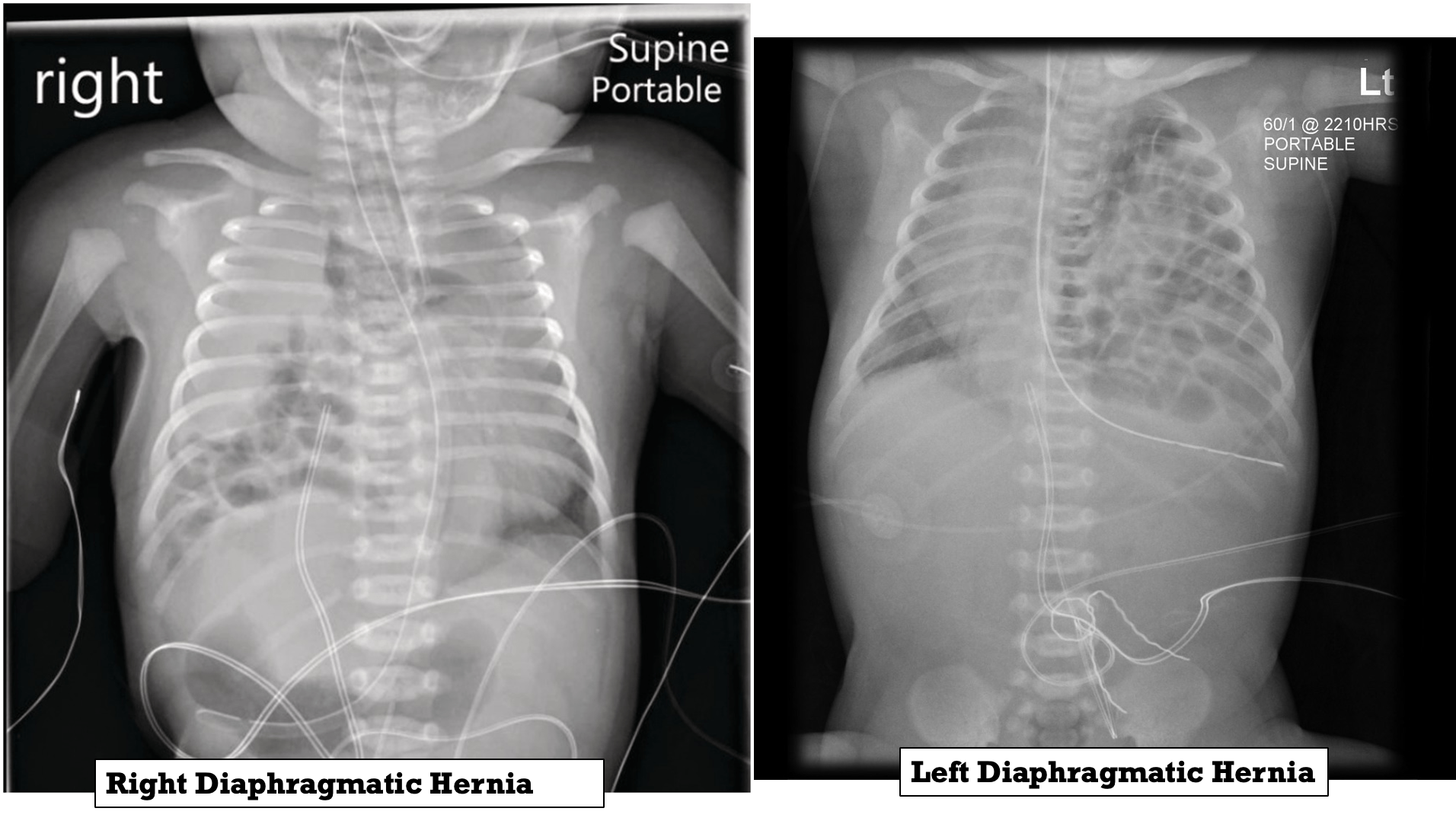
Diaphragmatic Hernia
Occurs when the diaphragm fails to completely close during development, allowing for abdominal contents to enter the chest cavity. 85% occur on the left side and 15% occur on the right side.
The ipsilateral lung is hypoplastic, and there will be a contralateral shift of the mediastinum, resulting in contralateral lung hypoplasia.
Types of Diaphragmatic Hernia
-
Bochdalek hernia: The most common type of congenital diaphragmatic hernia, a postero-lateral hernia, accounts for 70% of cases. more common and benign with better prognosis
-
Morgagni hernia: Occurs posterior to the sternum due to failure of sternal and costal fibers to fuse, accounting for 25%. liver shifted with bad prognosis
-
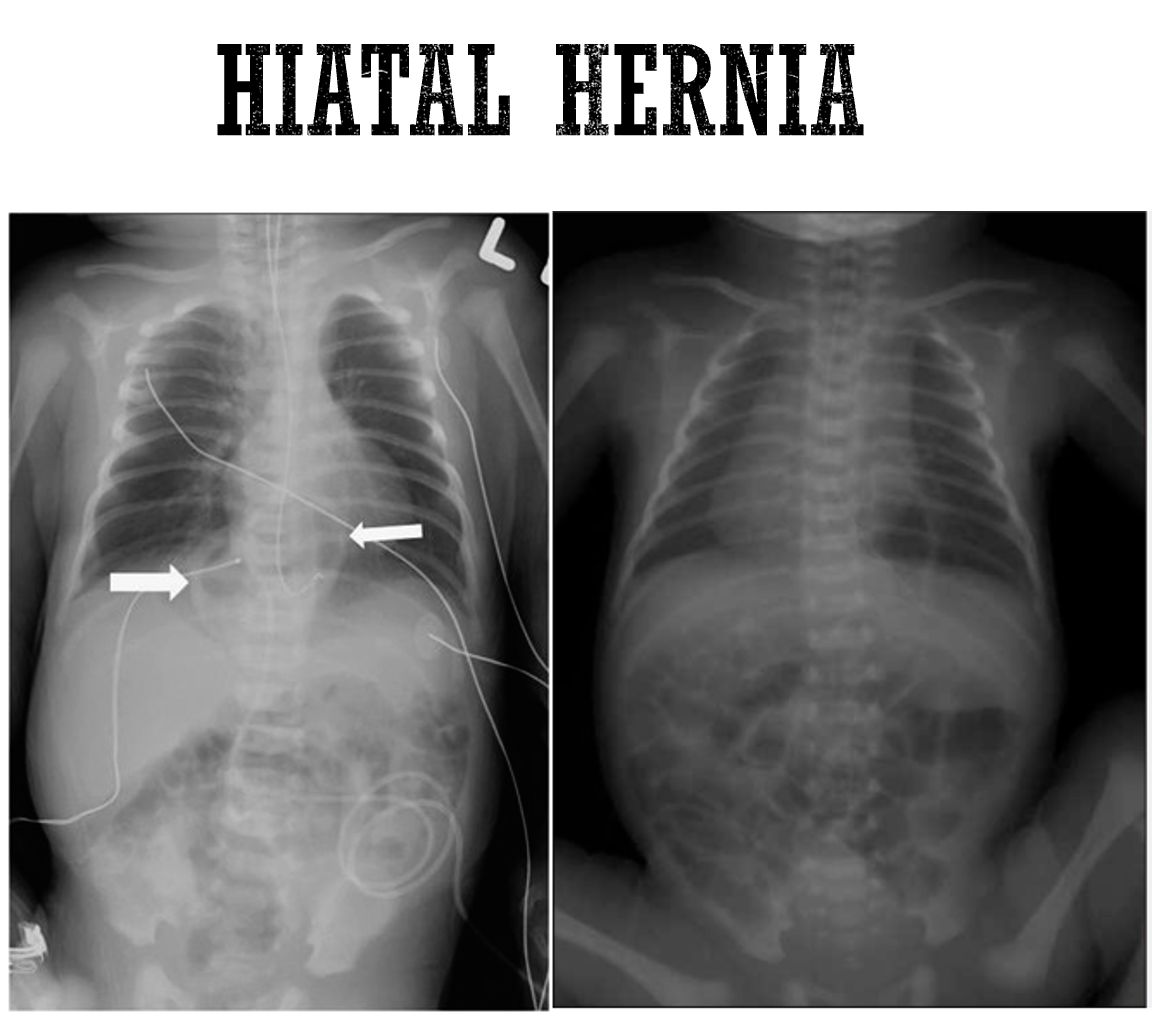
Hiatal hernia: Occurs through the esophageal hiatus.
Symptoms
Symptoms occur immediately after birth:
- Respiratory distress and irregular chest movements
- Decreased or absent breath sounds on the hernia side, and heart sounds displaced to the opposite side
- Cyanosis
- Bowel sounds may be heard in the chest with a decrease in breath sounds bilaterally
- Scaphoid abdomen
Diagnosis
- Antenatally by US
- Post delivery - Imaging studies:
- Chest radiography: to confirm diagnosis of congenital diaphragmatic hernia
- Cardiac and renal ultrasonography: to rule out associated anomalies
Complications
- Persistent pulmonary hypertension
- Lung hypoplasia
 A newborn with left congenital diaphragmatic hernia.
A newborn with left congenital diaphragmatic hernia.
Note the scaphoid abdomen and the barrel-shaped chest.

Management
- Avoiding mask ventilation (contraindicated) due air entering gastric content, which may aspirate to complicated pneumonia.
- Immediate endotracheal intubation after birth
- Immediately after intubation, Placement of orogastric tube and connecting it to continuous suction ***to prevent bowel distention and further lung compression. ***
- Continuous monitoring of oxygenation, BP, and perfusion.
- Vasoactive agents (e.g., dopamine, dobutamine, milrinone).
- Echocardiogram is a critically important imaging study, guiding therapeutic decisions by measuring pulmonary and systemic artery pressure. (tricuspid regurge)
- Surgical correction.
Diagnosis
A. Prenatal Ultrasound Diagnosis
-
Diagnosis earlier in gestation may correlate with a poorer prognosis due to severity of the condition.
-
Presence of liver in the thorax correlates with increased severity and poorer prognosis.
B. Postnatal Diagnosis
-
The diagnosis is made or confirmed by radiograph.
-
Echocardiography and appropriate studies for associated malformations should be done.
Complications
- Pulmonary hypoplasia
- Pulmonary hypertension
- Associated anomalies, especially congenital heart disease (CHD), neural tube defects, skeletal anomalies, intestinal atresias, and renal anomalies.
Factors associated with better prognosis are herniation of bowel into the chest after the 2nd trimester, absence of liver herniation, and absence of coexisting anomalies. The later the onset of postnatal symptoms, the higher the survival rate and better prognosis.