Surgical Infections & Antibiotics
Dr. Ahmed Khan
Factors Predispose to infections:
-
Adequate dose of the micro-organism.
-
Virulence of the organisms: the ability of bacteria to: a. Produce toxins (exotoxins, endotoxins) b. Resist phagocytosis (encapsulated organisms).
-
Susceptible host:
- Non-intact skin & mucous membrane.
- Poor inflammatory response.
- Poor acquired immunity.
- Suitable local environment: a. The presence of foreign bodies as prosthetic materials and devitalised tissues i ncrease the pathogenicity of microbes by impairing local defence mechanisms. b. Poor surgical technique.
Diagnosis of infection
Clinical features:
- Local features of inflammation (redness, hotness, pain, oedema and loss of function) which may not be all present.
- Systemic symptoms.
Investigations :
- BC, ESR (Men: 0 – 22, Women: 0 to 29 mm/hr), CRP (1-3 mg/L)
- Sample for gram stain & culture.
- Others.eg; serology & radiology.
Principles of treatment:
- Drainage of pus (I&D)
- Debridement of wounds (necrotic tissue).
- Removal of the source and foreign bodies.
- Supportive measures.
Surgical infections
-
Enterocolitis (Pseudomembranous colitis)
-
Lymphangitis
-
Hidradenitis suppurativa
-
Surgical site infection (SSI)
-
Nosocomial infections:(HAIs)
Antibiotics Policy:
Antibiotics are avoided in self-limiting infections. Choice is made according to the nature and sensitivity of the infecting organisms.
Single agent therapy is preferred to combination therapy and narrow spectrum agents preferred to broad spectrum agents whenever possible.
Adequate doses are given by correct route & at correct time intervals. Antibiotics used systemically must not be used topically.
Antibiotics are not used to treat abscesses unless adequately drained with a few exceptions like lung abscess.
Principles of Prophylactic antibiotic use:
The parenteral antibiotics used in prophylaxis should be given in sufficient dosage within 30 minutes preceding incision. This results in near maximum drug levels in the wound and the surrounding tissues during the operation.
Oral preoperative antibiotic only in the preparation of patients before elective colon surgery, the chosen agents should be given during the 24 hours before the operation in order to attain significant intraluminal (local) and serum (systemic) levels.
Prophylaxis should be short – often a single dose will suffice.
The current recommendation is to administer a second dose only if the operation lasts for longer than 2 - 3 hours.
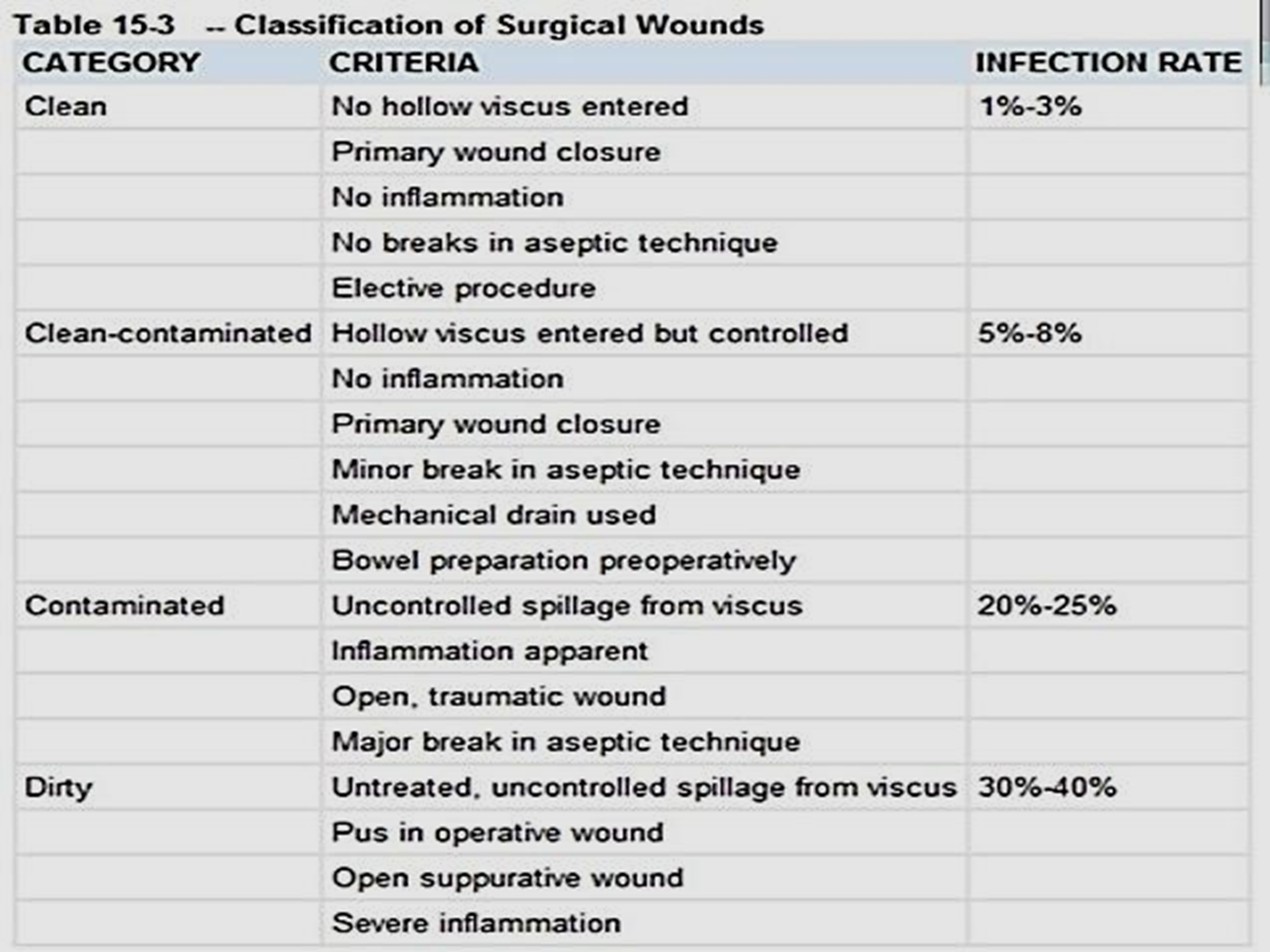
Most prophylactic antibiotics used in surgery are given to prevent wound infection in:
-
all clean-contaminated procedures; these include penetration of the gastrointestinal tract, whether by penetrating trauma or related to a pathological organ event (e.g., ruptured appendix, perforated colonic diverticulum) prior to the development of clinical peritonitis.
-
Clean operations with foreign body implant (e.g. vascular, cardiac and orthopaedic operations), and those without foreign body implants especially hernia repair, breast surgery, median sternotomy, vascular surgery involving the aorta and the lower extremities, and craniotomy.
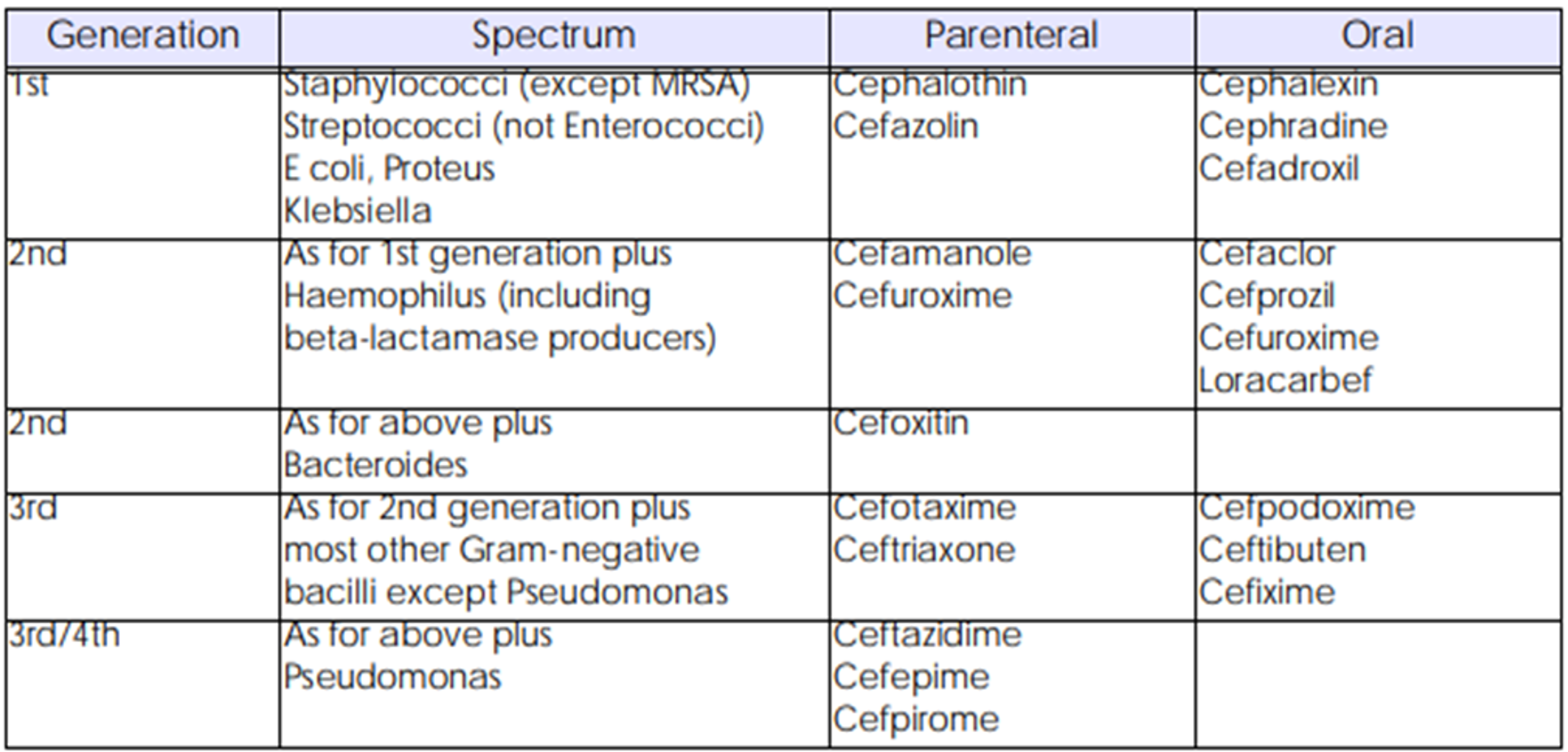
The use of wide spectrum antibiotics for prophylaxis should be avoided.
-
1st generation cephalosporin*** MUST be the preferred option. e.g. cefazolin 1 - 2 g pre-induction OR 2nd generation cephalosporins e.g. cefuroxime 1.5 g IV
-
During prolonged operations, additional intraoperative doses every 4 – 8 hours are indicated.
-
Some authors recommend continuing the antibiotic for up to 48 hours after the procedure (e.g. 1 - 2 g 8 hourly).
-
Vancomycin,only if there is a high rate of documented MRSA infections in the unit.
-
*Methicillin-resistant Staphylococcus aureus (MRSA) is a cause of staph infection that is difficult to treat because of resistance to some antibiotics. Staph infections—including those caused by MRSA—can spread in hospitals
Objectives
To be able to diagnosed, investigate and manage common community acquired infections.
To have a basic understanding of prevention and management of hospital acquired infection (nosocomial).
To have a basic understanding of the methods of Asepsis and its implications.
To have a guideline in the use of antibiotics for both therapy and prophylaxis and the awareness of main side effects of commonly used antibiotics.