Psychiatry Cases, Medications & MEQs
اللهم يا معلّم موسى علّمني، ويا مفهم سليمان فهّمني، ويا مؤتي لقمان الحكمة وفصل الخطاب آتني الحكمة وفصل الخطاب اللهم اجعل ألستنا عامرة بذكرك، وقلوبنا بخشيتك، وأسرارنا بطاعتك، إنك على كل شيء قدير، حسبنا الله ونعم الوكيل
if there are any correction, changes, or addition in your notes please send me message dr.alkharji@proton.me
Updates through https://medatlax.com/Clinical/Level-10/Psychiatry/CL-Psychiatry/Psychiatry-MEQs/Psychiatry-Cases-MEQs - will be highlighted yellow
Psychiatry Cases MEQs
-
Seven cases/scenarios of cases done by roleplay/presentation
-
Each case possibly have these questions
- What is most probable diagnosis
- How would you support your diagnosis for this scenario ( 2 diagnostic criterias)
- Differential Diagnosis related to the probable diagnosis
- specific cause of such condition
- Psychopathology mentioned case above?
- What is two best investigation (setting bio-psycho-social)
- What is two best Management/Treatment (setting bio-psycho-social) bio=medications psycho=nonpharmacological - mention two for each ++ reschedule for reassessment in 1 week
~social; education, lifestyle spiritual; mindfulness exercises
Common medications
escitalo haliperadol espradol lithium sodium valporate, benzodiazepine
- Treats most cases
- Side effects?
- class
General note
any high suicidal intent should be admitted to hospital for close monitoring in cases where visual hallucination is percent CT of brain is indicated any prose intent for criminal activity should contact authorities explain why you chose your evidence diagnosis, investigations or treatment
Antidepressants
| Class | Name of Drugs | Mechanism of Action | Dosage/Duration/Time to Work | **Prelabs/Workup ** | Therapeutic Uses | Side Effects | Contraindications |
|---|---|---|---|---|---|---|---|
| Tricyclics (TCAs) | Amitriptyline, Nortriptyline, Imipramine | Inhibit the reuptake of norepinephrine and serotonin; block various receptors (antihistaminic, anticholinergic, antiadrenergic) | Typically start at low doses, titrate as needed. Time to work: 2-4 weeks imipramine 25 mg till 150 mg as required | ECG for QT prolongation, history of cardiovascular disease | Major depressive disorder, chronic pain, certain anxiety disorders | Antihistaminic (sedation, weight gain), anticholinergic (dry mouth, constipation, etc.), antiadrenergic (orthostatic hypotension), lethal in overdose, QT prolongation | Recent myocardial infarction, arrhythmias, uncontrolled hypertension, narrow-angle glaucoma, MAOI use |
| Monoamine Oxidase Inhibitors (MAOIs) | Phenelzine, Tranylcypromine, Isocarboxazid | Irreversibly inhibit monoamine oxidase, increasing levels of norepinephrine, dopamine, and serotonin | Start at low doses, gradual titration. Time to work: 2-4 weeks | Dietary restrictions (avoid tyramine-rich foods), baseline blood pressure | Major depressive disorder, atypical depression, certain anxiety disorders | Orthostatic hypotension, weight gain, dry mouth, risk of hypertensive crisis with tyramine, serotonin syndrome when combined with other serotonergic agents | Recent use of SSRIs, SNRIs, TCAs, sympathomimetics, tyramine-rich diet, uncontrolled hypertension |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | Fluoxetine, Sertraline, Escitalopram, Paroxetine | Block the presynaptic serotonin reuptake, increasing serotonin levels in the synaptic cleft | Initial doses vary by drug; 10 mg for Escitalopram, double dose for OCD cases such 20mg is indicated - time to work: 2-4 weeks for 6 months Paroxitine ~ 20 mg | Assess for history of seizures, bipolar disorder | Major depressive disorder, anxiety disorders, OCD, PTSD, panic disorder | GI upset, sexual dysfunction, insomnia, agitation, discontinuation syndrome, minimal cardiotoxicity in overdose | MAOI use, hypersensitivity to SSRIs, bipolar disorder without mood stabilizer, bleeding disorders |
| Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) | Venlafaxine, Duloxetine | Inhibit reuptake of both serotonin and norepinephrine without significant antihistaminic or anticholinergic effects | Start at low doses, titrate as needed. Time to work: 2-4 weeks venlafaxine ~ 75 mg once a day | Monitor blood pressure, assess for liver function (especially with Duloxetine) | Major depressive disorder, anxiety disorders, neuropathic pain | Hypertension, GI upset, sexual dysfunction, withdrawal symptoms, risk of serotonin syndrome | MAOI use, uncontrolled hypertension, severe liver or kidney disease, history of seizures (especially with Duloxetine) |
| Novel Antidepressants | Mirtazapine (Remeron) Bupropion (Wellbutrin) | Mirtazapine: 5HT2 and 5HT3 receptor antagonist Bupropion: Dopamine and norepinephrine reuptake inhibitor | Mirtazapine: Start low, dose-dependent sedation or activation Bupropion: Start low, avoid doses >450mg | Mirtazapine: Monitor lipid levels Bupropion: Assess seizure risk, history of eating disorders | Mirtazapine: Major depressive disorder, as hypnotic Bupropion: Major depressive disorder, ADHD, smoking cessation | Mirtazapine: Weight gain, increased cholesterol and triglycerides, sedation Bupropion: Insomnia, anxiety, seizure risk, potential for abuse | Mirtazapine: Hyperlipidemia Bupropion: Seizure disorders, eating disorders, MAOI use |
Mood Stabilizers & Anticonvulsants
| Class | Drug Name | Mechanism of Action | Dosage/Duration | Prelabs/Workup | Therapeutic Uses | Side Effects | Contraindications |
|---|---|---|---|---|---|---|---|
| Mood Stabilizer | Lithium | Modulates inositol phosphate cycle, inhibits GSK-3, and affects neurotransmitter release. | Start: 300 mg PO BID Increase: by 300 mg/day as needed Usual: 900-1500 mg/day Time to work: Steady state in ~5 days | Baseline creatinine, TSH, CBC, pregnancy test (if applicable) | Bipolar disorder (mania, depression, prophylaxis), reduces suicide rate | GI distress, thyroid abnormalities, polyuria, tremor, weight gain, cognitive slowing, nephrotoxicity, tremor, sedation | Renal impairment, severe cardiovascular disease |
| Mood Stabilizer | Valproic acid | Increases GABA levels, inhibits sodium and calcium channels, and modulates neurotransmitter release. | Target Level: 50-125 µg/ml Time to work: Steady state in ~4-5 days | Liver function tests, CBC, pregnancy test, folic acid supplement (women) | Bipolar disorder (mania prophylaxis), rapid cycling, mixed episodes | Thrombocytopenia, weight gain, nausea, hepatotoxicity, tremor, increased risk of neural tube defects, hair loss, in rare cases may result in pancreatitis | Liver disease, urea cycle disorders, pregnancy (trimester specific) |
| Anticonvulsant | Carbamazepine (Tegretol) | Blocks voltage-gated sodium channels, stabilizing hyperexcited neural membranes, reduces synaptic transmission. | Target Level: 4-12 µg/ml Start: Dose individualized Time to work: Steady state in ~5 days Duration: Ongoing with monitoring | Liver function tests, CBC, EKG | Acute mania, mania prophylaxis, rapid cycling, mixed episodes | Rash, dizziness, sedation, ataxia, hyponatremia, aplastic anemia, hepatotoxicity, AV conduction delays | Bone marrow suppression history, severe hepatic impairment |
| Anticonvulsant | Lamotrigine (Lamictal) | Inhibits voltage-sensitive sodium channels, stabilizes neuronal membranes, modulates glutamate release. | Initiation: 25 mg daily for 2 weeks Titration: Increase to 50 mg/day for 2 weeks, then to 100 mg/day Time to work: Weeks to months | None specific beyond standard precautions | Bipolar disorder (prevention of depressive episodes), maintenance therapy | Rash (including Stevens-Johnson Syndrome), dizziness, headache, diplopia, ataxia, nausea, insomnia | History of serious rash with lamotrigine, hypersensitivity |
Antipsychotics
Psychiatry Medications Overview
| Name of Drugs | Mechanism of Action | Dosage/Duration/Time to Work | Prelabs/Workup Prior to Use | Therapeutic Uses | Side Effects | Contraindications |
|---|---|---|---|---|---|---|
| Clozapine (Clozaril) | Serotonin-dopamine antagonist; primarily blocks D2 receptors | Initiate at low dose, titrate as needed; therapeutic effects usually seen within 1-2 weeks | Complete blood count (CBC) monitoring due to risk of agranulocytosis | Treatment-resistant schizophrenia, suicidal behavior in schizophrenia or schizoaffective disorder | Agranulocytosis, seizures, sedation, weight gain, hyperglycemia, hyperlipidemia, myocarditis | History of clozapine-induced agranulocytosis, severe cardiovascular disease |
| Risperidone | Dopamine D2 and serotonin 5-HT2A receptor antagonist | Typical dose: 1-16 mg/day at night; onset within 1-2 weeks - | Metabolic panel, CBC | Schizophrenia, bipolar disorder, irritability in autistic children | Extrapyramidal symptoms (EPS), hyperprolactinemia, weight gain, sedation | Parkinson’s disease, prolactinoma, severe CNS depression |
| Olanzapine | Dopamine D2 and serotonin 5-HT2A receptor antagonist | Typical dose: 5-20 mg/day; onset within 1-2 weeks | Metabolic panel, CBC | Schizophrenia, bipolar disorder | Weight gain, metabolic syndrome, sedation, EPS | Diabetes mellitus, history of thrombotic events, severe cardiovascular disease |
| Quetiapine | Dopamine D2 and serotonin 5-HT2A receptor antagonist; also affects histamine and adrenergic receptors | Typical dose: 150-750 mg/day; onset within 1-2 weeks | Metabolic panel, CBC | Schizophrenia, bipolar disorder, major depressive disorder (as adjunct) | Sedation, weight gain, metabolic changes, orthostatic hypotension | Hypersensitivity to quetiapine, severe CNS depression |
| Haloperidol | High-affinity dopamine D2 receptor antagonist | Typical dose: 0.5-10 mg/day; onset within hours for acute psychosis | ECG, especially QT interval monitoring | Acute psychosis, Tourette syndrome, severe behavioral problems in children | Extrapyramidal symptoms (EPS), tardive dyskinesia, QT prolongation, sedation | Parkinson’s disease, bradycardia, epilepsy, severe CNS depression |
Antipsychotics as mood stabilizers
FDA approved indications in Bipolar disorder
| Generic name | Trade name | Manic | Mixed | Maintenance | Depressed |
|---|---|---|---|---|---|
| Aripiprazole | Abilify | x | x | x | |
| Ziprasidone | Geodon | x | x | X* | |
| Risperdone | Risperdal | x | x | ||
| Asenapine | Saphris | x | x | ||
| Quetiapine | Seroquel | x | X* | ||
| Quetiapine XR | Seroquel XR | x | X* | x | |
| Chlorpromazine | Thorazine | x | |||
| Olanzapine | Zyprexa | x | x | x | |
| Olanzapine/fluoxetine comb | Symbyax | x |
Anxiolytics and benzodiazepines
| Class | Name of Drugs | Mechanism of Action | Dosage/Duration/Time to Work | Prelabs/Workup Prior to Medications | Therapeutic Uses | Side Effects | Contraindications |
|---|---|---|---|---|---|---|---|
| Anxiolytics | Buspirone, Hydroxyzine | Buspirone: Partial agonist at 5-HT₁A receptors Hydroxyzine: H₁ histamine receptor antagonist | Buspirone: 15-30 mg/day, several weeks for effect Hydroxyzine: 25-100 mg 3-4 times daily | Assess for MAOI use, bipolar disorder, allergy history | Generalized Anxiety Disorder, Panic Disorder, Insomnia | Dizziness, headache, sedation, dry mouth | MAOI use (for Buspirone), glaucoma, severe liver impairment |
| Benzodiazepines | Diazepam, Lorazepam, Alprazolam | Enhance inhibitory neurotransmission by increasing GABAₐ receptor affinity | Varies by drug: • Diazepam: 2-10 mg 2-4 times daily • Lorazepam: 0.5-2 mg 2-3 times daily • Alprazolam: 0.25-0.5 mg 3 times daily | History of substance abuse, respiratory issues, hepatic function | Anxiety Disorders, Insomnia, Seizure Control, Alcohol Withdrawal | Somnolence, cognitive deficits, amnesia, tolerance, dependence | Acute narrow-angle glaucoma, severe respiratory insufficiency, hypersensitivity to benzodiazepines |
| Flumazenil | Flumazenil | Competitive antagonist at the benzodiazepine binding site of GABAₐ receptors in the CNS | 0.2 mg IV over 15 seconds, may repeat every minute up to total of 3 mg | Assess for benzodiazepine use, seizure history | Reversal of benzodiazepine overdose | Seizures (in prolonged benzodiazepine use), anxiety, tremors | Chronic benzodiazepine use, known seizure disorder, hypoventilation |
Bipolar Therapeutics
| Class | Name of Drugs | Mechanism of Action | Dosage/Duration/Time to Work | Prelabs Workup Prior Medications | Therapeutic Uses | Side Effects | Contraindications |
|---|---|---|---|---|---|---|---|
| Mood Stabilizers | Lithium | Alters sodium transport in neurons, modulates neurotransmission | Start at 300 mg PO BID, usual 900-1500 mg/day, steady state in ~5 days | Baseline creatinine, TSH, CBC, pregnancy test for women | Anti-manic, anti-depressant, prophylaxis | GI distress, thyroid abnormalities, polyuria, weight gain, tremor, cognitive slowing, nephrotoxicity | Renal impairment, pregnancy (risk of Ebstein’s anomaly) |
| Valproic Acid | Increases GABA levels, inhibits sodium and calcium channels | Start at 250 mg BID, increase weekly by 250 mg, therapeutic levels 350-700 μmol/L | History and physical, LFTs, CBC with platelets | Manic episodes, bipolar depression, prophylaxis | GI distress, sedation, hepatotoxicity, thrombocytopenia, weight gain, tremor, polycystic ovarian disease | Liver disease, polycystic ovarian syndrome | |
| Lamotrigine | Inhibits voltage-sensitive sodium channels, stabilizes neuronal membranes | Start at 12.5-25 mg PO daily, increase biweekly by 12.5-25 mg, usual 50-200 mg/day | None specific, monitor for rash | Depression, prophylaxis | Rash (Stevens-Johnson), dizziness, headache, blurred vision | History of Stevens-Johnson syndrome | |
| Carbamazepine | Blocks sodium channels, stabilizes hyperexcited nerve membranes | Start at 100 mg BID, increase by 200 mg every 5 days, usual 800-1000 mg/day | History and physical, CBC with diff, platelets, LFTs | Mania, bipolar depression, prophylaxis | Dizziness, ataxia, sedation, diplopia, nausea, rashes, hyponatremia, agranulocytosis, hepatic failure | Bone marrow suppression, hepatic impairment | |
| Atypical Neuroleptics | Olanzapine | Dopamine and serotonin receptor antagonism | 5-20 mg/day | None specific | Mania, depression, prophylaxis | Weight gain, increased glucose/triglycerides, sedation, extrapyramidal symptoms | Metabolic syndrome, diabetes mellitus |
| Risperidone | Dopamine D2 and serotonin 5-HT2A receptor antagonist | 1-4 mg/day | None specific | Mania, psychosis | Extrapyramidal symptoms, weight gain, sedation, prolactin elevation | Parkinson’s disease, prolactin-related conditions | |
| Quetiapine | Dopamine D2 and serotonin 5-HT2A receptor antagonist | 200-800 mg/day | None specific | Mania, psychosis | Sedation, weight gain, metabolic changes, orthostatic hypotension | ||
| Aripiprazole | Partial agonist at dopamine D2 and serotonin 5-HT1A receptors, antagonist at 5-HT2A | 10-15 mg/day | None specific | Mania, psychosis | Akathisia, insomnia, nausea, vomiting, dizziness | ||
| Ziprasidone | Dopamine D2 and serotonin 5-HT2A receptor antagonist | 20-80 mg BID | None specific | Mania, psychosis | QT prolongation, sedation, extrapyramidal symptoms, headache |
medication doses for all above being examples or range and needing individualization depending on case.
Stimulants in cases of ADHD
-
Stimulant medications – Ritalin, Dexedrine.
-
Reduced impulsiveness and hyperactivity and improved attention.
-
NARI, atomoxetine.
-
Parents and teachers must be advised on how to cope with hyperactive children.
-
Nootropic drugs and mild doses of antipsychotics are sometimes prescribed.
-
Stimulant drugs such as methylphenidate sometimes have the paradoxical effect, according to theory, that stimulants act by reducing the excessive, poorly synchronized variability in the various dimensions of arousal and reactivity seen in ADHD.
-
Stimulants are the drugs of first choice.
side effects dry mouth, palpitation, insomnia
Others
Propranolol ~ 10-20mg (sideeffects; orthostatic hypotension) used in PTSD/ASD conditions Donepezil for dementia Diazepam + Thiamine for Delirium tremens
Cases
Psychosomatic Medicine
Case 1: Perinatal Psychiatry
Case Scenario:
Jane, a 28-year-old woman in her third trimester, has been experiencing intense anxiety and depressive symptoms following her first pregnancy. She reports persistent fears about harming her baby and difficulties in bonding.
-
What is the most probable diagnosis?
Major Depressive Disorder with peripartum onset / Perinatal Depression - postpartum depression if symptoms appear after birth -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Depressed mood most of the day, nearly every day.
- Diminished interest in activities, including bonding with the baby.
-
Differential Diagnosis related to the probable diagnosis:
Postpartum Psychosis, Generalized Anxiety Disorder -
Mention likely specific cause of such condition?
Hormonal fluctuations during pregnancy and postpartum period. -
Psychopathology mentioned case above?
Anxiety and depressive symptoms affecting maternal functioning. -
What are two best investigations?
- Hormonal level assessments
- Psychological evaluation for depression and anxiety
-
What are two best Management/Treatment?
- SSRIs (e.g., Sertraline 50 mg daily, 4-6 weeks intial, for 6 month)
- Cognitive Behavioral Therapy (12-16 sessions)
- Social support, support groups, education
Case Scenario:
A 28-year-old woman, 32 weeks pregnant, presents with persistent feelings of sadness, fatigue, and lack of interest in activities she once enjoyed. She reports difficulty sleeping, changes in appetite, and occasional thoughts of harming herself and her baby. These symptoms began six weeks after delivery.
-
What is the most probable diagnosis?
Postpartum Depression -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Presence of depressive symptoms such as persistent sadness, fatigue, and lack of interest lasting more than two weeks.
- Onset of symptoms within four weeks after delivery.
-
Differential Diagnosis related to the probable diagnosis
Postpartum “Baby Blues”, Bipolar Disorder, Anxiety Disorders -
Mention likely specific cause of such condition?
Hormonal changes postpartum combined with psychosocial stressors. -
Psychopathology mentioned case above?
Major Depressive Disorder -
What is two best investigation (biological, psychological, social investigations)
- Psychological: Clinical interview for depression assessment.
- Biological: Thyroid function tests to rule out thyroid-related mood disorders.
-
What is two best Management/Treatment (biological; dose, duration, time to work) (psychological & social investigations)
- Biological:
- SSRIs (e.g., Sertraline 50 mg daily for 6 months)
- Duration: Minimum 6 months of treatment
- Psychological & Social:
- Cognitive Behavioral Therapy (CBT)
- Social Support: Engaging family support and support groups
- Biological:
Case 2: SSD - Somatic Symptoms and Related Disorders
Case Scenario:
Mark, a 35-year-old male, presents with multiple, persistent physical complaints such as chronic pain and gastrointestinal issues without a clear medical cause. He is excessively worried about his symptoms and frequently seeks medical attention. A 45-year-old female presents with multiple, recurrent, and unexplained physical symptoms, including chronic pain and fatigue, which significantly interfere with her daily functioning. She frequently visits various specialists and is preoccupied with the belief that she has a serious undiagnosed illness despite extensive medical evaluations showing no evidence of such conditions.
-
What is the most probable diagnosis?
Somatic Symptom Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- One or more somatic symptoms that are distressing and/or result in significant disruption of daily life.
- Excessive thoughts, feelings, or behaviors related to the somatic symptoms.
-
Differential Diagnosis related to the probable diagnosis:
Illness Anxiety Disorder (Hypochondriasis) , Factitious Disorder, conversion disorder, SLE -
Mention likely specific cause of such condition?
Psychological stress and heightened bodily awareness. -
Psychopathology mentioned case above?
Emotional arousal and maladaptive interpretation of bodily sensations. -
What are two best investigations?
- Comprehensive medical evaluation to rule out underlying conditions, if all investigation were done prior with other doctors with no findings prior most likely is false, and no investigation is done unless warranted.
- Psychological assessment for anxiety and depression
-
What are two best Management/Treatment?
- SSRIs (e.g., Escitalopram 10 mg daily, 6-8 weeks) ; Dry mouth and decreased libido
- Cognitive Behavioral Therapy
Case 3: IAD - Illness Anxiety Disorder
Case Scenario:
Lisa, a 40-year-old woman, is preoccupied with having a serious illness despite medical evaluations showing no evidence. She frequently checks her body for signs of disease and avoids medical appointments out of fear. A 35-year-old male is excessively worried about having a serious heart condition despite multiple negative cardiac tests and reassurances from his physician. He frequently checks his pulse, avoids physical activities fearing they might trigger a heart attack, and often seeks unnecessary medical consultations.
-
What is the most probable diagnosis?
Illness Anxiety Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Preoccupation with having or acquiring a serious illness. despite absence of significant somatic symptoms. High level of anxiety about health, with excessive health-related behaviors such as frequent check-ups and avoidance of activities.
- Excessive health-related behaviors or maladaptive avoidance.
-
Differential Diagnosis related to the probable diagnosis:
Somatic Symptom Disorder, Generalized Anxiety Disorder, OCD -
Mention likely specific cause of such condition?
High health-related anxiety and cognitive distortions about illness. -
Psychopathology mentioned case above?
Severe health-related anxiety without significant physical symptoms. -
What are two best investigations?
- Medical evaluation to rule out physical illnesses if warranted, basic screening done such cbc to r/o infection if there is suspicion
- Psychological assessment for anxiety disorders
-
What are two best Management/Treatment?
- SSRIs (e.g., Fluoxetine 20 mg daily, 6-12 weeks)
- Cognitive Behavioral Therapy (16-20 sessions)
Case 4: Conversion Disorder
Case Scenario:
Tom, a 22-year-old male, abruptly loses the ability to speak and experiences partial paralysis of his right arm following a traumatic event. Medical tests reveal no neurological abnormalities. A 22-year-old female college student experiences sudden onset of paralysis in her right arm following a highly stressful exam period. Neurological examinations and imaging studies reveal no physical abnormalities. Her symptoms are inconsistent with known neurological conditions.
-
What is the most probable diagnosis?
Conversion Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- One or more symptoms of altered voluntary motor function (paralysis) incompatible with recognized neurological conditions.
- Clinical findings provide evidence of incompatibility between the symptom and neurological or medical conditions.
-
Differential Diagnosis related to the probable diagnosis:
Stroke, Multiple Sclerosis, Guillain-Barré Syndrome -
Mention likely specific cause of such condition?
Psychological stress manifesting as physical symptoms. -
Psychopathology mentioned case above?
Conversion of psychological stress into physical paralysis. -
What are two best investigations?
- Neurological examination and imaging MRI to r/o structural abnormalities
- Psychological evaluation for trauma and stress
-
What are two best Management/Treatment?
-
- SSRIs if anxiety or depression is present (e.g., Sertraline 50 mg daily)
- Physical therapy as needed
- Trauma-focused Cognitive Behavioral Therapy
-
Case 5: PFAOMC - Psychological Factors Affecting Other Medical Conditions
Case Scenario:
Sarah, a 50-year-old diabetic patient, has poor glycemic control attributed to her significant stress from work and family issues. Her psychological state is negatively impacting her medical condition management. A 60-year-old male with Type 2 Diabetes Mellitus demonstrates poor adherence to his insulin regimen and frequently misses medical appointments. He expresses feelings of hopelessness and denies the benefits of his treatment, leading to uncontrolled blood glucose levels and recurrent infections.
-
What is the most probable diagnosis?
Psychological Factors Affecting Other Medical Conditions (PFAOMC) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a medical condition (Type 2 Diabetes Mellitus).
- Psychological factors adversely affecting the course of the medical condition through poor treatment adherence and emotional distress.
-
Differential Diagnosis related to the probable diagnosis:
Adjustment Disorder, Major Depressive Disorder, Substance Use Disorder, Cognitive Impairment -
Mention likely specific cause of such condition?
Chronic stress and inadequate coping mechanisms affecting disease management. -
Psychopathology mentioned case above?
Stress and potential depressive symptoms interfering with self-care. -
What are two best investigations?
- Glycemic monitoring and medical evaluation
- Psychological assessment for stress and coping strategies
-
What are two best Management/Treatment?
- Adjustment of diabetes treatment plan as needed
-
- Antidepressants such as SSRIs (e.g., Escitalopram 10 mg daily for 6 months)
-
- Cognitive Behavioral Therapy (CBT)
- Patient education and support groups to improve adherence
Case 6: Factitious Disorder
Case Scenario:
Michael, a 30-year-old healthcare worker, frequently presents with self-induced symptoms such as gastrointestinal pain and seizures. Medical evaluations cannot find an organic cause, and he seems eager to undergo invasive procedures. A 30-year-old female medical student frequently presents to emergency departments with various self-induced symptoms, including simulated seizures and self-inflicted wounds. Multiple hospitalizations reveal inconsistent histories and evidence of deceptive behavior without any external rewards.
-
What is the most probable diagnosis?
Factitious Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Intentional production or feigning of physical or psychological symptoms.
- Deception evident in the presentation, without external incentives.
-
Differential Diagnosis related to the probable diagnosis:
Malingering, Somatic Symptom Disorder -
Mention likely specific cause of such condition?
Psychological need to assume the sick role for internal gratification. -
Psychopathology mentioned case above?
Manipulative behavior to receive medical attention. -
What are two best investigations?
- Comprehensive medical evaluation to identify fabricated symptoms, if it were already investigated by numerous doctors without any findings dont do it.
- Psychiatric assessment for underlying personality disorders
-
What are two best Management/Treatment?
- Psychotherapy, particularly Cognitive Behavioral Therapy (ongoing)
- Establishing a therapeutic relationship to address underlying issues
Personality disorders
Case 1: Cluster A - Paranoid Personality Disorder
Case Scenario:
John, a 45-year-old accountant, believes that his coworkers are plotting against him to undermine his position. He constantly looks over his shoulder, rarely shares personal information, and reacts aggressively to perceived slights.
-
What is the most probable diagnosis?
Paranoid Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Pervasive mistrust and suspicion of others’ motives
- Reluctance to confide in others due to fear of betrayal
-
Differential Diagnosis related to the probable diagnosis
Delusional Disorder, Schizophrenia -
Mention likely specific cause of such condition?
Genetic predisposition and early childhood experiences of mistrust -
Psychopathology mentioned case above?
Persistent distrust and hypervigilance towards others -
What is two best investigation
- Comprehensive psychological assessment
- Family history evaluation
-
What is two best Management/Treatment
- Cognitive Behavioral Therapy (CBT)
- Social skills training
Case 2: Cluster A - Schizoid Personality Disorder
Case Scenario:
Lisa, a 30-year-old graphic designer, prefers working alone and shows little interest in forming friendships. She rarely expresses emotions and seems indifferent to praise or criticism.
-
What is the most probable diagnosis?
Schizoid Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Detachment from social relationships
- Restricted range of emotional expression
-
Differential Diagnosis related to the probable diagnosis
Avoidant Personality Disorder, Autism Spectrum Disorder -
Mention likely specific cause of such condition?
Genetic factors and early emotional neglect -
Psychopathology mentioned case above?
Emotional coldness and preference for solitary activities -
What is two best investigation
- Psychological evaluation for social functioning
- Genetic history assessment
-
What is two best Management/Treatment
- Psychodynamic therapy
- Social skills training
Case 3: Cluster A - Schizotypal Personality Disorder
Case Scenario:
Mark, a 28-year-old artist, has unusual beliefs in supernatural phenomena and experiences odd perceptual distortions. He has few close friends and displays eccentric behavior in social settings.
-
What is the most probable diagnosis?
Schizotypal Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Peculiar thinking and odd beliefs
- Social anxiety and limited interpersonal relationships
-
Differential Diagnosis related to the probable diagnosis
Schizophrenia, Bipolar Disorder -
Mention likely specific cause of such condition?
Genetic vulnerability and early life stressors -
Psychopathology mentioned case above?
Eccentric behavior and unusual perceptual experiences -
What is two best investigation
- Comprehensive psychiatric evaluation
- Family history of psychotic disorders
-
What is two best Management/Treatment
- Low-dose antipsychotic medication
- Cognitive Behavioral Therapy (CBT)
QT prolongation and Extrapyramidal are known side effects of antipsychotic
Case 4: Cluster B - Antisocial Personality Disorder
Case Scenario:
Tom, a 35-year-old with a history of criminal activities, frequently engages in deceitful behavior and shows no remorse for his actions. He often disregards the rights and feelings of others.
-
What is the most probable diagnosis?
Antisocial Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Persistent disregard for the rights of others
- Deceitfulness and manipulative behavior
-
Differential Diagnosis related to the probable diagnosis
Borderline Personality Disorder, Narcissistic Personality Disorder -
Mention likely specific cause of such condition?
Genetic factors and childhood abuse or neglect -
Psychopathology mentioned case above?
Lack of remorse and manipulative tendencies -
What is two best investigation
- Criminal history review
- Psychological assessment for impulsivity
-
What is two best Management/Treatment
- Dialectical Behavior Therapy / Cognitive Behavioral Therapy (CBT)
- Social rehabilitation programs
Case 5: Cluster B - Borderline Personality Disorder
Case Scenario:
Sarah, a 25-year-old woman, experiences intense and unstable relationships. She exhibits impulsive behaviors, such as reckless spending and substance abuse, and frequently engages in self-harm. Sara, a 25-year-old woman, experiences intense and unstable relationships. She exhibits impulsive behaviors and frequently engages in self-harm when feeling abandoned.
-
What is the most probable diagnosis?
Borderline Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Intense and unstable interpersonal relationships
- Impulsivity in potentially self-harm
-
Differential Diagnosis related to the probable diagnosis
Bipolar Disorder, Post-Traumatic Stress Disorder -
Mention likely specific cause of such condition?
Childhood trauma and genetic predisposition -
Psychopathology mentioned case above?
Emotional instability and self-harm behaviors -
What is two best investigation
- Comprehensive psychological evaluation
- Assessment of trauma history
-
What is two best Management/Treatment
- Dialectical Behavior Therapy (DBT)
- Medications for mood stabilization (e.g., SSRIs)
- Couples therapy
Case 6: Cluster B - Histrionic Personality Disorder
Case Scenario:
Emma, a 30-year-old actress, seeks constant attention and becomes uncomfortable when not the center of attention. She uses her appearance and theatrical behavior to draw focus in social interactions.
-
What is the most probable diagnosis?
Histrionic Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Excessive attention-seeking behavior
- Inappropriately seductive or provocative behavior
-
Differential Diagnosis related to the probable diagnosis
Narcissistic Personality Disorder, Borderline Personality Disorder -
Mention likely specific cause of such condition?
Early childhood experiences and genetic factors -
Psychopathology mentioned case above?
Dramatic and attention-seeking actions -
What is two best investigation
- Psychological assessment for attention-seeking behaviors
- Social history review
-
What is two best Management/Treatment
- CBT
- Group therapy
Case 7: Cluster B - Narcissistic Personality Disorder
Case Scenario:
Robert, a 40-year-old executive, has an inflated sense of self-importance and expects special treatment. He lacks empathy and often exploits others to achieve his goals.
-
What is the most probable diagnosis?
Narcissistic Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Grandiose sense of self-importance
- Lack of empathy for others
-
Differential Diagnosis related to the probable diagnosis
Antisocial Personality Disorder, Histrionic Personality Disorder -
Mention likely specific cause of such condition?
Genetic predisposition and childhood environment -
Psychopathology mentioned case above?
Exploitative behavior and entitlement -
What is two best investigation
- Comprehensive personality assessment
- Evaluation of interpersonal relationships
-
What is two best Management/Treatment
- Psychotherapy focusing on empathy development
- Cognitive Behavioral Therapy (CBT)
- Relationship counseling
Case 8: Cluster C - Avoidant Personality Disorder
Case Scenario:
Alice, a 29-year-old teacher, avoids social gatherings due to intense fear of criticism. She feels inadequate and restricts her career choices to roles that require minimal interaction.
-
What is the most probable diagnosis?
Avoidant Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Feelings of inadequacy and hypersensitivity to negative evaluation
- Avoidance of social interactions despite desire for relationships
-
Differential Diagnosis related to the probable diagnosis
Schizoid Personality Disorder, Social Anxiety Disorder -
Mention likely specific cause of such condition?
Genetic factors and early experiences of rejection -
Psychopathology mentioned case above?
Social inhibition and extreme sensitivity to criticism -
What is two best investigation
- Psychological assessment for anxiety
- Social history evaluation
-
What is two best Management/Treatment
- Cognitive Behavioral Therapy (CBT)
- Group therapy for social skills
Case 9: Cluster C - Dependent Personality Disorder
Case Scenario:
Michael, a 32-year-old nurse, relies heavily on his partner for decision-making. He fears abandonment and feels helpless when alone, often making submissive choices to keep his relationship intact.
-
What is the most probable diagnosis?
Dependent Personality Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Excessive need to be taken care of
- Difficulty making everyday decisions without reassurance
-
Differential Diagnosis related to the probable diagnosis
Borderline Personality Disorder, Avoidant Personality Disorder -
Mention likely specific cause of such condition?
Early childhood dependency and lack of autonomy -
Psychopathology mentioned case above?
Submissive behavior and fear of separation -
What is two best investigation
- Psychological evaluation for dependency issues
- Social support system assessment
-
What is two best Management/Treatment
- Cognitive Behavioral Therapy (CBT)
- Skills training for independence/ Assertiveness training
Case 10: Cluster C - Obsessive-Compulsive Personality Disorder
Case Scenario:
Karen, a 38-year-old librarian, is excessively devoted to work and perfectionism. She struggles with delegating tasks and spends long hours organizing books, often neglecting leisure activities.
-
What is the most probable diagnosis?
Obsessive-Compulsive Personality Disorder (OCPD) NOT OCD -
Unlike obsessive-compulsive disorder, individuals with OCPD do not necessarily have obsessions or compulsions.
-
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Preoccupation with orderliness, perfectionism
- Inflexibility and control over work and relationships
-
Differential Diagnosis related to the probable diagnosis
Obsessive-Compulsive Disorder, Autism Spectrum Disorder -
Mention likely specific cause of such condition?
Genetic factors and early life experiences emphasizing perfection -
Psychopathology mentioned case above?
Rigidity in routines and excessive focus on details -
What is two best investigation
- Psychological personality assessment for perfectionism
- Occupational history review
-
What is two best Management/Treatment
- Cognitive Behavioral Therapy (CBT)
- Relaxation techniques and stress management training
Childhood mental disorders
Case 1: Separation Anxiety Disorder of Childhood
Case Scenario:
Emma, a 9-year-old girl, becomes extremely distressed when her mother leaves for work. She frequently complains of headaches and stomachaches to avoid going to school. Emma refuses to attend classes and becomes tearful at the thought of separation from her mother.
-
What is the most probable diagnosis?
Separation Anxiety Disorder (SAD) of Childhood -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Excessive fear or anxiety concerning separation from attachment figures.
- Persistent reluctance or refusal to go to school despite academic performance.
-
Differential Diagnosis related to the probable diagnosis
Generalized Anxiety Disorder, School Refusal due to other reasons, Adjustment Disorder -
Mention likely specific cause of such condition?
Genetic predisposition and environmental factors such as recent family changes or stressors. -
Psychopathology mentioned case above?
Anxiety related to separation and avoidance behavior. -
What is two best investigation
- Psychological assessment through structured interviews.
- Evaluation of family dynamics and recent life stressors.
-
What is two best Management/Treatment
- Cognitive Behavioral Therapy (12-16 weeks) to address anxiety symptoms.
- Family therapy to improve family relationships and support systems.
Case 2: ADHD
Case Scenario:
Liam, a 7-year-old boy, is constantly fidgeting in class, interrupts his teacher frequently, and has difficulty completing his homework. His parents report that he is easily distracted and often forgets to bring his school materials home.
-
What is the most probable diagnosis?
Attention-Deficit/Hyperactivity Disorder (ADHD) -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Hyperactivity and impulsivity evidenced by constant fidgeting and interrupting.
- Inattention demonstrated by difficulty completing tasks and being easily distracted.
-
Differential Diagnosis related to the probable diagnosis
Oppositional Defiant Disorder, Anxiety Disorders, Learning Disabilities -
Mention likely specific cause of such condition?
Genetic mutations in dopamine receptor and transporter genes. -
Psychopathology mentioned case above?
Impulsivity, hyperactivity, and inattention affecting academic performance and social interactions. -
What is two best investigation
- Neuropsychological testing to assess attention and executive functions.
- Family history evaluation for genetic factors.
-
What is two best Management/Treatment
- Stimulant medications (Ritalin, Dexedrine, NARI, atomoxetine)
- Cognitive Behavioral therapy to develop coping strategies and improve self-regulation.
Nausea, vomiting, headache, insomnia which are common side effects of stimulant medications like Ritalin.
Case 3: Conduct Disorder
Case Scenario:
Jake, a 12-year-old boy, frequently engages in aggressive behavior toward peers, including bullying and physical fights. He has a history of stealing items from stores and lying to cover his actions. His parents have noticed a decline in his behavior since the introduction of a new stepfather.
-
What is the most probable diagnosis?
Conduct Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Aggressive behavior towards people and animals, such as bullying and fighting.
- Deceitfulness or theft, evidenced by stealing and lying.
-
Differential Diagnosis related to the probable diagnosis
Oppositional Defiant Disorder, ADHD, Substance Use Disorders -
Mention likely specific cause of such condition?
Dysfunctional family environment and disruption of attachment due to new family member. -
Psychopathology mentioned case above?
Aggressive and antisocial behavior disrupting social and familial relationships. -
What is two best investigation
- Comprehensive behavioral assessment through clinical interviews.
- Evaluation of family dynamics and history of abuse or neglect.
-
What is two best Management/Treatment
- Family therapy to enhance emotional support and understanding (12-20 sessions).
- Behavioral interventions and possibly court-mandated supervised residence if necessary.
Case 4: Autism Spectrum Disorder (ASD)
Case Scenario:
Sophia, a 3-year-old girl, shows limited eye contact and prefers to play alone with her toys. She engages in repetitive hand-flapping movements and becomes extremely upset when her daily routine is altered. Sophia has difficulty communicating her needs and often responds to questions with non-verbal gestures.
-
What is the most probable diagnosis?
Autism Spectrum Disorder (ASD) -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Persistent deficits in social communication and social interaction.
- Restricted, repetitive patterns of behavior, interests, or activities.
-
Differential Diagnosis related to the probable diagnosis
Social (Pragmatic) Communication Disorder, Developmental Coordination Disorder, Intellectual Disability -
Mention likely specific cause of such condition?
Abnormalities in brain and central nervous system development, possibly genetic and environmental factors. -
Psychopathology mentioned case above?
Impaired social interaction, communication difficulties, and repetitive behaviors affecting daily functioning. -
What is two best investigation
- Comprehensive developmental evaluation by a multidisciplinary team.
- Genetic testing to rule out associated genetic conditions.
-
What is two best Management/Treatment
- Applied Behavior Analysis (ABA) therapy (intensive, 20-40 hours per week) to improve social and communication skills.
- Speech and occupational therapy to address communication challenges and sensory sensitivities.
Anxiety & OCD
Case 1: Panic Disorder
Case Scenario:
John, a 34-year-old male, experiences sudden and recurrent panic attacks characterized by heart palpitations, shortness of breath, and fear of losing control. These episodes occur unexpectedly and have led him to avoid certain places where he previously had attacks.
-
What is the most probable diagnosis?
Panic Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Recurrent unexpected panic attacks
- persistent concern about additional attacks
-
Differential Diagnosis related to the probable diagnosis
Generalized Anxiety Disorder, Hyperthyroidism, Cardiovascular Disorders -
Mention likely specific cause of such condition?
Serotonin dysregulation -
Psychopathology mentioned case above?
Acute physiological arousal and catastrophic thinking -
What is two best investigation
- Biological: Thyroid function tests
- Psychological: Detailed panic attack history
-
What is two best Management/Treatment
- Biological: Start an SSRI (e.g., Sertraline 50 mg daily) for 12 weeks
- Psychological: Cognitive Behavioral Therapy focusing on exposure and coping strategies
Panic Attack vs. Panic Disorder
Things to keep in mind
- A panic attack ≠ panic disorder
- Panic disorder often has a waxing and waning course
Case 2: Agoraphobia
Case Scenario:
Emily, a 45-year-old woman, avoids leaving her home due to fear of having a panic attack in public places. She feels trapped and experiences significant distress when considering venturing outside alone.
-
What is the most probable diagnosis?
Agoraphobia - is fear of public places -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Marked fear of using public transportation, being in open spaces, or being in enclosed places
- Avoidance of situations that may cause panic, leading to significant distress and impairment
-
Differential Diagnosis related to the probable diagnosis
Panic Disorder, Social Anxiety Disorder, Major Depressive Disorder -
Mention likely specific cause of such condition?
Learned safety behaviors and avoidance reinforcement -
Psychopathology mentioned case above?
Fear of helplessness in public situations and avoidance behavior -
What is two best investigation
- Biological: Rule out medical conditions like cardiovascular issues
- Psychological: Assess for co-occurring anxiety or depressive disorders
-
What is two best Management/Treatment
- Biological: SSRIs (e.g., Escitalopram 10 mg daily) for at least 12 weeks
- Psychological: Exposure therapy combined with Cognitive Behavioral Therapy
Case 3: Specific Phobia
Case Scenario:
Alex, a 22-year-old college student, has an intense fear of spiders. The sight of a spider causes immediate anxiety, leading him to avoid places where spiders might be present, such as gardens and basements.
-
What is the most probable diagnosis?
Specific Phobia - fear of spiders - (Arachnophobia) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Marked fear or anxiety about a specific object or situation (spiders)
- Immediate fear response upon exposure and active avoidance of the feared object
-
Differential Diagnosis related to the probable diagnosis
Social Anxiety Disorder, Obsessive-Compulsive Disorder, Generalized Anxiety Disorder -
Mention likely specific cause of such condition?
Traumatic experience with spiders or genetic predisposition -
Psychopathology mentioned case above?
Immediate fear response and avoidance behavior -
What is two best investigation
- Biological: Rule out any physiological conditions that may mimic anxiety
- Psychological: Detailed history of fear onset and triggers
-
What is two best Management/Treatment
- Biological: SSRIs are not typically first-line; consider short-term benzodiazepines if necessary
- Psychological: Exposure Therapy and Cognitive Behavioral Therapy
Case 4: Generalized Anxiety Disorder (GAD)
Case Scenario:
Maria, a 30-year-old teacher, constantly worries about various aspects of her life, including work, health, and family. She finds it difficult to control her worry, which has persisted for over a year and affects her daily functioning.
-
What is the most probable diagnosis?
Generalized Anxiety Disorder (GAD) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Worry occurring more days than not for at least six months
- Persistent worries; Difficulty controlling the worry and associated with symptoms like restlessness and fatigue
-
Differential Diagnosis related to the probable diagnosis
Panic Disorder, Major Depressive Disorder, Obsessive-Compulsive Disorder -
Mention likely specific cause of such condition?
Chronic stress and imbalance in neurotransmitters like GABA and serotonin -
Psychopathology mentioned case above?
Persistent worry and physical symptoms of anxiety -
What is two best investigation
- Biological: Thyroid function tests to R/O hyperthyroidism
- Psychological: Comprehensive anxiety assessment
-
What is two best Management/Treatment
- Biological: SSRIs (e.g., Escitalopram 10 mg daily) for 12 weeks
- Psychological: Cognitive Behavioral Therapy focusing on anxiety management techniques
Case 5: Social Anxiety Disorder (SAD)
Case Scenario:
Lisa, a 19-year-old university student, has an intense fear of social situations where she might be judged or embarrassed. She avoids public speaking, social gatherings, and often feels anxious during interactions, significantly impacting her academic and personal life.
-
What is the most probable diagnosis?
Social Anxiety Disorder (SAD) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Marked fear of social or performance situations involving possible scrutiny
- Fear leads to avoidance or enduring with intense anxiety, causing significant impairment
-
Differential Diagnosis related to the probable diagnosis
Generalized Anxiety Disorder, Specific Phobia, Obsessive-Compulsive Disorder -
Mention likely specific cause of such condition?
Negative social experiences and heightened sensitivity to evaluation -
Psychopathology mentioned case above?
Fear of negative evaluation and avoidance of social interactions -
What is two best investigation
- Biological: Rule out medical conditions that may mimic anxiety
- Psychological: Social anxiety assessment and history
-
What is two best Management/Treatment
- Biological: SSRIs (e.g., Paroxetine 20 mg daily) for 12 weeks
- Psychological: Cognitive Behavioral Therapy with social skills training
Case 6: Obsessive-Compulsive Disorder (OCD)
Case Scenario:
Tom, a 26-year-old software engineer, is plagued by intrusive thoughts about contamination. To alleviate his anxiety, he engages in excessive hand-washing multiple times a day, which interferes with his daily activities and social interactions.
-
What is the most probable diagnosis?
Obsessive-Compulsive Disorder (OCD) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Presence of obsessions (intrusive thoughts about contamination)
- Engagement in compulsions (excessive hand-washing, symmetry, checking) to reduce anxiety
-
Differential Diagnosis related to the probable diagnosis
Generalized Anxiety Disorder, Body Dysmorphic Disorder, Tic Disorders -
Mention likely specific cause of such condition?
Serotonin dysregulation and genetic predisposition -
Psychopathology mentioned case above?
Intrusive thoughts and repetitive behaviors to manage anxiety -
What is two best investigation
- Biological: Neuroimaging - MRI
- Psychological: Detailed assessment of obsessive and compulsive symptoms
-
What is two best Management/Treatment
- Biological: SSRIs (e.g., Fluoxetine 60 mg daily) for at least 12 weeks - or escitalopram 10mg/d
- Psychological: Behavioral therapy, Exposure and Response Prevention (ERP) Therapy
Biological Etiology of OCD
Biological Serotonin Hypothesis Clomipramine, SSRI’s, mCPP Neuroimmunology PANDAS, autoimmune Genetics 1st degree relatives 35%, Monozygotes 80-87% Neuroimaging Orbital Frontal Cortex, Basal Ganglia, Anterior Cingulate Gyrus
Psychotic Disorders
Case 1: Major Depressive Disorder (MDD) with Psychotic Features
Case Scenario:
35-year-old male presents with a two-week history of persistent sadness, loss of interest in activities, significant weight loss, insomnia, and feelings of worthlessness. He reports hearing voices that tell him he is useless and should end his life. There is no history of manic episodes or substance use.
-
What is the most probable diagnosis?
Major Depressive Disorder (MDD) with Psychotic Features -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a major depressive episode.
- Presence of psychotic symptoms (auditory hallucinations) during the depressive episode.
-
Differential Diagnosis related to the probable diagnosis
Schizophrenia, Substance-Induced Psychotic Disorder, Delusional Disorder -
Mention likely specific cause of such condition?
Neurochemical imbalances, particularly involving serotonin and dopamine. -
Psychopathology mentioned case above?
Auditory hallucinations and depressive cognitions. -
What is two best investigation
- Blood tests to rule out medical causes.
- Psychiatric evaluation for severity of depression and psychosis.
-
What is two best Management/Treatment
- Antidepressant with antipsychotic (e.g., Sertraline 50mg daily + Risperidone 2mg daily) for 6-8 weeks.
- Cognitive Behavioral Therapy and social support interventions.
Case 2: Bipolar I Disorder, Manic with Psychotic Features
Case Scenario:
28-year-old female exhibits a one-week period of elevated mood, increased energy, reduced need for sleep, grandiose ideas, rapid speech, and impulsive spending. She also experiences delusions of having special powers and hears voices praising her abilities. No prior depressive episodes reported.
-
What is the most probable diagnosis?
Bipolar I Disorder, Manic or Mixed with Psychotic Features -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a manic episode.
- Presence of psychotic features during the manic phase.
-
Differential Diagnosis related to the probable diagnosis
Schizophrenia, Substance-Induced Psychotic Disorder, Delusional Disorder -
Mention likely specific cause of such condition?
Genetic predisposition and dysregulation of dopamine pathways. -
Psychopathology mentioned case above?
Grandiose delusions and auditory hallucinations. -
What is two best investigation
- Comprehensive psychiatric assessment.
- Substance use screening to rule out induced psychosis.
-
What is two best Management/Treatment
- Mood stabilizer such as Lithium 600mg daily + Antipsychotic like Olanzapine 10mg daily for acute management.
- Psychoeducation and family therapy.
Case 3: Schizophrenia
Case Scenario:
22-year-old male presents with a six-month history of social withdrawal, disorganized speech, and reduced emotional expression. He reports hearing multiple voices conversing about him and experiencing delusions of persecution. There is a decline in academic performance and occupational functioning.
-
What is the most probable diagnosis?
-
Schizophrenia with disorganized features
-
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of delusions and hallucinations for more than six months.
- Significant social and occupational dysfunction.
-
Differential Diagnosis related to the probable diagnosis
Schizophreniform Disorder, Bipolar I Disorder with Psychotic Features, Psychotic Disorder NOS -
Mention likely specific cause of such condition?
Genetic factors and neurodevelopmental abnormalities affecting dopamine pathways. -
Psychopathology mentioned case above?
Auditory hallucinations and persecutory delusions. -
What is two best investigation
- MRI or CT scan to rule out brain abnormalities. (usually doesnt need brain imaging, although any visual hallucination may discern need for this in such cases with any SOL cases that may participate associated symptoms)
- Comprehensive psychiatric evaluation.
-
What is two best Management/Treatment
- Atypical antipsychotic such as Risperidone 4mg daily for symptom control. or typical antipsychotic: Haloperidol 1-3 mg/d; side effects extrapyrimidal, tardine dyskinesia -
- Cognitive Behavioral Therapy and supported employment programs.
Case 4: Substance-Induced Psychotic Disorder
Case Scenario:
40-year-old male with a history of chronic cocaine use presents with acute paranoia, visual hallucinations, and delusions of being watched. These symptoms began two days after a binge and have persisted despite abstinence efforts.
-
What is the most probable diagnosis?
Substance-Induced Psychotic Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Onset of psychotic symptoms during or shortly after substance intoxication.
- Evidence of substance use (cocaine) related to the psychosis.
-
Differential Diagnosis related to the probable diagnosis
Schizophrenia, Delusional Disorder, Psychotic Disorder due to a GMC -
Mention likely specific cause of such condition?
Neurotoxicity from cocaine affecting dopamine pathways. -
Psychopathology mentioned case above?
Paranoia, visual hallucinations, and delusional persecution. -
What is two best investigation
- Urine toxicology screen.
- Medical evaluation to rule out other causes.
-
What is two best Management/Treatment
- Antipsychotic such as Haloperidol 5mg as needed.
- Substance abuse counseling and rehabilitation programs.
Case 5: Psychotic Disorder due to a General Medical Condition (GMC)
Case Scenario:
50-year-old female with a recent diagnosis of thyroid carcinoma presents with confusion, visual hallucinations, and delusions of impending doom. Laboratory tests reveal severe hypercalcemia.
-
What is the most probable diagnosis?
Psychotic Disorders Due to a General Medical Condition (GMC) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of psychotic symptoms concurrent with a medical condition (hypercalcemia).
- Temporal relationship between the medical condition and onset of psychosis.
-
Differential Diagnosis related to the probable diagnosis
Delirium, Substance-Induced Psychotic Disorder, Schizophrenia -
Mention likely specific cause of such condition?
Metabolic disturbances (hypercalcemia) affecting brain function. -
Psychopathology mentioned case above?
Visual hallucinations and paranoid delusions. -
What is two best investigation
- Comprehensive metabolic panel.
- Neurological assessment.
-
What is two best Management/Treatment
- Treat underlying hypercalcemia with intravenous fluids and bisphosphonates.
- Supportive psychotherapy and monitoring.
Case 6: Delusional Disorder
Delusional Disorder Subtypes
- Erotomanic
- Grandiose
- Persecutory
- Jealous
- Somatic
- Mixed
Case Scenario:
45-year-old male believes that his neighbor is secretly poisoning his food to harm his health. He has no other psychotic symptoms and maintains normal functioning in his job and social relationships. The belief has persisted for three months.
-
What is the most probable diagnosis?
Delusional Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a nonbizarre delusion for at least one month.
- Absence of other psychotic symptoms and relatively preserved functioning.
-
Differential Diagnosis related to the probable diagnosis
Paranoid Personality Disorder, Schizophrenia, Psychotic Disorder NOS -
Mention likely specific cause of such condition?
Genetic predisposition and cognitive biases towards suspicion. -
Psychopathology mentioned case above?
Persecutory delusions. -
What is two best investigation
- Psychiatric evaluation to assess delusion severity.
- Medical assessment to rule out other causes of paranoid ideation.
-
What is two best Management/Treatment
- Antipsychotic medication such as Risperidone 2mg daily if needed.
- Cognitive Behavioral Therapy focused on reality testing and coping strategies.
Depressive disorder & Suicide
Case 1: MDD
Case Scenario:
A 28-year-old male presents with a two-month history of feeling down, significant weight gain, increased appetite, fatigue, and difficulty concentrating at work. He reports a loss of interest in his hobbies and has had occasional thoughts of self-harm but no specific plan.
-
What is the most probable diagnosis?
Major Depressive Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Persistent low mood for at least two weeks
- Significant weight gain and increased appetite
-
Differential Diagnosis related to the probable diagnosis
Bipolar Disorder, Hypothyroidism, Adjustment Disorder -
Mention likely specific cause of such condition?
Biochemical deficit of Serotonin and Noradrenaline -
Psychopathology mentioned case above?
Anhedonia, impaired concentration -
What is two best investigation
Thyroid function tests
Clinical interview for psychosocial stressors -
What is two best Management/Treatment
Biological:- Start Sertraline 50 mg daily
- Duration: 6-9 months
- Time to work: 4-6 weeks
Psychological & Social:
- Cognitive Behavioral Therapy
- Social support interventions
Case 2: MDD
Case Scenario:
A 45-year-old divorced woman has been experiencing persistent sadness, insomnia, and feelings of worthlessness for the past three weeks. She has withdrawn from social activities and has missed several days of work. She denies any suicidal ideation.
-
What is the most probable diagnosis?
Major Depressive Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Depressed mood for more than two weeks
- Insomnia and feelings of worthlessness
-
Differential Diagnosis related to the probable diagnosis
Dysthymia (Two years of depressed mood for more days than not) , Bipolar Disorder, Grief -
Mention likely specific cause of such condition?
Psychosocial stressors related to divorce -
Psychopathology mentioned case above?
Social withdrawal, impaired occupational functioning -
What is two best investigation
Complete blood count and chemistries
Assessment of social support systems -
What is two best Management/Treatment
Biological:- Begin Fluoxetine 20 mg daily
- Duration: 6 months
- Time to work: 4-6 weeks
Psychological & Social:
- Interpersonal Therapy
- Family therapy to enhance social support
Case 3: MDD
Case Scenario:
A 60-year-old male with a history of hypertension and coronary artery disease presents with a two-month history of decreased interest in activities, fatigue, and difficulty concentrating. He has noticed a decline in his work performance and has minimal engagement with family members. He denies any thoughts of self-harm.
-
What is the most probable diagnosis?
Major Depressive Disorder associated with coronary disease -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Persistent low mood for over two weeks
- Decreased interest in activities and fatigue
-
Differential Diagnosis related to the probable diagnosis
Chronic Medical Illness-related Depression, Dementia, Adjustment Disorder -
Mention likely specific cause of such condition?
Chronic medical illness contributing to depressive symptoms -
Psychopathology mentioned case above?
Anhedonia, impaired occupational and social functioning -
What is two best investigation
Thyroid function tests
Evaluation of psychosocial stressors related to chronic illness -
What is two best Management/Treatment
Biological:- Initiate Escitalopram 10 mg daily
- Duration: 6-12 months
- Time to work: 4-6 weeks fully work - initial effects at 2 weeks
Psychological & Social:
- Behavioral Activation Therapy
- Support groups for individuals with chronic illnesses
What are the areas in Brain Affected by Depression ?? • Limbic System • Hypothalamus - Hippocampus
Depression & Medical illness
Case 1: Depression & Coronary Heart Disease
Case Scenario:
John, a 58-year-old male with a history of coronary heart disease (CHD), presents with persistent low mood, loss of interest in activities he once enjoyed, and increased fatigue over the past two months. He reports difficulty sleeping and a decrease in appetite. John has been less compliant with his medication regimen since his CHD diagnosis.
-
What is the most probable diagnosis?
Major Depressive Disorder associated with CHD -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Depressed mood
- Loss of interest or pleasure
-
Differential Diagnosis related to the probable diagnosis
Adjustment Disorder with Depressed Mood, Bipolar II Disorder -
Mention likely specific cause of such condition?
Chronic stress and physiological changes related to coronary heart disease -
Psychopathology mentioned case above?
Depressed mood, anhedonia, sleep and appetite disturbances -
What is two best investigation (biological, psychological, social investigations)
- PHQ-9 depression screening
- Medication adherence assessment
-
What is two best Management/Treatment (biological; dose, duration, time to work) (psychological & social investigations)
- Biological: Sertraline 50 mg daily for 6-12 weeks
- Psychological: Cognitive Behavioral Therapy (CBT)
Case 2: Depression & Diabetes
Case Scenario:
Maria, a 45-year-old female with type II diabetes mellitus, has been experiencing persistent sadness, decreased energy, and difficulty concentrating for the past three months. She has noticed increased blood glucose levels and has struggled to maintain her dietary regimen.
-
What is the most probable diagnosis?
Major Depressive Disorder associated with DM II -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Depressed mood
- Poor concentration/indecisiveness
-
Differential Diagnosis related to the probable diagnosis
Persistent Depressive Disorder, Adjustment Disorder with Depressed Mood, Bipolar Disorder -
Mention likely specific cause of such condition?
Bi-directional relationship between diabetes and depression, poor glycemic control -
Psychopathology mentioned case above?
Depressed mood, decreased energy, impaired concentration -
What is two best investigation (biological, psychological, social investigations)
- HbA1c levels
- Depression screening questionnaire (e.g., PHQ-9)
-
What is two best Management/Treatment (biological; dose, duration, time to work) (psychological & social investigations)
- Biological: Escitalopram 10 mg daily for 6-8 weeks
- Social: Diabetes education and support groups
Case 3: Depression & Cancer
Case Scenario:
Emma, a 52-year-old female recently diagnosed with breast cancer, reports feelings of hopelessness, crying spells, and a lack of interest in daily activities. She is undergoing chemotherapy and expresses concerns about her prognosis and the impact of treatment on her family.
-
What is the most probable diagnosis?
Major Depressive Disorder associated with Breast cancer -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Depressed mood
- Feelings of hopelessness
-
Differential Diagnosis related to the probable diagnosis
Adjustment Disorder with Depressed Mood, Anxiety Disorder, Persistent Depressive Disorder -
Mention likely specific cause of such condition?
Psychological stress related to cancer diagnosis and treatment -
Psychopathology mentioned case above?
Hopelessness, anhedonia, emotional distress -
What is two best investigation (biological, psychological, social investigations)
- Clinical interview for depression
- Assessment of social support networks
-
What is two best Management/Treatment (biological; dose, duration, time to work) (psychological & social investigations)
- Biological: Citalopram 20 mg daily for 8-12 weeks
- Psychological: Supportive psychotherapy
Case 4: Depression and Medical Illnesses
Case Scenario:
Robert, a 70-year-old male with chronic kidney disease (CKD), presents with persistent sadness, fatigue, and decreased appetite. He has difficulty adhering to his dialysis schedule and reports feeling worthless. His medical team is concerned about his declining self-care.
-
What is the most probable diagnosis?
Major Depressive Disorder associated with CKD -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Depressed mood
- Decreased appetite
-
Differential Diagnosis related to the probable diagnosis
Depressive Disorder due to Another Medical Condition, Adjustment Disorder, Persistent Depressive Disorder -
Mention likely specific cause of such condition?
Interrelation between chronic medical condition (CKD) and depression -
Psychopathology mentioned case above?
Depressed mood, fatigue, hopelessness -
What is two best investigation (biological, psychological, social investigations)
- Screening for depression (e.g., Geriatric Depression Scale)
- Evaluation of renal function and treatment adherence
-
What is two best Management/Treatment (biological; dose, duration, time to work) (psychological & social investigations)
- Biological: Sertraline 50 mg daily, monitor for serotonin syndrome
- Social: Dialysis adherence support and counseling
Bipolar Disorders
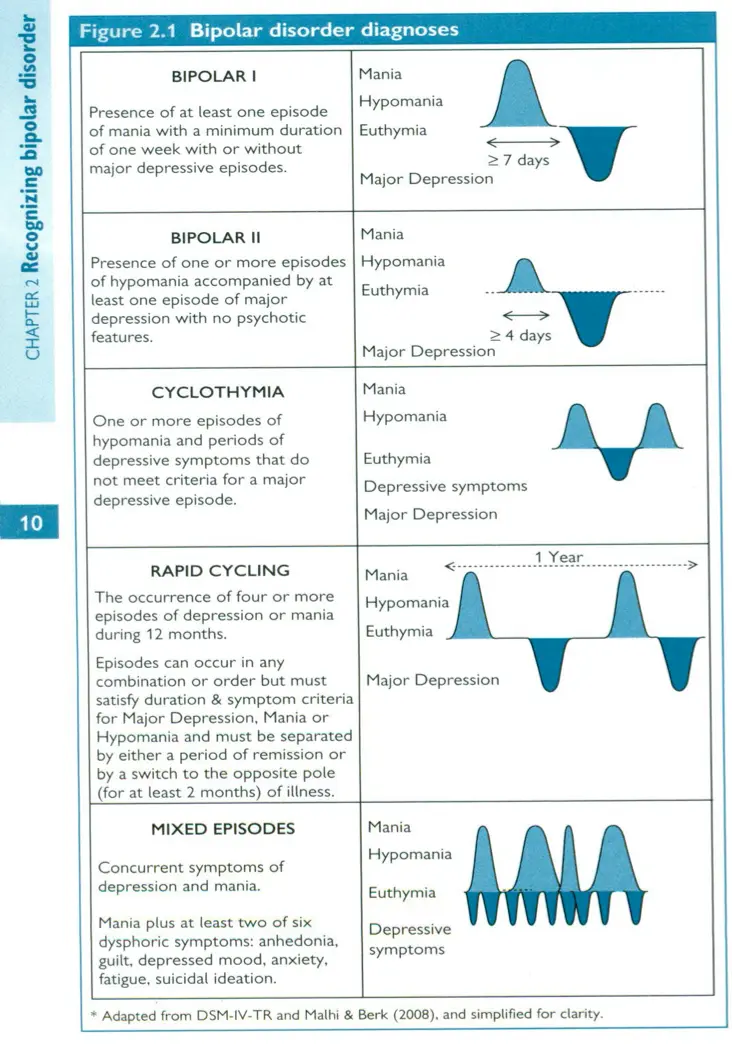
Bipolar disorder diagnoses
- BIPOLAR I
- Presence of at least one episode of mania with a minimum duration of one week with or without major depressive episodes.
- BIPOLAR II
- Presence of one or more episodes of hypomania accompanied by at least one episode of major depression with no psychotic features.
- CYCLOTHYMIA
- One or more episodes of hypomania and periods of depressive symptoms that do not meet criteria for a major depressive episode.
- RAPID CYCLING
- The occurrence of four or more episodes of depression or mania during 12 months.
- Episodes can occur in any combination or order but must satisfy duration & symptom criteria for Major Depression, Mania or Hypomania and must be separated by either a period of remission or by a switch to the opposite pole (for at least 2 months) of illness.
- MIXED EPISODES
- Concurrent symptoms of depression and mania.
- Must also be at least two of six of the following:
- Mania
- Hypomania
- Euthymia
- Depressive symptoms
- Major Depression
Case 1: Bipolar Depression
Case Scenario:
A 28-year-old female presents with persistent feelings of sadness, loss of interest in activities, and significant weight loss over the past two months. She reports difficulty concentrating and feelings of hopelessness. She had previous history of elevated mood episodes treated intermittently with lithium.
-
What is the most probable diagnosis?
Bipolar II -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of at least one major depressive episode.
- History of previous manic or hypomanic episodes.
-
Differential Diagnosis related to the probable diagnosis:
Major Depressive Disorder, Cyclothymia -
Mention likely specific cause of such condition?
Heritability and genetic predisposition. -
Psychopathology mentioned case above?
Depression -
What are two best investigations?
- Comprehensive psychiatric evaluation.
- Family history assessment.
-
What are two best Management/Treatment?
- Biological: Start Lithium 300 mg BID, monitor levels; duration: indefinite prophylaxis.
- Psychological: Cognitive Behavioral Therapy (CBT).
Case 2: Acute Treatment of Mania, Mixed State, Rapid Cycling
Case Scenario:
A 35-year-old male is brought to the emergency department exhibiting excessive energy, reduced need for sleep, grandiose ideas, and rapid speech lasting for five days. His behavior is erratic, and he has been impulsively spending large sums of money. There is a history of similar episodes occurring four times in the past year.
-
What is the most probable diagnosis?
Bipolar I Disorder, Acute Mania with Rapid Cycling -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a manic episode lasting at least one week.
- History of four or more mood episodes within the past year.
- Flight of ideas, grandiose
-
Differential Diagnosis related to the probable diagnosis:
Substance-induced mood disorder, Schizophrenia -
Mention likely specific cause of such condition?
Neurochemical imbalances, genetic factors. -
Psychopathology mentioned case above?
Mania -
What are two best investigations?
- Laboratory tests including CBC, electrolytes, liver function tests.
- Psychiatric evaluation for substance use; toxology
-
What are two best Management/Treatment?
- Biological: Start Divalproex 500 mg BID; duration: acute management.
- Biological: Initiate Risperidone 2 mg/day; time to work: within days.
- Psychological & Social: Psychoeducation and family therapy.
Case 3: Bipolar & Pregnancy
Case Scenario:
A 30-year-old pregnant woman at 8 weeks gestation with Bipolar I Disorder is experiencing a depressive episode. She is currently on Valproic Acid but is concerned about the effects on her pregnancy.
-
What is the most probable diagnosis?
Bipolar I Disorder, Depressive Episode during Pregnancy -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Presence of a major depressive episode.
- History of at least one manic episode.
-
Differential Diagnosis related to the probable diagnosis:
Major Depressive Disorder with psychotic features, Adjustment Disorder with depressed mood -
Mention likely specific cause of such condition?
Medication-related teratogenic effects and hormonal changes during pregnancy. -
Psychopathology mentioned case above?
Depression -
What are two best investigations?
- Fetal ultrasound for neural tube defects.
- Comprehensive risk-benefit analysis of medication use during pregnancy.
-
What are two best Management/Treatment?
- Biological: Switch from Valproic Acid to Lamotrigine; dose: start at 25 mg daily, titrate gradually.
- Biological: Continue Lithium with dose adjustments as needed; monitor levels closely.
- Psychological & Social: Initiate psychotherapy (e.g., Interpersonal Therapy) and provide social support.
Cognitive disorders
Case 1: Delirium
Case Scenario:
A 78-year-old man is admitted to the hospital for pneumonia. On the second day of hospitalization, he becomes increasingly confused, has difficulty paying attention, and exhibits fluctuating levels of consciousness. His family reports that he was alert and oriented at admission but now is disoriented to time and place, with episodes of agitation and periods of lethargy.
-
What is the most probable diagnosis?
Delirium -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Disturbance in attention and awareness
- Acute onset with a fluctuating course
-
Differential Diagnosis related to the probable diagnosis
Major Neurocognitive Disorder, Depression, Schizophrenia -
Mention likely specific cause of such condition?
Infection (pneumonia) leading to physiological disturbances -
Psychopathology mentioned case above?
Agitation and periods of lethargy -
What is two best investigation
- Electrolyte panel
- Cognitive assessment (e.g., MMSE)
-
What is two best Management/Treatment
- Treat underlying pneumonia
- Antipsychotic medication (e.g., Haloperidol 0.5 mg IV as needed)
Case 2: Dementia
Case Scenario:
A 68-year-old woman presents with progressive memory loss over the past two years. She struggles to remember recent events, has difficulty planning and organizing daily tasks, and occasionally experiences confusion about familiar places. Her family has noticed a gradual decline in her ability to manage finances and perform household chores.
-
What is the most probable diagnosis?
Major Neurocognitive Disorder (Dementia) -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Significant cognitive decline in memory and executive function
- Impairment in independence with daily activities
-
Differential Diagnosis related to the probable diagnosis
Depression (Pseudodementia), Mild Neurocognitive Disorder, Alzheimer’s Disease -
Mention likely specific cause of such condition?
Alzheimer’s Disease -
Psychopathology mentioned case above?
Memory loss, executive dysfunction, confusion -
What is two best investigation
- Neuropsychological testing
- MRI of the brain
-
What is two best Management/Treatment
- Cholinesterase inhibitor (e.g., Donepezil 5 mg daily, titrate as needed)
- Supportive therapy and caregiver education
Case 3: Alcohol Withdrawal (Delirium Tremens)
Case Scenario:
A 55-year-old man with a history of chronic alcohol use presents to the emergency department 4 days after his last drink. He is agitated, disoriented, has tremors, excessive sweating, tachycardia, and visual hallucinations. His family reports that he has been unable to sleep and is experiencing severe anxiety and confusion.
-
What is the most probable diagnosis?
Delirium Tremens (Severe Alcohol Withdrawal) -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Acute onset with confusion and disorientation
- Autonomic hyperactivity (tachycardia, sweating) and tremors
-
Differential Diagnosis related to the probable diagnosis
Sepsis-induced delirium, Benzodiazepine withdrawal, Acute psychosis -
Mention likely specific cause of such condition?
Chronic alcohol use leading to severe withdrawal -
Psychopathology mentioned case above?
Agitation, anxiety, confusion, visual hallucinations -
What is two best investigation
- Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar)
- Electrolyte panel
- Toxology
-
What is two best Management/Treatment
- Benzodiazepines; diazepam 20-50mg/d or (e.g., Lorazepam 2 mg IV every 1 hour as needed) ,
- Thiamine supplementation (e.g., Thiamine 100 mg/daily)
-
Mention non-pharmacological management strategy
- CBT
- Contingency management
- Motivational interviewing
Case 4: Alcohol-Related Disorder (Wernicke’s Encephalopathy)
Case Scenario:
A 60-year-old chronic alcoholic is brought to the hospital with confusion, unsteady gait, and abnormal eye movements. He has a history of poor dietary intake and prolonged vomiting. On examination, he is disoriented, has nystagmus, and exhibits ataxia of stance and gait.
-
What is the most probable diagnosis?
Wernicke’s Encephalopathy -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Encephalopathy (confusion, disorientation)
- Oculomotor dysfunction (nystagmus) and gait ataxia
-
Differential Diagnosis related to the probable diagnosis
Delirium Tremens, Basal Nerve Thiamine Deficiency, Multiple Sclerosis -
Mention likely specific cause of such condition?
Thiamine (Vitamin B1) deficiency due to chronic alcohol use -
Psychopathology mentioned case above?
Confusion and disorientation -
What is two best investigation
- Thiamine level
- MRI of the brain
-
What is two best Management/Treatment
- Thiamine supplementation (e.g., Thiamine 500 mg IV daily)
- Nutritional support and hydration
Case 5: Alcohol-Related Disorder (Korsakoff’s Syndrome)
Case Scenario:
A 65-year-old man with a long history of alcohol abuse is brought to the clinic by his family. They report that he has severe memory loss, especially for recent events, and often makes up stories to fill in gaps in his memory. Despite his memory issues, he maintains his long-term memories and social skills. He is unaware of his memory deficits.
-
What is the most probable diagnosis?
Korsakoff’s Syndrome -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Severe anterograde and retrograde amnesia
- Confabulation and lack of awareness of memory deficits
-
Differential Diagnosis related to the probable diagnosis
Alzheimer’s Disease, Delirium, Depression -
Mention likely specific cause of such condition?
Chronic thiamine deficiency due to prolonged alcohol abuse -
Psychopathology mentioned case above?
Memory loss, confabulation -
What is two best investigation
- Neuropsychological testing
- Thiamine level assessment
-
What is two best Management/Treatment
- Thiamine supplementation (e.g., Thiamine 500 mg IV daily)
- Cognitive rehabilitation and supportive psychotherapy
Case 6: Alcohol Use Disorder
Case Scenario:
A forty-year-old woman presents for evaluation with a history of increasing alcohol consumption over the past five years. She reports drinking daily, often unable to reduce her intake despite wanting to. She has experienced unsuccessful attempts to cut down, and her drinking has led to problems at work and strained family relationships.
-
What is the most probable diagnosis?
Alcohol Use Disorder - alcoholism -
How would you support your diagnosis for this scenario (2 diagnostic criteria)?
- Persistent desire or unsuccessful efforts to cut down alcohol use
- Continued use despite social and occupational problems
-
Differential Diagnosis related to the probable diagnosis
Depression, Anxiety Disorders, Personality Disorders -
Mention likely specific cause of such condition?
Genetic predisposition and environmental factors contributing to dependency -
Psychopathology mentioned case above?
Dependence on alcohol, impaired control over drinking -
What is two best investigation
- Alcohol use history and screening (e.g., AUDIT)
- Liver function tests
-
What is two best Management/Treatment
- Pharmacotherapy (e.g., Naltrexone 50 mg daily)
- Cognitive-behavioral therapy and support groups
Substance abuse
Case 1: Hallucinogens
Case Scenario:
A 22-year-old university student is brought to the emergency department by friends after exhibiting erratic and unpredictable behavior following a party. He is experiencing visual hallucinations, believes he can communicate with extraterrestrial beings, and has difficulty distinguishing reality from his perceptions.
-
What is the most probable diagnosis?
Hallucinogen Intoxication -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Distorted perception with visual hallucinations
- Unpredictable and dangerous behavior
-
Differential Diagnosis related to the probable diagnosis
Acute psychotic disorder, Substance-induced psychosis, Schizophrenia -
Mention likely specific cause of such condition?
Use of LSD or similar hallucinogenic substances -
Psychopathology mentioned case above?
Delusions of communication with extraterrestrial beings -
What is two best investigation
- Toxicology screening (biological)
- Psychological assessment for underlying mental health conditions
-
What is two best Management/Treatment
- Supportive care and benzodiazepines for agitation (biological)
- Cognitive Behavioral Therapy (psychological)
Case 2: Cannabinoids
Case Scenario:
A 19-year-old female presents with red, bloodshot eyes, dry mouth, increased appetite, and a rapid heart rate after attending a social gathering where marijuana was consumed. She appears relaxed but slightly anxious.
-
What is the most probable diagnosis?
Cannabis Intoxication -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Recent use of cannabis
- Two or more signs: conjunctival injection and tachycardia
-
Differential Diagnosis related to the probable diagnosis
Acute anxiety episode, Allergic conjunctivitis, Other substance intoxications -
Mention likely specific cause of such condition?
Consumption of marijuana containing high levels of THC -
Psychopathology mentioned case above?
Anxiety related to intoxication -
What is two best investigation
- Urine drug screen for cannabinoids (biological)
- Social history to assess frequency and context of use
-
What is two best Management/Treatment
- Supportive care and hydration (biological)
- Motivational Interviewing to address use behaviors (psychological)
Case 3: Stimulants
Case Scenario:
A 28-year-old male presents with elevated blood pressure, tachycardia, dilated pupils, and reports feeling extremely energetic and unable to sleep after taking methamphetamine to enhance his work performance. He exhibits hypervigilance and paranoia about his colleagues.
-
What is the most probable diagnosis?
Stimulant Intoxication (Methamphetamine) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Recent use of methamphetamine
- Symptoms of increased heart rate and paranoia
-
Differential Diagnosis related to the probable diagnosis
Acute psychotic disorder, Cocaine intoxication, Hyperthyroidism -
Mention likely specific cause of such condition?
Abuse of methamphetamine leading to excessive CNS stimulation -
Psychopathology mentioned case above?
Paranoid delusions and hypervigilance -
What is two best investigation
- Urine toxicology for stimulants (biological)
- Psychological evaluation for potential psychosis
-
What is two best Management/Treatment
- Benzodiazepines to manage agitation and prevent seizures (biological)
- Cognitive Behavioral Therapy for stimulant abuse (psychological)
Case 4: Opioids
Case Scenario:
A 35-year-old male with a history of heroin use is brought to the clinic for evaluation. He reports needing to use heroin daily to function normally and experiences severe withdrawal symptoms, including muscle aches, nausea, and anxiety when attempting to reduce use.
-
What is the most probable diagnosis?
Opioid Use disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Strong desire or compulsion to take heroin
- Withdrawal symptoms upon cessation
-
Differential Diagnosis related to the probable diagnosis
Alcohol dependence, Benzodiazepine dependence, Chronic pain syndrome -
Mention likely specific cause of such condition?
Prolonged use of heroin leading to physical and psychological dependence -
Psychopathology mentioned case above?
Compulsive drug-seeking behavior despite harmful consequences -
What is two best investigation
- Urine toxicology for opioids (biological)
- Hepatitis viruses screening, HIV screening
- Assessment of social factors contributing to dependence
-
What is two best Management/Treatment
- treatment of the withdrawal state – buprenorphine,
- Behavioral Therapy (psychological)
- Group therapy
Case 5: Sedatives & Hypnotics
Case Scenario:
A 45-year-old female with a history of insomnia has been taking high doses of benzodiazepines for the past year. She reports experiencing anxiety, tremors, and seizures upon attempting to reduce her medication without medical supervision.
-
What is the most probable diagnosis?
Sedative, Hypnotic or Anxiolytic Dependence -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Evidence of tolerance and withdrawal symptoms
- Difficulty controlling benzodiazepine use
-
Differential Diagnosis related to the probable diagnosis
Generalized Anxiety Disorder, Panic Disorder, Epilepsy -
Mention likely specific cause of such condition?
Chronic use and dependence on benzodiazepines for insomnia -
Psychopathology mentioned case above?
Physical dependence with withdrawal-induced seizures -
What is two best investigation
- Clinical assessment for withdrawal symptoms (biological)
- Psychological evaluation for anxiety and dependence patterns
-
What is two best Management/Treatment
- Slow tapering of benzodiazepine dose combined with anticonvulsants as needed (biological)
- Cognitive Behavioral Therapy
Case 6: Volatile Solvents
Case Scenario:
A 16-year-old adolescent is brought to the emergency room exhibiting disorientation, incoordination, and slurred speech after being found inhaling glue to alleviate peer pressure stress. He reports feeling euphoric but is now confused and unable to stand steadily.
-
What is the most probable diagnosis?
Volatile Solvent Intoxication -
How would you support your diagnosis (2 diagnostic criterias)
- Recent inhalant use (glue)
- Acute onset of disorientation and incoordination
-
Differential Diagnosis related to the probable diagnosis
Alcohol intoxication, Cannabis intoxication, Acute psychotic episode -
Mention likely specific cause of such condition?
Inhalation of volatile solvents present in glue leading to CNS depression -
Psychopathology mentioned case above?
Acute confusion and impaired motor coordination -
What is two best investigation
- Blood tests to rule out other intoxications (biological)
- Social assessment for substance use patterns and peer influences
-
What is two best Management/Treatment
- Supportive care with oxygen therapy as needed (biological)
- Behavioral counseling and family therapy to address use (psychological & social)
Stress
Case 1: Acute Stress Disorder
Case Scenario:
John, a 28-year-old firefighter, was involved in a severe house fire where he narrowly escaped while rescuing a family. In the weeks following the incident, he experiences frequent flashbacks, nightmares, and avoids places that remind him of the fire. He also feels constantly on edge and has difficulty concentrating at work.
-
What is the most probable diagnosis?
Acute Stress Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Exposure to a traumatic event (severe house fire).
- Presence of dissociative symptoms (flashbacks, nightmares, reccurent dreams).
- minimum of 2 days and a maximum of 4 weeks and occurs within 4 weeks
-
Differential Diagnosis related to the probable diagnosis
- Adjustment Disorder,
- MDD, anxiety disorders (gen/panic)
- Posttraumatic Stress Disorder (PTSD)?
-
Mention likely specific cause of such condition?
Exposure to life-threatening trauma. -
Psychopathology mentioned case above?
Reexperiencing, avoidance, hyperarousal. -
What is two best investigation
- Clinical interview (Psychological).
- Assessment of sleep patterns and stress levels (Biological).
-
What is two best Management/Treatment
- Biological: SSRI e.g., Sertraline 50 mg daily for 6 months. , paroxetine srris 20 mg/d, or tricylclic imipramine 75mg/d
- Psychological: Cognitive Behavioral Therapy (CBT).
Case 2: Posttraumatic Stress Disorder (PTSD)
Case Scenario:
Maria, a 35-year-old nurse, witnessed a colleague’s sudden death during a night shift at the hospital. Six months later, she continues to have intrusive memories of the event, avoids thinking about work, and has become increasingly irritable and hypervigilant, affecting her personal and professional relationships, she has been seeing reccurent flashbacks of the event.
-
What is the most probable diagnosis?
Posttraumatic Stress Disorder (PTSD) -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Recurrent images, thoughts, or perceptions.
- Recurrent distressing dreams of the event.
- Acting or feeling as if the traumatic event were recurring flashback
- Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event
C. Persistent avoidance of stimuli associated with the trauma.
D. Persistent symptoms of increased arousal (not present before).
E. Duration is more than 1 month.
-
Differential Diagnosis related to the probable diagnosis
Major Depressive Disorder Acute Stress Disorder? adjustment disorder anxiety disorders (generalized/panic) -
Mention likely specific cause of such condition?
Witnessing a colleague’s sudden and traumatic death. -
Psychopathology mentioned case above?
Intrusive thoughts, avoidance behavior, increased arousal. -
What is two best investigation
- Structured Clinical Interview for criteria’s.
- Evaluation of social support systems (Social).
-
What is two best Management/Treatment
- Biological: SSRI e.g., Fluoxetine 20 mg daily for 6 months. / ecitalopram 10mg/d 2wk effect, full 4wk for 6m / Propranolol
- Psychological: Trauma-focused Cognitive Behavioral Therapy (CBT).
- Social: education
Case 3: Adjustment Disorder
Case Scenario:
Sara, a 22-year-old university student, recently moved to a new city for her studies. Within three months, she has been feeling unusually sad, has lost interest in her studies, and has started isolating herself from friends and family. She reports difficulty managing her daily responsibilities and experiences significant distress.
-
What is the most probable diagnosis?
Acute Adjustment Disorder -
How would you support your diagnosis for this scenario (2 diagnostic criterias)
- Emotional symptoms (sadness, loss of interest) in response to an identifiable stressor (moving to a new city).
- Occurring within three months of the onset of the stressor.
-
Specify if:
- Acute: less than 6 months
- Chronic: for 6 months or longer
- The specific stressor(s) can be specified on Axis IV
- With depressed mood, anxiety, mixed or with disturbance of conduct
-
Differential Diagnosis related to the probable diagnosis
Major Depressive Disorder, Acute Stress Disorder -
Mention likely specific cause of such condition?
Significant life change and relocation. -
Psychopathology mentioned case above?
Depressed mood, social withdrawal, impaired functioning. -
What is two best investigation
- Psychological assessment using DSM-5 criteria.
- Evaluation of social support and coping mechanisms (Social).
-
What is two best Management/Treatment
- Biological: Low-dose antidepressants if depressive symptoms are severe, e.g., Escitalopram 10 mg daily for 3 months.
- Psychological: Supportive counseling/psychotherapy and stress management techniques, explaination, education
Stress Related Medical Diseases
Cardiovascular Disease
- Cardiovascular disease is probably the most serious health problem that can be linked to stress.
- The most common cause of death in Britain and the USA.
- The primary causes of heart disease include smoking and high-fat diets, but stress is a significant contributory factor.
- Adrenal hormones act to increase blood pressure; frequent or perpetual state of high blood pressure can have a serious effect on health in the long term.
- High blood pressure is linked with the development of arteriosclerosis, or hardening of the arteries.
- Eventually, an artery can become blocked, leading to angina, stroke, and heart failure.
The Immune System
-
The immune system protects the body from infection. It fights foreign invaders (such as viruses and harmful bacteria) and cancer.
-
Excessive stress can damage the immune system by affecting the thymus gland, which forms T-cells for regulating immunity and also produces various immune-related hormones.
-
The stress reaction diverts resources to the main parts of the body that need to deal with stress, mainly the brain, heart, and muscles.
-
Hormones produced by the adrenal glands can cause the thymus gland to shrink and also degrade the activity of white blood cells, causing damage to the body’s ability to fight infection.
-
As a result, high stress can result in reduced resistance to common infections, such as colds, influenza, and herpes (cold sores).
Diabetes
- The release of adrenal hormones under stress can have a significant impact on blood-sugar levels.
- Adrenaline causes sugar in the liver to be dumped into the bloodstream, and cortisol acts to reduce metabolism of glucose by cells.
- Large amounts of cortisol act to decrease insulin sensitivity. High blood-sugar levels are not dangerous in normally healthy individuals, but chronic stress, combined with other factors such as obesity, act to increase the likelihood of developing diabetes.
Digestive Disorders
-
Many problems with the digestive tract, such as constipation, diarrhea, and irritable bowel syndrome, are linked to stress.
-
Hormonal imbalances can cause alterations in intestinal function, such as spasms, constipation, and diarrhea.
-
Chronic stress tends to disturb the digestive system altogether, exacerbating intestinal problems.
Headaches
- Most headaches are caused not by disease but by fatigue, emotional disorders, or allergies.
- Intermittent tension headaches are caused by worry, anxiety, overwork, or inadequate ventilation.
- The most common type a chronic tension headache is often caused by depression.
- Headaches brought on by muscle spasms are classified as tension headaches; almost 90 percent.
- Tension headaches are often associated with poor sleep.
Premenstural Syndrome (PMS)
-
Stress has a debilitating effect on the nerves in general, and certain premenstrual symptoms may be aggravated by stress.
-
Many sufferers of PMS have abnormal levels of the adrenal hormone aldosterone which may account for some of the problems of excessive fluid retention and weight gain, breast tenderness, and abdominal bloating.
-
Further release of aldosterone caused by stress will exacerbate these problems.
Depression
- Chronic stress can produce severe depression, because of its debilitating psychological effects.
- The physiological changes produced by stress can also contribute to depression.
- Adrenaline and noradrenaline are not only adrenal hormones but also chemical messengers in the brain.
- Deficiencies of noradrenaline have been linked to depression in certain individuals.
- Adrenal exhaustion through chronic long-term stress may be a contributory factor in depressive illness.
Women health
Case 1: Postpartum Depression
Case Scenario:
Jane, a 28-year-old mother, has been experiencing persistent feelings of sadness, fatigue, and anxiety for the past two months following the birth of her first child. She finds it difficult to bond with her baby and has lost interest in activities she once enjoyed. Jane also struggles with feelings of worthlessness and fears she cannot cope with motherhood.
-
What is the most probable diagnosis?
Postpartum Depression -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Major depressive episode occurring within 6 weeks postpartum.
- Persistent feelings of sadness, fatigue, and anxiety affecting daily functioning.
-
Differential Diagnosis related to the probable diagnosis
Postpartum Blues, Adjustment Disorder with Depressed Mood -
Mention likely specific cause of such condition?
Hormonal changes after childbirth -
Psychopathology mentioned case above?
Major Depressive Disorder -
What is two best investigation
- Clinical interview assessing depressive symptoms
- Hormonal level tests
-
What is two best Management/Treatment
- Biological: Start SSRIs (e.g., Sertraline 50mg daily) for 6-12 months
- Psychological: Interpersonal Therapy (IPT) for 12 weeks
Case 2: Anorexia Nervosa
Case Scenario:
Emily, a 17-year-old female, has lost significant weight over the past three months. She restricts her food intake severely, exercises excessively, and exhibits an intense fear of gaining weight. Emily frequently excuses herself from meals and expresses a distorted body image, believing she is overweight despite being underweight.
-
What is the most probable diagnosis?
Anorexia Nervosa -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Restriction of energy intake leading to significantly low body weight.
- Intense fear of gaining weight and distorted body image.
-
Differential Diagnosis related to the probable diagnosis
Major Depressive Disorder, Body Dysmorphic Disorder -
Mention likely specific cause of such condition?
Combination of genetic predisposition and environmental factors related to body image. -
Psychopathology mentioned case above?
Distortion of body image, anxiety about weight gain -
What is two best investigation
- Biological: Complete blood count (CBC) and electrolyte panel
- Psychological: Eating Disorder Inventory (EDI-2)
-
What is two best Management/Treatment
- Biological: Hospitalization for severe weight loss if necessary
- Psychological: Cognitive Behavioral Therapy (CBT) for 6 months
Case 3: Bulimia Nervosa
Case Scenario:
Mark, a 20-year-old male, engages in recurrent episodes of binge eating, consuming large amounts of food in a short period. Following these episodes, he compensates by self-induced vomiting and excessive use of laxatives. Mark expresses a significant concern over his body shape and weight despite maintaining a relatively normal body weight.
-
What is the most probable diagnosis?
Bulimia Nervosa -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Recurrent episodes of binge eating followed by inappropriate compensatory behaviors.
- Self-evaluation is unduly influenced by body shape and weight.
-
Differential Diagnosis related to the probable diagnosis
Anorexia Nervosa (binge-eating/purging subtype), Borderline Personality Disorder -
Mention likely specific cause of such condition?
Psychological factors including low self-esteem and societal pressure on body image. -
Psychopathology mentioned case above?
Binge-purge cycle, body dissatisfaction -
What is two best investigation
- Biological: Electrolyte imbalance assessment
- Psychological: Structured Clinical Interview for DSM Disorders
-
What is two best Management/Treatment
- Biological: Start SSRIs (e.g., Fluoxetine 60mg daily) for 6 months
- Psychological: Cognitive Behavioral Therapy (CBT) for 6-12 months
Case 4: Woman Health Psychiatry
Case Scenario:
Maria, a 35-year-old woman, experiences depressive symptoms during her perimenopausal period. She reports mood swings, anxiety, and a lack of interest in daily activities. Maria also faces challenges related to hormonal changes and increased responsibilities at work and home, contributing to her mental health struggles.
-
What is the most probable diagnosis?
Perimenopause-related Depression -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Depressive symptoms temporally associated with perimenopausal hormonal changes.
- Onset of symptoms during the perimenopausal period.
-
Differential Diagnosis related to the probable diagnosis
Major Depressive Disorder, Adjustment Disorder with Depressed Mood -
Mention likely specific cause of such condition?
Hormonal fluctuations during perimenopause -
Psychopathology mentioned case above?
Mood swings, anxiety, depressive symptoms -
What is two best investigation
- Biological: Hormone level tests (e.g., estrogen, progesterone)
- Psychological: Beck Depression Inventory (BDI)
-
What is two best Management/Treatment
- Biological: Hormone Replacement Therapy (HRT) as appropriate
- Psychological: Cognitive Behavioral Therapy (CBT) for 12 weeks
Case 5: Eating Disorders
Case Scenario:
Sophia, a 22-year-old university student, exhibits an intense fear of gaining weight and engages in extreme dietary restrictions and excessive exercise. She is preoccupied with her body weight and shape, often skipping meals and avoiding social situations involving food. Despite her low body weight, Sophia denies feeling fat and continues her restrictive behaviors.
-
What is the most probable diagnosis?
Anorexia Nervosa -
How would you support your diagnosis for this scenario (2 diagnostic criterias)?
- Restriction of energy intake leading to significantly low body weight.
- Intense fear of gaining weight and distorted body image.
-
Differential Diagnosis related to the probable diagnosis
Bulimia Nervosa, Body Dysmorphic Disorder -
Mention likely specific cause of such condition?
Genetic predisposition and societal pressure on thinness. -
Psychopathology mentioned case above?
Body image distortion, anxiety about weight gain -
What is two best investigation
- Biological: Electrolyte panel and BMI calculation
- Psychological: SCOFF questionnaire
-
What is two best Management/Treatment
- Biological: Nutritional rehabilitation with a structured meal plan
- Psychological: Family Therapy for 6 months