Amphotericin B (Ambisome) is a naturally occurring polyene antifungal agent.
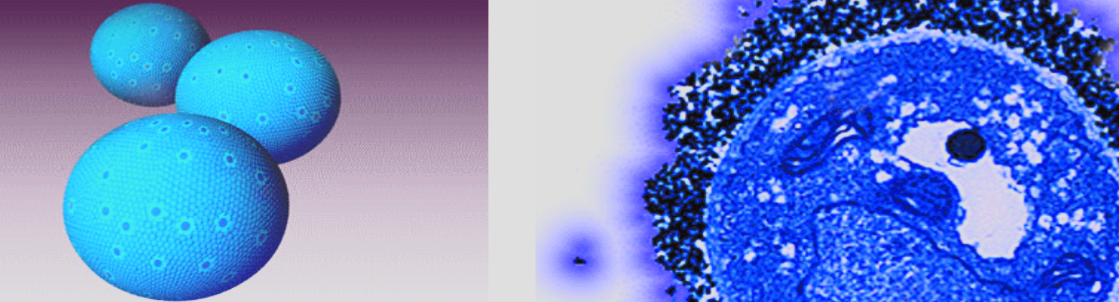
- Liposomes carry the drug.
- Fungi have lipase and cause release of drug in their cell
- Advantage: less adverse reactions
Uses:
In spite of its toxic potential, amphotericin B remains the drug of choice for the treatment of several life-threatening mycoses (systemic fungal infections).
It is effective against a wide range of fungi and many strains of Aspergillus. *Amphotericin B is also used in the treatment of the protozoal infection mucocutaneus leishmaniasis
Mechanism of action:
Amphotericin B is either fungicidal or fungistatic, depending on the organism and the concentration of the drug.
It binds to ergosterol in the plasma membranes of sensitive fungal cells. There, it forms pores (channels) that disrupt membrane function, allowing electrolytes (particularly potassium) and small molecules to leak from the cell, resulting in cell death.
Pharmacokinetic: Amphotericin B has low therapeutic index.
Amphotericin B is administered by slow, intravenous (IV) infusion. Amphotericin B is insoluble in water and must be co-formulated with either sodium deoxycholate or a variety of artificial lipids to form liposomes. The liposomal preparations have the primary advantage of reduced renal and infusion toxicity. However, due to high cost, liposomal preparations are reserved mainly as salvage therapy for patients who cannot tolerate conventional amphotericin B. - in severe systemic
Adverse effects
-
Fever and chills: These occur most commonly 1 to 3 hours after starting the IV administration but usually subside with repeated administration of the drug. Premedication with a corticosteroid or an antipyretic as paracetamol and diphenhydramine helps to prevent this problem.
-
Renal impairment: Azotemia is exacerbated by other nephrotoxic drugs, such as aminoglycosides, and vancomycin, although adequate hydration can decrease its severity. Nephrotoxicity with amphotericin B is direct effects on the distal tubule and indirect effects through vasoconstriction of the afferent arteriole cause the nephrotoxicity. This nephrotoxicity leads to (hypomagnesemia) and (hypokalemia), such that patients frequently need supplementation of these electrolytes.
-
Hypotension: A fall in blood pressure accompanied by hypokalemia may occur, requiring potassium supplementation.
-
Thrombophlebitis: The drug is irritant to the endothelium of the veins, and local thrombophlebitis after intravenous injection. Adding heparin to the infusion can alleviate this problem.
-
cardiotoxicity Y , hemolytic anemia, leukopenia, thrombocytopenia ,Anemia hepatotoxicity, and anaphylactic reactions. Intrathecal injections can cause neurotoxicity.