Clinical Cases
Pediatric Cases and Management
Case 1: 14-Month-Old with Cyanosis
A 14-month-old baby presented to the ER. His mother noticed bluish discoloration of his lips, especially when he gets angry. He also puts his knee to his chin and gets relieved. Physical exam reveals systolic ejection murmurs and parasternal heave.
- a) Diagnosis: TOF (Tetralogy of Fallot)
- b) Investigation:
- Echocardiogram (echo)
- Electrocardiogram (ECG)
- Chest X-ray (CXR)
- c) Line of Management (until surgical correction): Prostaglandin
Bronchiolitis
- Relevant Questions for the Mother:
- 1- Ask about Cough, breathlessness, and wheeze?
- 2- Ask about feeding pattern?
- 3- Ask about recent URTI (Upper Respiratory Tract Infection)?
- 4- Ask about breastfeeding?
- 5- Ask about preterm history?
- 6- Ask about social history, including smoking and living in crowded conditions?
- Examination Findings:
- 1- Take vital signs (BP, PR, RR, O2 saturation, and fever).
- 2- Chest examination looking for wheezing and crackling sounds through the stethoscope.
- Investigations:
- 1- Blood gases
- 2- Chest X-ray
- 3- Culture of a sample of nasal fluid to determine the virus causing the disease.
- 4- Serology looking for RSV (Respiratory Syncytial Virus).
- Differential Diagnoses (DDx):
- 1- Bronchiolitis
- 2- Asthma
- 3- Pneumonia
- Management:
- 1- Admission
- 2- Supportive management directed toward symptomatic relief and maintenance of hydration and oxygenation.
- 3- Semi-sitting position
Case: 4-Month-Old with Respiratory Distress
A 4-month-old boy admitted through ER with a history of low-grade fever for 4 days, cough for 5 days, and respiratory distress for 3 days. The infant was born in the hospital with a birth weight of 2.5 kg and 35 weeks gestational age.
On examination: ill-looking, tachypnea with RR 52/min, tachycardia (HR .min), BP 90/50. His weight: 4.5 kg.
On chest examination: Expiratory wheeze, decreased bilateral air entry, and crackle sounds.
-
a- Write two relevant questions to ask the mother?
- Difficulty feeding
- Sweating
- Cyanosis
- Apnea
- Increasing coryza and congestion.
- Admission to NICU after birth.
- Any congenital cardiac disease in other siblings.
- Did he receive palivizumab to prevent respiratory syncytial virus infections.
- Parental smoking
-
b- What specific signs you should look for during examination of this infant?
- Respiratory distress signs: tachypnea, nasal flaring, retractions.
- Irritability
- Cardiac murmur
- Peripheral pulses.
- Fever.
- Hypoxia (oxygen saturation by Pulse oximetry)
- Plotting weight, height, and HC on growth chart.
-
c- What are the important investigations?
- Rapid viral antigen testing of nasopharyngeal secretions for respiratory syncytial virus
- Arterial blood gas analysis
- White blood cell count with differential
- C-reactive protein level
- Blood cultures
- Urine analysis, specific gravity, and culture
- Cerebrospinal fluid analysis and culture
- Serum chemistries
- Electrocardiography or echocardiography
- Chest radiographs
-
d- What is the most likely diagnosis and give two differential diagnoses?
- Most likely diagnosis: Acute bronchiolitis
- Differential diagnosis:
- Aspiration Pneumonia
- Asthma
- Bacterial Pneumonia
- Chlamydial Pneumonias
- Cystic Fibrosis
- Heart Failure
- Pediatric Sepsis
- Pertussis
- Viral Pneumonia
- Congenital heart disease
- Gastroesophageal reflux
-
e- Outline the management plan?
- Supplemental humidified oxygen
- Maintenance of hydration
- Mechanical ventilation
- Nasal and oral suctioning
- Apnea and cardiorespiratory monitoring
- Temperature regulation in small infants.
- Racemic epinephrine
- What relevant questions you should ask the mother? (2 Qs).
- 3 most important Qs:
- Hx of cyanosis.
- Hx of respiratory pattern.
- Hx of feeding pattern.
- Less important Qs:
- FHx of congenital heart disease.
- Hx of previous medications.
- Hx of previous admissions.
- 3 most important Qs:
- What things in examination you should look for?
- Vital signs (O2 sat by pulse oximeter, PR, BP).
- Cardiovascular examination (Femoral pulses, location of murmurs, grade of murmurs, maximum intensity of murmurs, liver size)
- What investigations you should order?
- CXR
- ECG
- Echo
- CBC
- What’s your DDx?
- Cyanotic congenital heart disease.
- Severe BA, bronchiolitis or pneumonia (but you should look also for respiratory involvement in the examination such as; wheezing, cough, crepitation or signs of respiratory distress in the examination).
- What’s your management?
- Admit
- Give IVF
- Give O2.
- While you’re examining this baby he got worse, what are you going to do? (OSCE Q).
- This baby is having cyanotic spells.
- First, Call for help!
- Then you can do knee-chest position (squat).
- Then O2, IVF and phenylephrine.
Case: 3-Month-Old with Down Syndrome
A 3-month-old girl with Down syndrome exhibits poor weight gain, tachycardia, tachypnea, and a low-pitched grade 2 systolic murmur. Oxygen saturation is 94% in room air. Chest radiography reveals cardiomegaly and increased pulmonary vascularity.
-
?Write two relevant questions, to ask the mother
- Feeding pattern
- Excessive sweating
- Cyanosis
- Family history of CHD (Congenital Heart Disease)
-
? What are the important investigations
- Echocardiography
- ECG
-
?What is the most likely diagnosis
- Complete atrioventricular septal defect
-
?Write 2 differential diagnoses
- VSD (Ventricular Septal Defect)
- ASD (Atrial Septal Defect)
-
? Outline the management plan
- Antifailure medications: Lasix, captopril, digoxin
- Extra calories (high caloric milk formula)
- Treatment of associated infection
- Correction of anemia
- Surgery: open heart surgery
Case: 4-Year-Old with Exercise Intolerance
A 4-year-old male presents in the office for a preschool physical examination. In the course of the interview, his mother mentions that he seems to get short of breath with exercise recently. It is especially noticeable during his swimming lessons when he tires before the other children do in his class. He has otherwise been in good health since his last physical exam in the previous year. Exam: T37.5, P92, R25, BP 97/70, oxygen saturation 98% in room air. Height and weight are at the 25th percentile. He is cooperative and well-nourished in no distress. HEENT and neck exams are normal. Heart: No palpable thrill, normal 1st and 2nd heart sounds; no clicks or rubs; grade 2/6 ejection systolic murmur heard along the left sternal border. Abdomen without no organomegaly or masses palpable. Genitalia: normal male. His neurological examination is normal He receives his immunizations, and tuberculin skin test
-
?Write two relevant questions, to ask the mother
- Any family history of congenital heart disease?
- Any excessive sweating noticed?
- Poor feeding or weight gain noticed?
-
? What are the important investigations
- Echocardiogram
- Blood pressure brachiofemoral delay
- ECG
-
?What is the most likely diagnosis
- Coarctation of the Aorta
-
?Write 2 differential diagnoses
- PDA (Patent Ductus Arteriosus)
- VSD (Ventricular Septal Defect)
- ASD (Atrial Septal Defect)
-
? Outline the management plan
- Prostaglandin E1 for early presentation
- Surgical late presentation: balloon angioplasty and stent
Case: 5-Hour-Old Newborn with Cyanosis
A 5-hour-old male newborn infant was born at 39 weeks gestation via vaginal delivery to a 23-year-old G2 P2 O+ mother with unremarkable prenatal serology studies. At 5 hours of age, with the second feeding, the baby appears tachypneic and cyanotic and he is therefore taken to the nursery for further evaluation. Exam: VS T 37.0, HR 145, RR 78, BP 67/38, oxygen saturation in room air. He is an alert active, mildly cyanotic term male 82% Tachypnea and mild nasal flaring are present. His heart is regular with a grade 2/6 systolic ejection murmur at the lower left sternal border. The precordium is quiet. Lungs are clear bilaterally. No hepatosplenomegaly is noted
-
?Write two relevant questions, to ask the mother
- Family history of congenital heart disease?
- Poor feeding and shortness of breath noticed in the last five hours?
- Pregnancy follow-up?
-
? What are the important investigations
- Oxygen saturation test
- ECG
- Chest x-ray
- Echocardiogram
-
?What is the most likely diagnosis
- Transposition of great vessels
-
?Write 2 differential diagnoses
- Tetralogy of Fallot
- Epstein anomaly
-
? Outline the management plan
- Prostaglandin to keep ductus arteriosus open
- Surgical procedure called atrial septostomy
Case: 3-Month-Old with Cyanotic Episodes Z
a 3 month old male infant who presents to the emergency department with a history of having episodes of excessive crying followed by limpness, cyanosis and fainting. He was born at 41 weeks of gestation by C-section because of failure to progress to a 23 year old mother G1P0. Apgar scores of 7 and 8 at 1 and 5 minutes, respectively. He had a two vessel cord and acrocyanosis. His cyanosis increased with crying. His oxygen saturations were 95% and stable. He was discharged from the hospital and followed in the office until this episode. He is now being hospitalized.
-
a- Write 3 relevant questions, to ask the mother?
- Feeding difficulty/weight
- Family history
- Congenital heart disease
- Developmental history
-
b- What specific signs you should look for during examination of this infant?
- Cardiac murmur (ejection systolic), single 2nd heart sound, bounding pulse, clubbing
-
c- What are the important investigations?
- Chest x-ray
- Echocardiogram
- ECG
- Cardiac catheterization
-
d- What is the most likely diagnosis and give two differential diagnoses?
- Tetralogy of Fallot
- All cyanotic heart diseases
-
e- Outline the management plan?
- Initial management is medical
- Definitive surgery at around 6 months of age.
prostaglanin works less than 1 months at 3 months, ask on family hx on safe side provoked with crying or feeding is it all over body or confined to the face two vessel check for dysmorphic feaetures is sthere any murmur pulses murmur cyanosis? tof differential diagnosus convulsion severe chest problem… mention lab + radiology in investigations for better mark
Case: 4-Month-Old with Mild Cyanosis and Murmur
A 4-month-old boy came to your clinic with his mother, and she told you that: “one doctor examined my child before and heard a cardiac murmur and referred me to you”. While examining this baby you noticed the baby has a mild cyanosis and murmur on auscultation.
- What relevant questions you should ask the mother? (2 Qs).
- 3 most important Qs:
- Hx of cyanosis.
- Hx of respiratory pattern.
- Hx of feeding pattern.
- Less important Qs:
- FHx of congenital heart disease.
- Hx of previous medications.
- Hx of previous admissions.
- 3 most important Qs:
- What things in examination you should look for?
- Vital signs (O2 sat by pulse oximeter, PR, BP).
- Cardiovascular examination (Femoral pulses, location of murmurs, grade of murmurs, maximum intensity of murmurs, liver size)
- What investigations you should order?
- CXR
- ECG
- Echo
- CBC
- What’s your DDx?
- Cyanotic congenital heart disease.
- Severe BA, bronchiolitis or pneumonia (but you should look also for respiratory involvement in the examination such as; wheezing, cough, crepitation or signs of respiratory distress in the examination).
- What’s your management?
- Admit
- Give IVF
- Give O2.
- While you’re examining this baby he got worse, what are you going to do? (OSCE Q).
- This baby is having cyanotic spells.
- First, Call for help!
- Then you can do knee-chest position (squat).
- Then O2, IVF and phenylephrine.
Heart Failure
- Relevant Questions for the Mother:
- 1- Ask about Difficulty feeding? Sweating?
- 2- Ask about expected growth.
- 3- Ask about Blue discoloration of lips or face?
- 4- Ask about Shortness of breath with exercise? (older children)
- 5- History of cardiac diseases?
- 6- Ask about previous medication and admission?
- Examination Findings:
- 1- Vital signs (O2 sat by pulse oximeter, PR, BP, temp)
- 2- Cardiovascular examination (femoral pulse, location of murmur, grade of murmur, maximum intensity of murmur, and liver size)
- Investigations:
- 1- CXR
- 2- ECG
- 3- ECHO
- 4- CBC, LFT & KFT
- Differential Diagnoses (DDx):
- 1- Congenital heart disease.
- 2- Cardiomegaly.
- 3- Acquired heart disease (e.g., Rheumatic fever).
- 4- Anemia
- Management:
- 1- Hemodynamic and Respiratory support in emergent cases.
- 2- Pharmacological:
- Inotropic agents: (Dopamine, Dobutamine).
- Diuretics: (Furosemide, Spironolactone).
- ACEI: (Captopril, enalapril).
- Digoxin.
- 3- Surgical:
- Palliative when no surgery is possible e.g., pulmonary artery banding.
- Definitive reparative surgery (for cardiac lesions).
- Heart Transplant
Case: 18-Day-Old with Down Syndrome
An 18-day-old girl with Down Syndrome presents with refusal to feed, tachypnea, and tachycardia. On examination, she has a 2nd-grade murmur.
-
Write two relevant questions?
- Family history of CHD
- Breathlessness
- Poor weight gain
- Sweating
- Feeding pattern
- Excessive sweating
- Cyanosis
-
What findings will you look for on examination?
- Tachypnea
- Tachycardia
- Soft pansystolic murmur
- Signs of heart failure
-
b- What are the important investigations?
- Echocardiography
- ECG
-
Mostly diagnosis?
- Large VSD or AVSD
-
What is your management plan?
- Antifailure: Lasix, captopril, digoxin
- Extra calories (high caloric milk formula)
- Treatment of associated infection
- Correction of anemia
- Surgery: open heart surgery
Case: 4-Month-Old with Poor Weight Gain
A 4-month-old girl, well child visit, mother complained about poor weight gain. Same problem with the first child. Husband is unemployed. Other development was normal. Mom alleged that feeding was going well (breastfeeding). Wt = 5kg. Went to ER at age 5 months, wt was “down”. Infant transferred to a children’s hospital for inpatient stay.
Case: 24-Hour-Old Infant of Diabetic Mother
A 24-hour-old infant, weight 4kg, whose mother was insulin-dependent, is slightly pale and cyanosed.
-
Q1: what’s the signs you will look for?
- SOB (Shortness of Breath)
- Tachycardia
- Tachypnea
- Edema
-
Q2: management for cyanotic case?
- Squat maneuver to increase vascular resistance
- O2
- Vasodilator (nifedipine)
- Diuretics
-
Q3: differential diagnosis?
- TGA (Transposition of the Great Arteries)
- Pulmonary atresia
- Tricuspid atresia
-
Q4: the hemoglobin 22 mg/dl. is it relevant?
- Yes, it’s relevant. The mother’s DM baby was overweight, which will lead to polycythemia.
-
Q5: investigations?
- ECG
- ECHO
- CXR
Bronchial Asthma
- Relevant Questions for the Mother:
- 1- Ask about the presence of symptoms (cough, wheezing, and dyspnea)?
- 2- Ask about a family history of asthma?
- 3- Ask about precipitating factors or conditions (respiratory tract infection, exercise, stress, weather, tobacco smoking, allergen, and inhaled irritant exposure)?
- 4- Ask about a personal history of other atopic diseases.
- 5- Environmental history.
- 6- Past medical history
- 7- Medication use, medical utilization.
- 8- Ask about school attendance and psychosocial factors
- Examination Findings:
- 1- Start by taking vital signs (BP, PR, RR, O2 saturation, and temperature).
- 2- Examination of the chest looking for dry cough, signs of respiratory distress, increased anterior-posterior diameter of the chest during air trapping, decreased air entry or wheezing, and prolonged expiratory phase.
OSPE
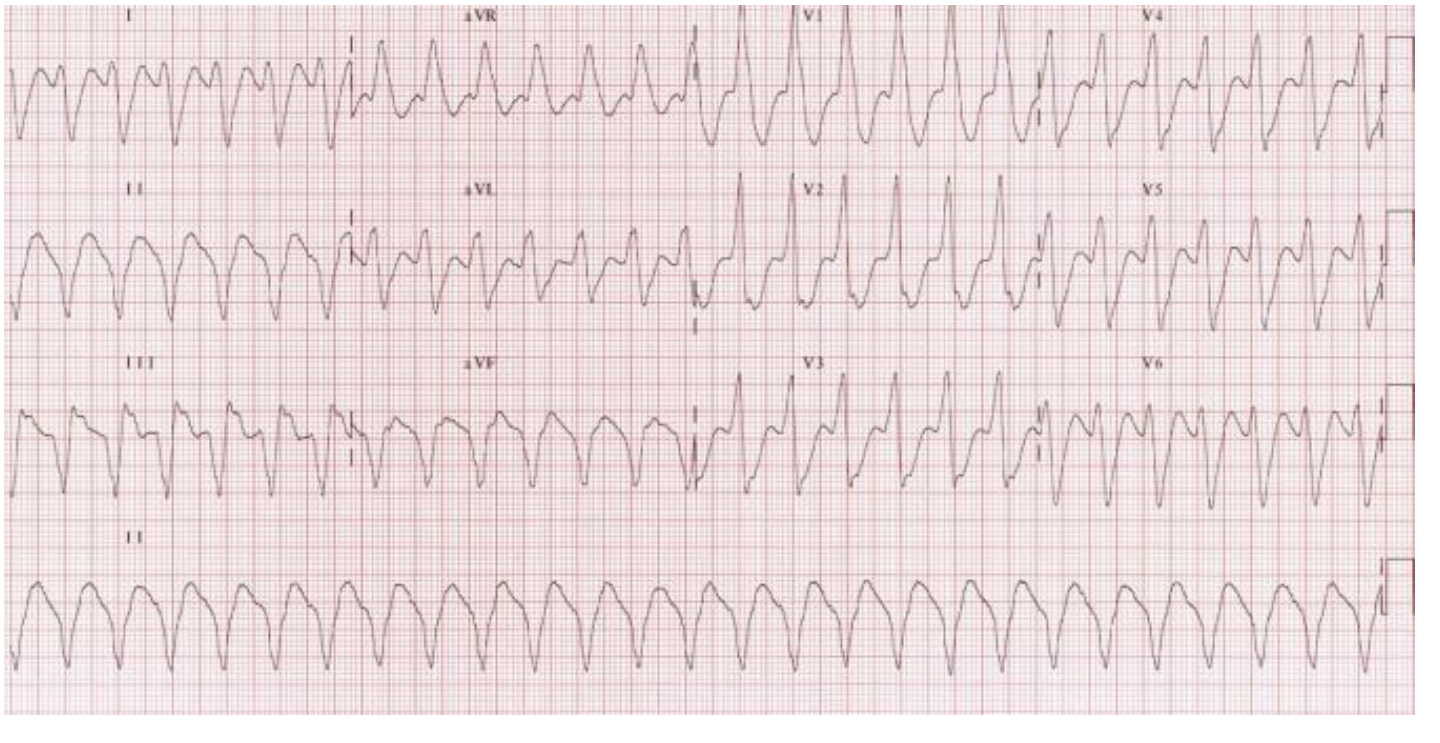
- List features?
- Tachycardia (HR: 150 bpm)
- Regular Rhythm
- Wide QRS complex
- Diagnosis?
- Monomorphic ventricular tachycardia
- Possible causes?
- Ischaemic heart disease
- Dilated cardiomyopathy
- Hypertrophic cardiomyopathy

- Describe the maneuvers done? Z
- The procedure is called “CardioPulmonary Resuscitation”.
- In the picture, it is done by 2 personnel.
- One is holding the bag valve mask to ventilate by doing C-E maneuver, “C-shaped fingers holding the mask, E-shaped fingers lifting the jaw”.
- The other person is performing compressions with 2 fingers ½ inch deep.
- What is the name of the device in the hand of the person at the upper end of bed?
- Bag valve mask
- In case of 2 rescuers, what is the compression-ventilation rate?
- 15 compressions and 2 ventilations.
VSD Murmur:
- At the 2-week checkup, a murmur is heard for the first time in an acyanotic well baby. The diagnosis of VSD with left-to-right shunt is made. The family is very upset with the physician for not having heard the murmur in the newborn period.
- Is the family justified? Why or why not?
- In newborns, there is a decrease in pulmonary vascular resistance (no murmur), but after 4-6 weeks, it will increase and cause a murmur.
- Is it possible that congestive heart failure will develop before the next regularly scheduled visit at 1 month? Yes, if it is a large VSD.
- Is pulmonary hypertension likely to be present at this time? NO
- Is the family justified? Why or why not?
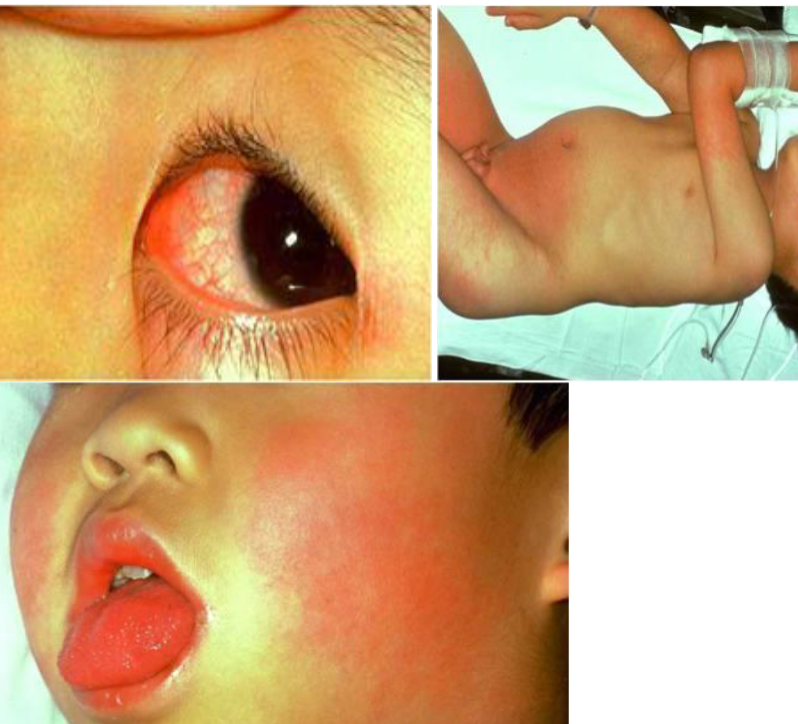
- A 20-month-old boy presents to the ER with a six-day history of fever, “red eyes”, and a rash. On exam, the patient is fussy with a T=39c. He has the following physical exam findings. Z
- Diagnosis: Kawasaki Disease - uncongug
- presents with red conjuctiva
- Complication: Coronary Artery aneurysm

- Describe? Edema of the hands and feet Z
- Rash: Maculopapular
- Bilateral bulbar conjunctival injection
- Erythema and cracking of lips, strawberry tongue
- Cervical lymphadenopathy, usually unilateral
- Diagnosis?
 Mid or Central Sternotomy Scar:
Mid or Central Sternotomy Scar:
- Description: Mid or central sternotomy scar - open heart surgeries (repair of septal defect or valve replacement) What is the most likely diagnosis? AVSD

Central Cyanosis
What is the observed clinical sign? Central cyanosis.
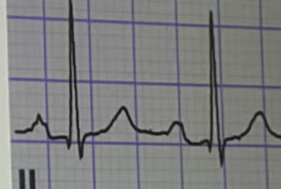 What is observed in the ECG? Prolonged P-R interval.
What is observed in the ECG? Prolonged P-R interval.
What are the possible diagnoses? Rheumatic fever or normal variant.

What is the test and what does it show?
- Diagnosis of Pneumothorax through transillumination

Newborn with abnormality and cardiac murmur
- What is abnormal? Central cyanosis in the limbs
- Diagnosis? CHD

Case
1st Sign ? Kawasaki disease 2nd sign ? Finger skin peeling Diagnosis ? Strawberry tongue.
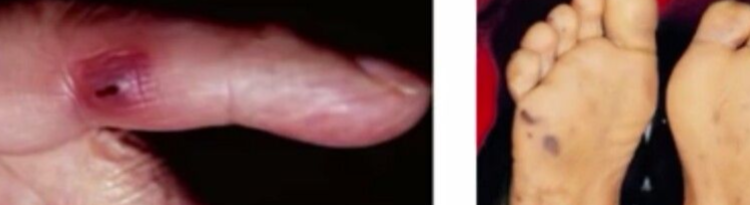
Case
Sign ? Janeway lesion Diagnosis ? infective endocarditis