IM
RHEUMATOID ARTHRITIS

Prof. Salih Bin Salih
RHEUMATOID ARTHRITIS
A chronic progressive disease causing inflammation in the joints and resulting in painful deformity and immobility, especially in the fingers, wrists, feet, and ankles”.
- Pattern of joints affected — RA usually affects the same joints on both sides of the body.
“In the early stages, rheumatoid arthritis typically affects small joints, especially the joints at the base of the fingers, the joints in the middle of the fingers, and the joints at the base of the toes. It may also begin in a single, large joint, such as the knee or shoulder, or it may come and go and move from one joint to another”.
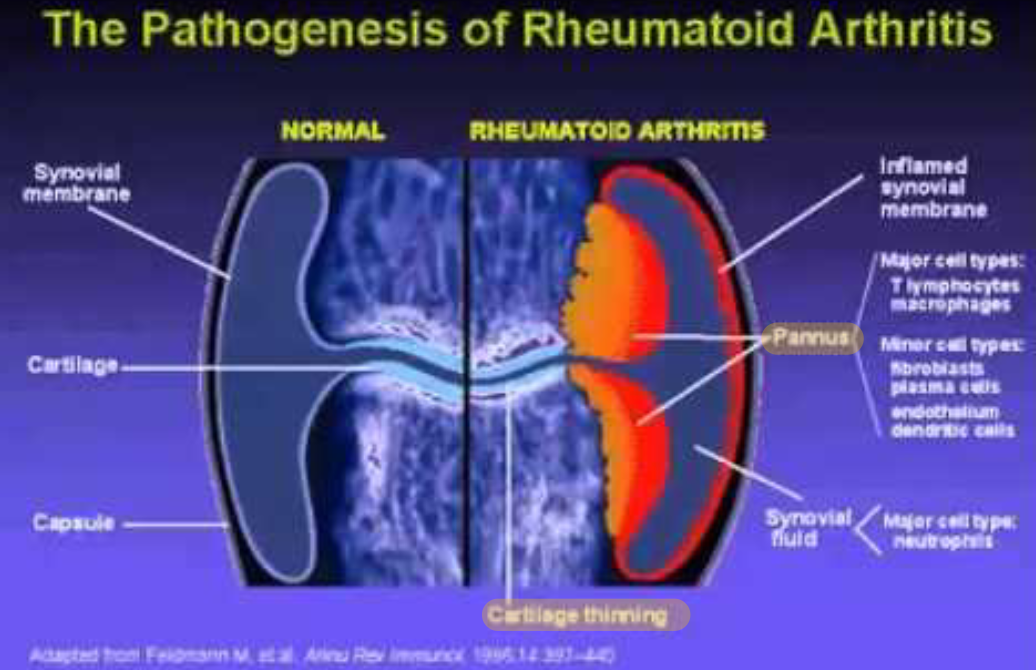
Pathophysiology: Rheumatoid arthritis
❖ An external trigger that triggers an autoimmune reaction, leading to synovial hypertrophy and chronic joint inflammation along with the potential for extra-articular manifestations.
❖ Synovial cell hyperplasia and endothelial cell activation lead to uncontrolled inflammation and cartilage and bone destruction.
❖ Genetic factors and abnormalities of immune system contribute to disease propagation.
DIAGNOSIS —
There is no single test used to diagnose RA.
Diagnosis is based upon characteristic signs and symptoms, the results of laboratory tests, and the results of x-rays.
| Diagnosis |
|---|
| ❖ Morning stiffness that lasts at least one hour and that has been present for at least six weeks |
| ❖ Swelling of three or more joints for at least six weeks |
| ❖ Swelling of the wrist, hand, or finger joints for at least six weeks |
| ❖ Swelling of the same joints on both sides of the body |
| ❖ Changes in hand x-rays that are characteristic of rheumatoid arthritis |
| ❖ Rheumatoid nodules of the skin |
| ❖ Blood test positive for rheumatoid factor and/or anti-citrullinated peptide/protein antibodies (ACPA) →Specific |
ACR/EULAR CRITERIA FOR RHEUMATOID ARTHRITIS DIAGNOSIS
| Score | |
|---|---|
| A Joint involvement | |
| 1 Large joint | 0 |
| 2 – 10 large joints | 1 |
| 1 – 3 small joints | 2 |
| 4 – 10 small joints | 3 |
| > 10 joints (≥ 1 small joint) | 5 |
| B Serology (≥ 1test result needed) | |
| Negative RF and negative ACPA | 0 |
| Low-positive RF or low-positive ACPA | 2 |
| High-positive RF or high-positive ACPA | 3 |
| C Acute phase-reactants (≥ 1test result needed) | |
| Normal CRP and normal ESR | 0 |
| Abnormal CRP or ESR | 1 |
| D Duration of symptoms | |
| < 6 weeks | 0 |
| ≥ 6 weeks | 1 |
Definite diagnosis requires total score ≥ 6/10
Inspection
-
❖ Hands – The joints of the hands are often the very first joints affected by RA. Certain hand deformities can occur with longstanding RA. The fingers may develop swan neck and boutonniere deformities.
-
❖ Wrist – Most commonly affected joint. In the early stages of RA, it may become difficult to bend the wrist backward.
-
❖ Elbow – Swelling of this joint may compress nerves.

Laboratory Studies
Useful laboratory studies fall into 3 categories—
- ❖ Markers of inflammation
- ❖ Hematologic parameters
- ❖ Immunologic parameter
include following:
- ❖ Erythrocyte sedimentation rate (ESR)
- ❖ C-reactive protein (CRP) level
- ❖ Rheumatoid factor (RF) assay(may be negative in 20%)
- ❖ Antinuclear antibody (ANA) assay خاص *
- ❖ Anti-cyclic citrullinated peptide (ACCP)levels. More specific and confirmatory
Markers of inflammation
- ❖ The ESR and the CRP level are associated with disease activity. The CRP value over time correlates with radiographic progression.
Hematologic parameters
- ❖ CBC — anemia of chronic disease correlates with disease activity; it improves with successful therapy.
- ❖ Hypochromic anemia may suggest blood loss, commonly from GIT associated NSAIDs.
- ❖ Thrombocytosis is common and is also associated with disease activity. Thrombocytopenia may be a rare adverse event of therapy and may occur in patients with Felty syndrome.
- ❖ Leukocytosis may occur but is usually mild. ❖ Leukopenia — consequence of therapy or a component of Felty’s syndrome. (Rheum. Arthritis+splenomegaly+neutropenia)
Immunologic parameters
-
❖ Rheumatoid factor - An immunoglobulin M (IgM) antibody is present in the blood of 70 to 80% of RA.
-
❖ RF is not specific for RA present in other connective tissue diseases, infections, and autoimmune disorders, as well as in 1-5% of healthy people. The presence of RF predicts radiographic progression of bone erosions, independent of disease activity. RF values fluctuate with disease activity, though titers of RF generally remain high even in patients with drug-induced remissions.
-
❖ Anti-citrullinated peptide/protein antibody (ACPA) test — are more specific than RF for diagnosing RA. Anti-ACPA antibody tests may be positive very early in the course of disease. The test is positive in most patients with RA.
Joint Aspiration indications
-
To R/O - coexistent infection or crystal arthritis in an acutely swollen joint.
-
In a new-onset Unilateral monoarticular arthritis or an unusual flare up in a patient with RA may need joint aspiration and synovial fluid analysis.

Radiographic Feature
- Peri-articular osteopenia
- Uniform symmetric joint space reduction
- Marginal sub-chondral erosions
- Joint sublaxations
- Joint destruction
- Collapse
- Ultrasound detects early soft tissue swelling
- MRI has greatest sensitivity to detect synovitis and marrow changes
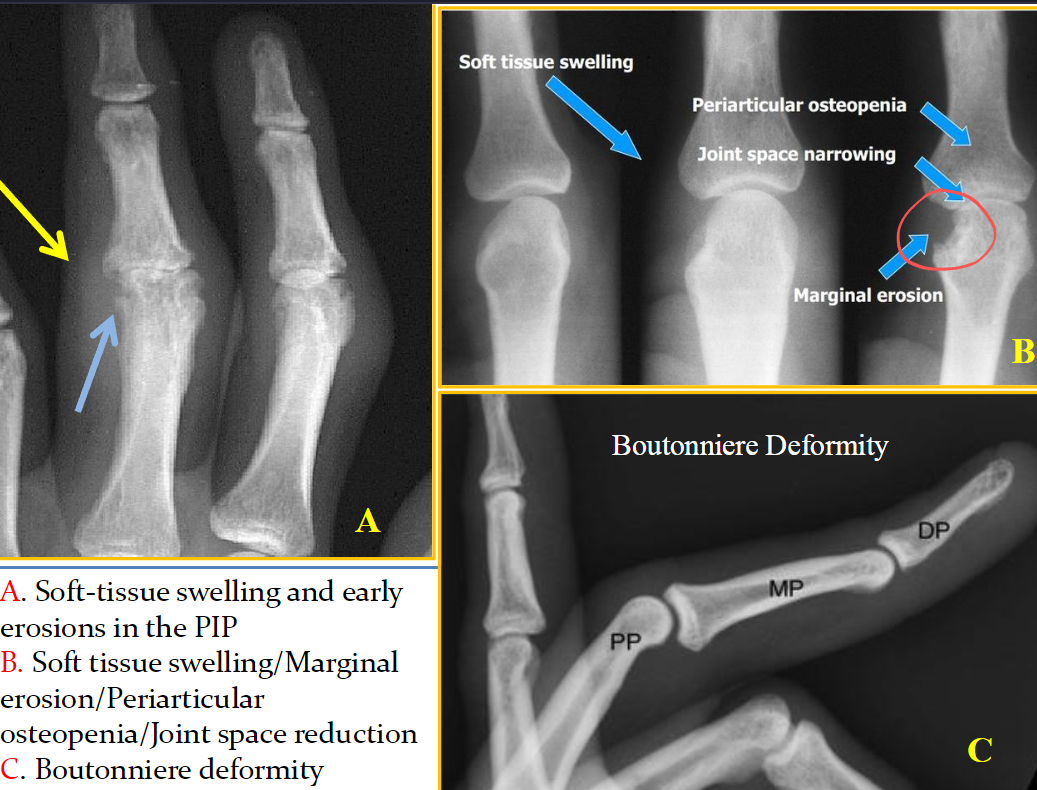 A. Soft-tissue swelling and early erosions in the PIP
B. Soft tissue swelling/Marginal erosion/Periarticular osteopenia/Joint space reduction
C. Boutonniere deformity
A. Soft-tissue swelling and early erosions in the PIP
B. Soft tissue swelling/Marginal erosion/Periarticular osteopenia/Joint space reduction
C. Boutonniere deformity
Extra-articular manifestations of RA
| Systemic | Musculoskeletal Z |
|---|---|
| Fever | Muscle wasting due to not moving |
| Weight loss | Tenosynovitis/Bursitis |
| Fatigue | Osteoporosis |
| Hematological Z | Ocular Z |
| Anaemia | Episcleritis/Scleritis |
| Thrombocytosis | Scleromalacia |
| Eosinophilia | Keratoconjunctivitis sica |
| Vasculitis | BAD Carditis (30% in+ RA) |
| Digital arteritis | Pericarditis/Myocarditis |
| Ulcers | Conduction defects |
| Pyoderma gangrenosum | Coronary vasculitis Granulomatous aortitis |
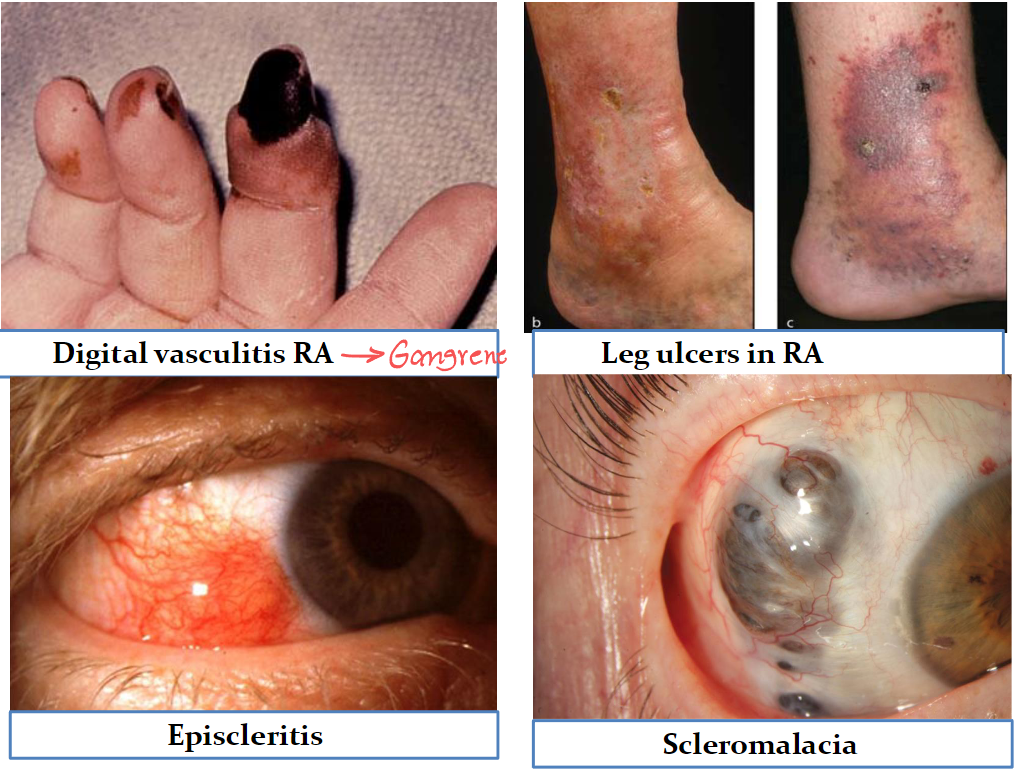
| Digital vasculitis RA →Gangrene | Leg ulcers in RA |
| Episcleritis | Scleromalacia |
Differential Diagnoses
| ❖ Fibromyalgia | ❖ Polymyalgia Rheumatica |
| ❖ Osteoarthritis | ❖ Psoriatic Arthritis |
| ❖ Polychondritis | ❖ Systemic Lupus Erythematosus (SLE) |
Treatment for RA
| Pretreatment evaluation | Treatment options RA |
|---|---|
| ❖ General testing for all patients include a baseline CBC, serum creatinine, LFT, ESR, and C-reactive protein (CRP) in all patients | ❖ NSAIDS ❖ Steroids ❖ DMARDs ❖ Non-biological ❖ Biological |
| ❖ Ophthalmologic screening for Hydroxychloroquine use | ❖ Immunosuppressive therapy ❖ Surgery |
 |
NONPHARMACOLOGIC AND PREVENTIVE THERAPIES
Briefly, these include:
- ❖ Patient education
- ❖ Psychosocial interventions
- ❖ Rest, exercise, and physical and occupational therapy
- ❖ Nutritional and dietary counseling
- ❖ Interventions to reduce risks of cardiovascular disease, including smoking cessation, and of osteoporosis
- ❖ Immunizations to decrease risk of infectious complications of immunosuppressive therapies
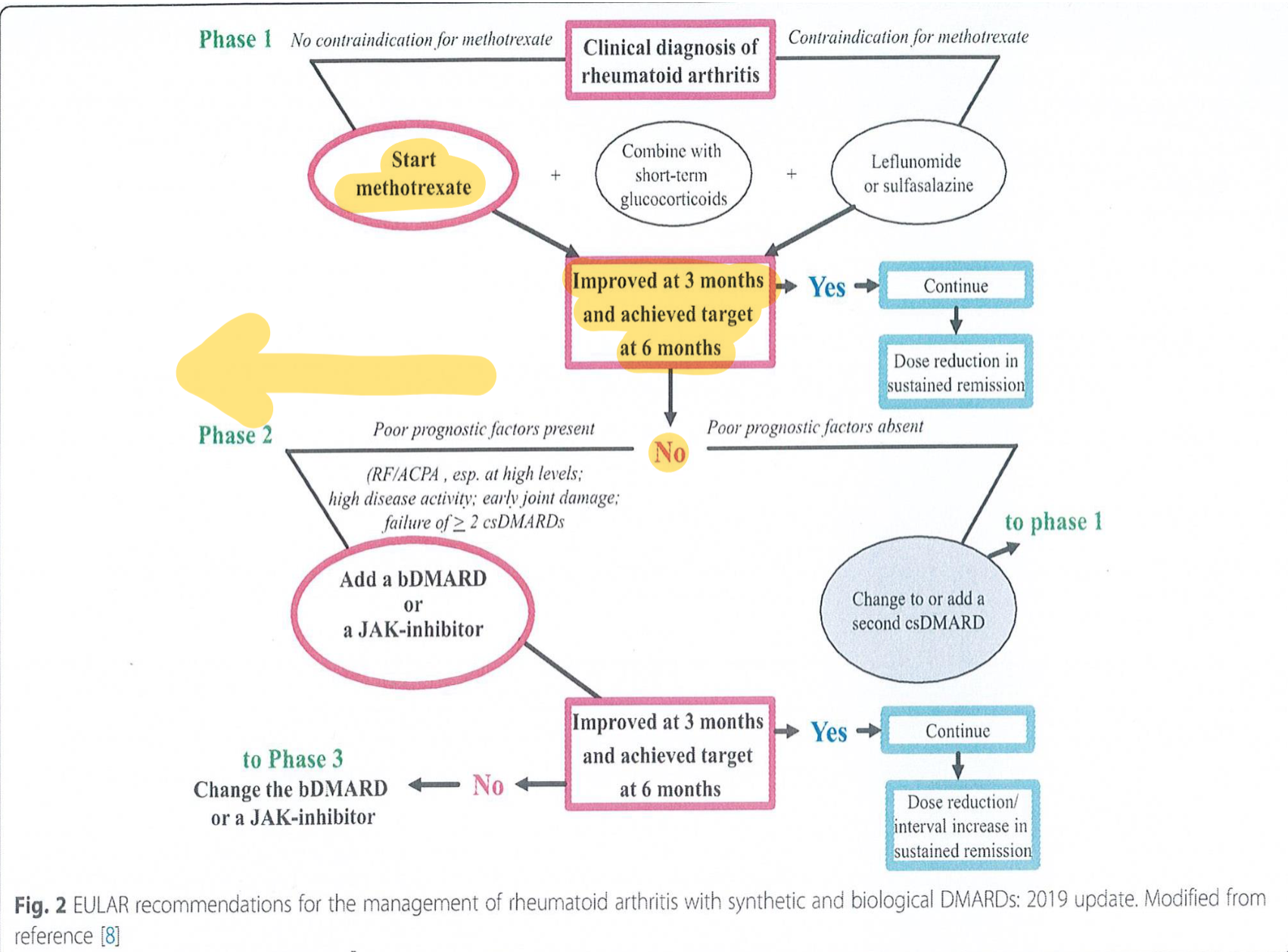
Choice of therapy
DMARDs (disease modifying antirheumatic drugs)
- Non-biologic DMARDs
- Biologic DMARDs, Start →if no improve
Non-biologic DMARDs
- Hydroxychloroquine
- Sulfasalazine
- Methotrexate
- Leflunomide
Biologic DMARDs: Produced by recombinant DNA technology
- Etanercept } TNF inhibitors
- Infliximab } TNF inhibitors
- Certolizumab} TNF inhibitors
Other agents including:
- Anakinra (human IL-1Ra)
- Rituximab
are often combined with MTX or other DMARDs to improve efficacy, generally target cytokines or their receptors.
Early use of DMARDs
| Mildly active RA |
|---|
| ❖ Initiate anti-inflammatory therapy with a NSAID for rapid symptomatic relief Begin DMARD treatment with Hydroxychloroquine (HCQ) or Sulfasalazine |
| Moderately to severe active RA |
| ❖ Initiate anti-inflammatory therapy with either a NSAID or steroids ❖ Begin DMARD therapy with Methotrexate . |
| Patients resistant to initial DMARD (e.g., MTX) |
| ❖ Treat with a combination of DMARDs (eg, MTX plus either a TNF inhibitor or SSZ and HCQ) Switch to a different DMARD (e.g., leflunomide or a TNF inhibitor), plus ant-inflammatory drug therapy. |
ASSESSMENT AND MONITORING
-
Patients should be seen on a regular basis for clinical evaluation and monitoring of clinical and laboratory assessment of disease activity and for screening for drug toxicities.
-
Patient and clinician assessment of symptoms and functional status
-
Evaluation of joint involvement and extra-articular manifestations
-
Laboratory markers
-
Imaging
Felty’s syndrome
-
Felty’s syndrome is characterized by rheumatoid arthritis, splenomegaly and neutropenia.
-
Neutropenia – Neutropenia is present in all patients, with absolute neutrophil counts below 2000/microl.
Physical Examination Z
Physical findings include:
- Splenomegaly
- Hepatomegaly (mild)
- Lymphadenopathy
- Weight loss
- Rheumatoid nodules
- Sjögren syndrome
- Articular findings of long-standing RA – Joint deformities typical of RA, as well as synovitis
Small-vessel vasculitis:
- Lower-extremity ulcers
- Palpable pupura
- Periungual infarcts
Systemic vasculitis:
- Mononeuritis multiplex
- Extremity ischemia
Other findings:
- Pleuritis
- Peripheral neuropathy
- Episcleritis
- Portal hypertension
Treatment
Immunosuppressant
- Methotrexate: It is very effective in treating rheumatoid arthritis (RA). Antirheumatic effects may take several weeks to become apparent.
- Cyclophosphamide is an antineoplastic alkylating immunosuppressive agent.
- It reduces the numbers of B and T cells and increases the risk of infection.
Hematopoietic Growth Factors Increase neutrophils since there’s neutropenia
-
Granulocyte-macrophage CSF (GM-CSF) stimulates division and maturation of earlier myeloid and macrophage precursor cells.
-
Increases granulocytes in 48–91% of patients.
Monoclonal Antibody: Rituximab
- Considered a second-line therapy in patients with refractory FS.
In Summary:
-
Rheumatoid arthritis is an autoimmune inflammatory disease primarily characterized by synovitis which is accompanied by extra-articular organ involvement, such as interstitial pneumonia, in addition to clinical symptoms including pain, swelling, stiffness of multiple joints, fever, and malaise.
-
Joint destruction progresses soon after the onset, and once the affected joints are deformed, the development of irreversible physical dysfunction is noted.
-
Thus, proper diagnosis and treatment are required from the early stages of the disease.
-
Although, palliative therapy with glucocorticoids are anti-inflammatory drugs had been used, disease-modifying antirheumatic drugs (DMARDs) are currently used to suppress immune abnormalities and to control disease activity.
-
DMARDs are classified into different groups, such as conventional synthetic DMARD, and biologic DMARD.
-
The appropriate use of these drugs has allowed remission to be the therapeutic goal in all patients
-
By maintaining remission, these drugs have also been shown to prevent the progression of joint destruction and physical dysfunction over a long period.
Imaging
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory autoimmune disorder that primarily affects the joints (e.g., causes pain, swelling, synovial destruction, deformities), The diagnosis of RA is clinical.
Perform imaging studies to further support the diagnosis and help establish disease severity.
- X-ray as the initial imaging study.
- Ultrasound and MRI might additionally be necessary to assess joint disease severity
X-ray Findings
Early: soft tissue swelling, osteopenia (juxtaarticular)
Late: joint space narrowing, marginal erosions of cartilage and bone, osteopenia (generalized), subchondral cysts
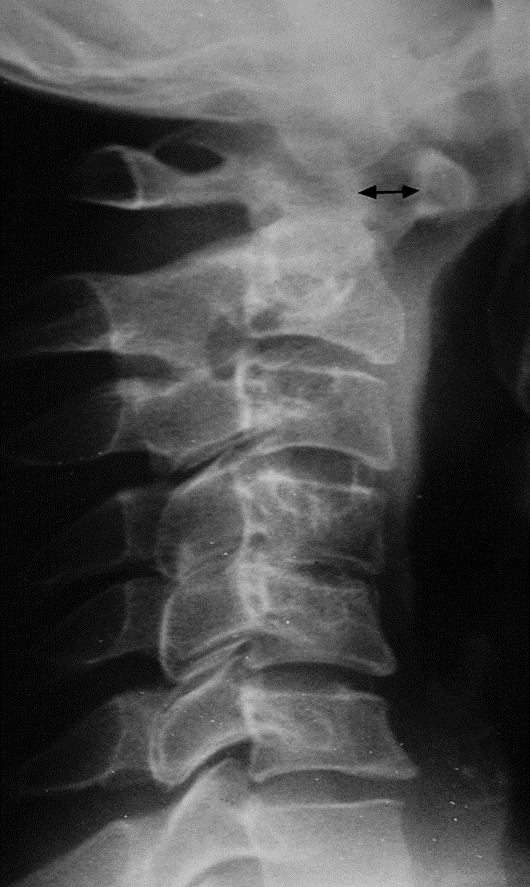
Atlantoaxial subluxation.
C1 is displaced anteriorly upon C2. The distance between the arch of the atlas and the odontoid peg (arrow) is increased from the normal value (2 mm) to 8 mm.

Rheumatoid arthritis of the wrist and hand
X-ray hands (PA view) There is generalized periarticular osteopenia (example indicated by green overlay) and narrowing of several metacarpophalangeal and proximal interphalangeal joint spaces (example indicated by green line). The marked deformity of the wrists is the result of numerous carpal, base of metacarpal, and radiocarpal erosions (red lines). Erosive scalloping (example indicated by yellow line) also involves the radioulnar joint..
Radiological sign:.
- Around joint, periarticular osteopenia/Osteoporosis
- Changes more to the proximal joints than distal
- Swan neck and Boutonnière deformity and extensive erosive
