensations in her toes and proximal muscle weakness of the lower extremities. She had diarrhea 4 weeks prior to ER visit which was associated with abdominal pain and last for few days only. She was healthy child before these events with normal development but the national immunization schedule was not completed. On examination : HR 90/M,BP:110/76,temp 37.6c Chest :equal BS on both side ,CVS; Short systolic murmur grade 2/6 at LLSB with normal .pulses in all limbs
-
a. Ask the child or mother about the following:
- Prickling, “pins and needles” sensations in other parts e.g fingers, ankles or wrists
- Does the Weakness in her legs spreads to her upper body
- Any Difficulty with eye or facial movements, including speaking, chewing or swallowing
- Severe pain that may feel achy or cramp-like and may be worse at night
- Difficulty with bladder control or bowel function
- Rapid heart rate
- Difficulty breathing.
-
b. specific signs you should look for during examination:
- tachycardias and bradycardias
- Tachypnea
- Blood pressure lability (alterations between hypertension and hypotension).
- Respiratory examination looking for poor inspiratory effort or diminished breath sounds .
- abdominal examination: looking for paucity or absence of bowel sounds (suggests paralytic ileus). Suprapubic tenderness or fullness (suggestive of urinary retention).
- Facial weakness (cranial nerve VII), cranial nerves VI, III, XII, V, IX, and X (Involvement of facial, oropharyngeal, and ocular muscles results in facial droop, dysphagia, dysarthria).
- Ophthalmoparesis, Ptosis.
- Lower extremity weakness, symmetrically and progressively.
- Upper extremity, trunk, facial, and oropharyngeal weakness.
- sensory changes
- Hyporeflexia or areflexia
- Hypotonia
-
C. Important investigations:
- Complete blood counts (CBCs) and metabolic panels, (ESR)
- Electromyography (EMG) and nerve conduction studies (NCS).
- Lumbar puncture for cerebrospinal fluid (CSF) studies ( CSF protein).
- Frequent evaluations of pulmonary function parameters.
- magnetic resonance imaging (MRI) and computed tomography (CT) scanning of the spine,
-
d. DDx:
- Acute myelopathy (eg, from compression, transverse myelitis, vascular injury)
- Chronic inflammatory demyelinating polyneuropathy
- Conversion disorder/hysterical paralysis
- Neurotoxic fish or shellfish poisoning
- Paraneoplastic neuropathy
- Poliomyelitis
- Porphyria polyneuropathy
- Spinal cord compression
- Spinal cord syndromes, particularly postinfection
- Tick paralysis
- Toxic neuropathies (eg, arsenic, thallium, organophosphates, lead)
- Vasculitic neuropathies
- Vitamin deficiency (eg, vitamin B-12, folate, thiamine)
- Acute cerebellar ataxia syndromes
- Posterior fossa structural lesion
-
e. The management plan:
- Admission to a hospital for close monitoring .
- Admission to an ICU, ( if develop respiratory failure).
- Intravenous immunoglobulin (IVIG) and plasma exchange
- Continued care also is needed to minimize problems related to immobility, neurogenic bowel and bladder, and pain.
Patient Case: Guillain-Barre Syndrome (GBS)
7-year-old Saudi girl brought to ER with complaints of pins and needles” sensations in her toes and proximal muscle weakness of the lower extremities. She had diarrhea 4 weeks prior to ER visit which was associated with abdominal pain and last for few days only. She was a healthy child before these events with normal development but the national immunization schedule was not completed.
On examination: HR 90/M, BP:110/76, temp 37.6c
Chest: equal BS on both sides, CVS; Short systolic murmur grade 2/6 at LLSB with normal pulses in all limbs.
a. Ask the child or mother about the following:
- Prickling, “pins and needles” sensations in other parts e.g fingers, ankles or wrists
- Does the Weakness in her legs spread to her upper body
- Any Difficulty with eye or facial movements, including speaking, chewing or swallowing
- Severe pain that may feel achy or cramp-like and may be worse at night
- Difficulty with bladder control or bowel function
- Rapid heart rate
- Difficulty breathing.
b. specific signs you should look for during examination:
- Sensory changes
- Hyporeflexia or areflexia
- Hypotonia
- tachycardias and bradycardias
- Tachypnea
- Blood pressure lability (alterations between hypertension and hypotension).
- Respiratory examination looking for poor inspiratory effort or diminished breath sounds.
- abdominal examination: looking for paucity or absence of bowel sounds (suggests paralytic ileus). Suprapubic tenderness or fullness (suggestive of urinary retention).
- Facial weakness (cranial nerve VII), cranial nerves VI, III, XII, V, IX, and X (Involvement of facial, oropharyngeal, and ocular muscles results in facial droop, dysphagia, dysarthria).
- Ophthalmoparesis, Ptosis.
- Lower extremity weakness, symmetrically and progressively.
- Upper extremity, trunk, facial, and oropharyngeal weakness.
- sensory changes
- Hyporeflexia or areflexia
- Hypotonia
c. Important Investigations
- Complete blood counts (CBCs) and metabolic panels. Erythrocyte sedimentation rate (ESR)
- Electromyography (EMG) and nerve conduction studies (NCS).
- Lumbar puncture for cerebrospinal fluid (CSF) studies (CSF protein).
- Frequent evaluations of pulmonary function parameters.
- Magnetic resonance imaging (MRI) and computed tomography (CT) scanning of the spine.
d . Most Likely Diagnosis
- Guillain-Barre Syndrome
e. Differential Diagnosis Problems to consider in the differential diagnosis of Guillain-Barré syndrome (GBS) include the following:
- Acute myelopathy (eg, from compression, transverse myelitis, vascular injury)
- Chronic inflammatory demyelinating polyneuropathy
- Conversion disorder/hysterical paralysis
- Neurotoxic fish or shellfish poisoning
- Paraneoplastic neuropathy
- Poliomyelitis
- Porphyria polyneuropathy
- Spinal cord compression
- Spinal cord syndromes, particularly postinfection
- Tick paralysis
- Toxic neuropathies (eg, arsenic, thallium, organophosphates, lead)
- Vasculitic neuropathies
- Vitamin deficiency (eg, vitamin B-12, folate, thiamine)
- Acute cerebellar ataxia syndromes
- Posterior fossa structural lesion
f. Management Plan
- Admission to a hospital for close monitoring.
- Admission to an ICU, (if develop respiratory failure).
- Intravenous immunoglobulin (IVIG) and plasma exchange
- Continued care also is needed to minimize problems related to immobility, neurogenic bowel and bladder, and pain.
 Intraosseous Access:
Intraosseous Access:
- Q1: What is the name of the procedure shown in the picture?
- Q2: Write two advantages of the procedure.
- Q3: Write two Contraindications for the procedure?
Answers:
- Q1: Intraosseous needle.
- Q2: When failure to find an IV line, we can use this method. Also, it is fast and can be used in emergency cases such as cardiac arrest.
- Q3: Infection at the site, fracture, osteoporosis.
Case Study: Oxygen Hood

Questions
- A-What is the name of the instrument?
- Oxygen hood
- B-this instrument used for
- Deliver more O2 to the baby
- C-give one alternative instrument?
- Nasal cannula, face mask
- D-how to monitor the improvement?
- Pulse oximetry
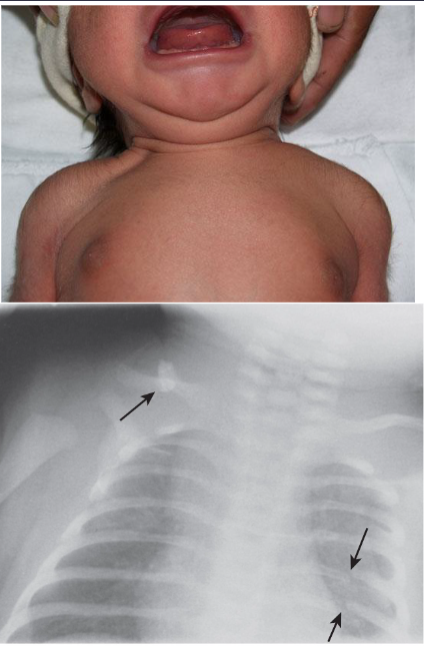
4.9 kg girl delivered by mid forceps after right shoulder dystocia
- Chest radiograph. What does it show? A right mid-clavicular fracture and incidental fractures of left fifth and sixth ribs.
 Pulse Oximeter Questions:
Pulse Oximeter Questions:
- Q1: Mention the name of the device seen above?
- Pulse Oximeter
- Q2: What does it measure?
- Oxygen saturation (SO2) in the blood
- Q3: What factors affect the accuracy of the results?
- Hypoperfusion of the extremity
- Vasoconstriction
- Movement
 Station -3:
Station -3:
- Describe the maneuvers done?
- The procedure is called “CardioPulmonary Resuscitation”.
- In the picture, it is done by 2 personnel.


What is this procedure?
- Positive-Pressure Ventilation & Chest Compressions
- When to do? No pulsation and shock
 What to do ? • CT brain • Diagnosis? • Battered baby syndrome
What to do ? • CT brain • Diagnosis? • Battered baby syndrome
Case Study: Spina Bifida

Questions
- A-What is the diagnosis?
- Spina Bifida
- B-Give one complication?
- C-Give one sign present?
- D-What is the management?
- Surgery

Pull to Sit Test
What does a positive test indicate? Hypotonia, specifically head lag in this case.

Status Epilepticus
- GE, status epilepticus, What to measure next? Blood pressure.

Case
What is the name of procedure shown above? Lumbar puncture Mention 2 contraindications of it? Local infection, Hydrocephalus What does the content of the collecting tubes indicate ? One tube contains normal clear CSF, The 2nd tube contains turbid CSF suggesting meningitis or traumatic specimen.