Internal Medicine Dr Nada Abdelrahman
Coronary Artery disease
Definitions
- Coronary artery disease (CAD): IHD due to narrowing or blockage of coronary arteries.
- Stable angina: retrosternal, on exertion, mental stress, and/or exposure to cold and subsides within 20 minutes of rest or after administration of nitroglycerin X
- NSTEMI & UNSTABLE ANGINA: recent onset (<24 hr), deterioration of stable angina or at rest.
- Stable CAD: asymptomatic, stable angina; post-MI medically ttt
- Refractory angina: pain not controlled by medication
- Variant (Prinzmetal’s) angina (♀): due to spasm, ttt with CCBs x, associated with ↑ST (episode)
- Microvascular angina : Hx of exertional angina + positive exercise test & normal angiography.
Topics
Pathophysiology and mechanisms
 Mechanisms:
CAD can be caused
Mechanisms:
CAD can be caused
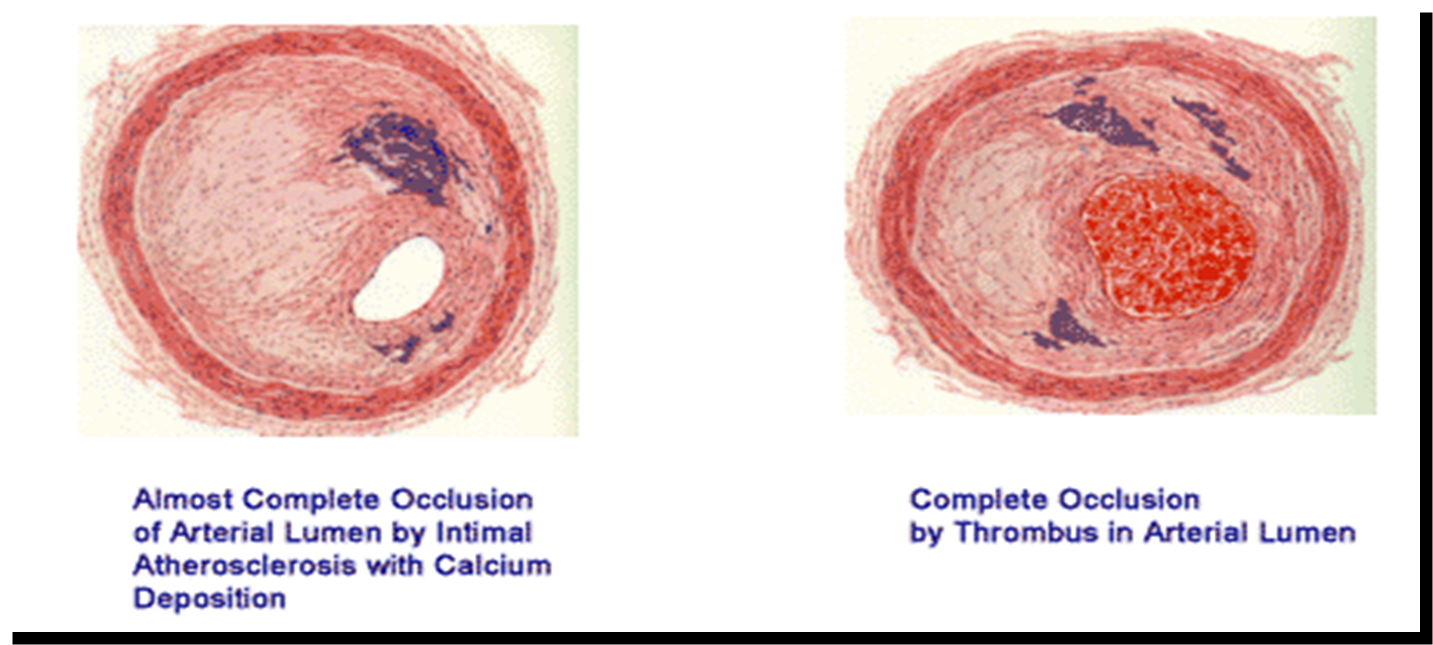
- Atheroma
- Thrombosis
- Embolus
- Spasm (reversible); cause in young male; cocaine
- Coronary ostial stenosis
Risk factors for CAD
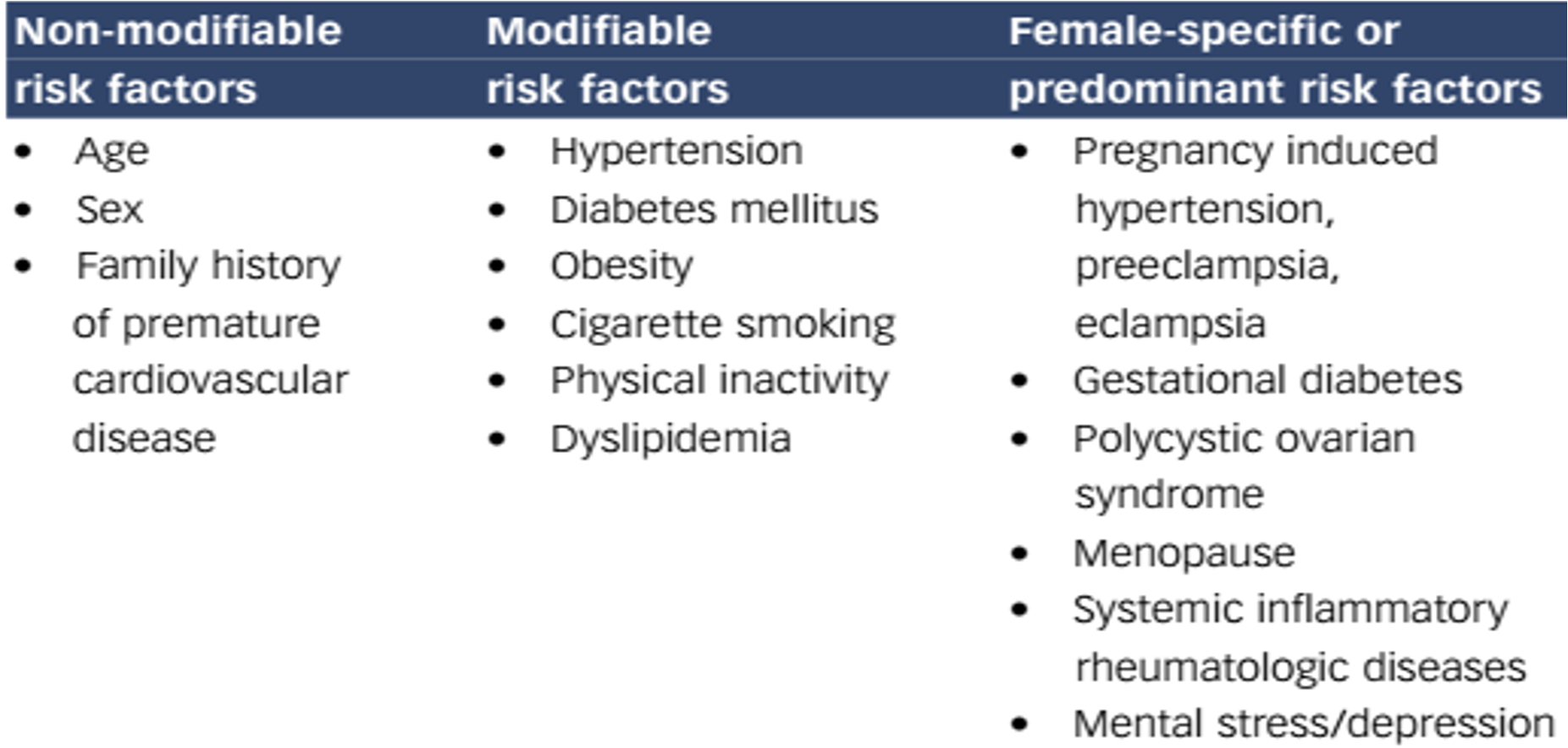 It is recommended that adult should do a minimum of 30 mins of moderate activity e.g. Brisk walking, cycling on 5 days of the week
It is recommended that adult should do a minimum of 30 mins of moderate activity e.g. Brisk walking, cycling on 5 days of the week
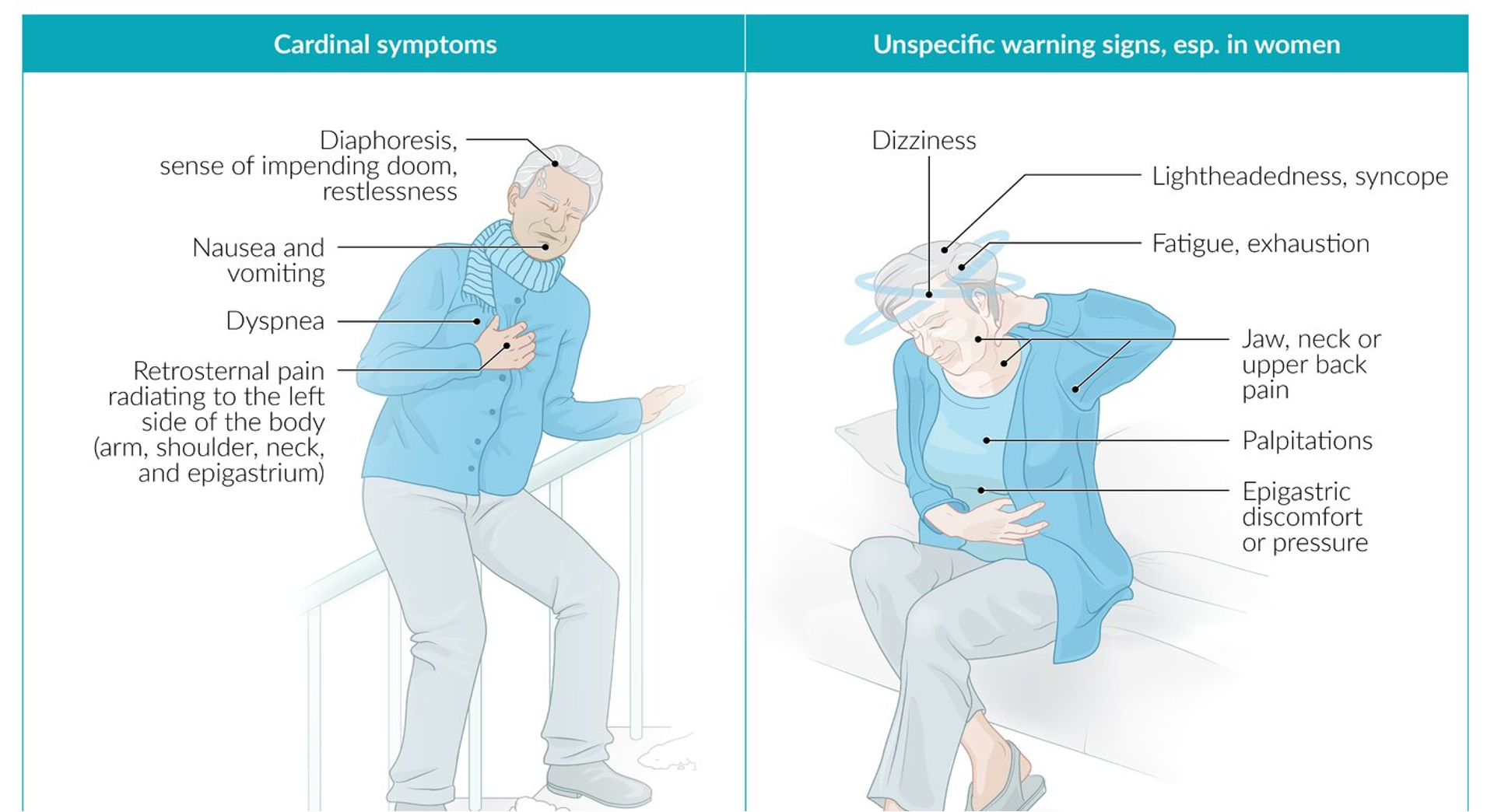
Clinical symptoms
- Angina: chest pain caused by myocardial ischemia.
- classically: left side
- Radiate: left arm or neck
- Absent (atypical): elderly, diabetic or female
- dyspnoea
- nausea and vomiting
- sweating
- palpitations
epigastric pain = inferior MI 40s+, female, htn, dm; usually vague typical chest pain - fatigue/ diziness - do ecg diabetes; there may be neuropathies subdue pain
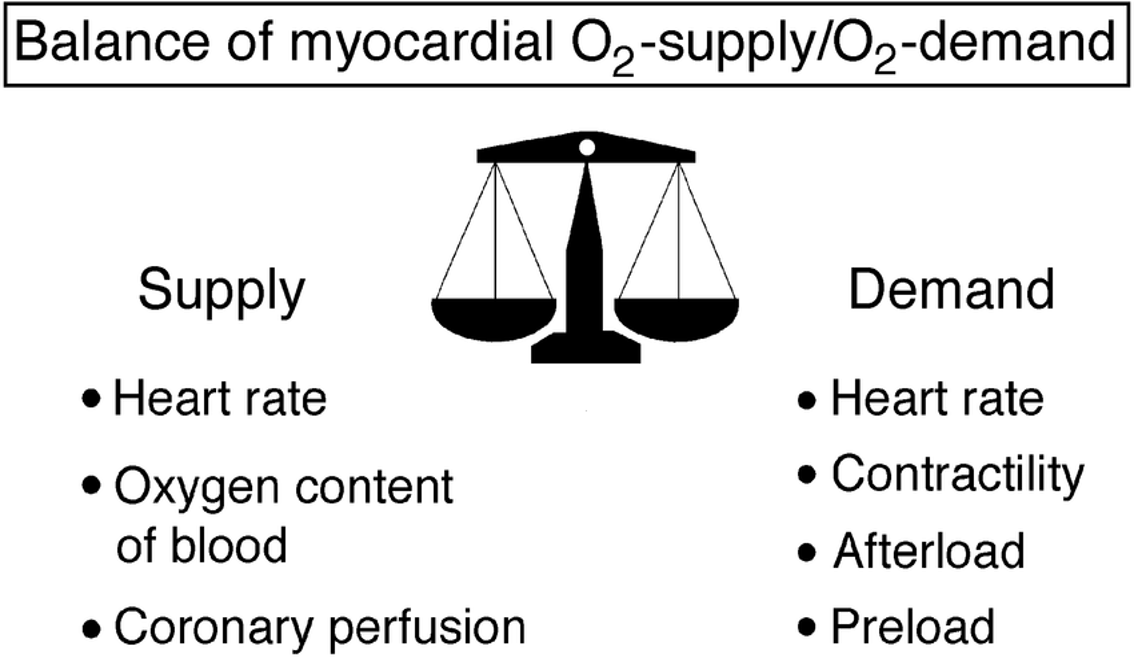
Decrease Supply - Anaemia - Carboxyhaemoglubinaemia - Hypotension
Increased demand
- increase cardiac output e.g. Thyrotoxicosis
- myocardial hypertrophy e.g. Hypertension,
- Aortic Stenosis
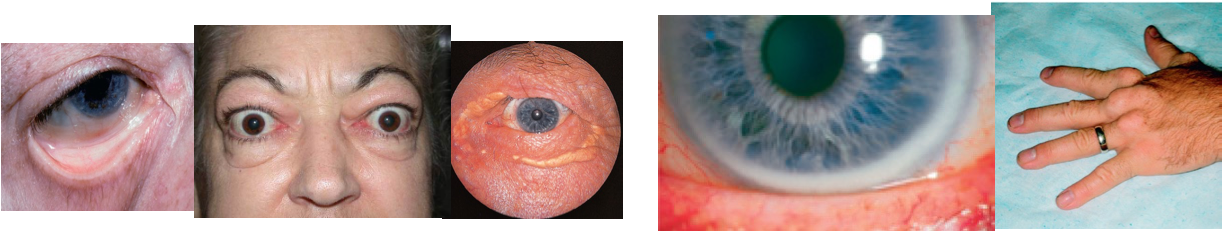
Physical examination
 No abnormal finding in angina
Look for
No abnormal finding in angina
Look for
- Anaemia
- Thyrotoxicosis
- Hyperlipidaemia (Xanthelasma,
Tendon Xanthoma) - Check for hypertension
- Examine CVS, exclude AS
Clinical scenario
A 58-year-old diabetic and hypertensive man presented with an intermittent painful retrosternal dullness for 4 weeks. The pain is recurrent and occurs on exertion or outside walking during cold weather. He experiences shortness of breath and palpitations during these episodes. The symptoms resolve spontaneously when he stops or sits down for a while. Over the past few days, the episodes have increased in frequency.
Physical examination: pulse is 88/min, respirations are 20/min, and BP: 144/90 mm Hg. A cardiac examination shows no abnormalities. Normal CXR. An ECG shows a normal sinus rhythm without any signs of ischemia. Normal cardiac markers. Which is your most likely diagnosis? cornorary artery disease
Therapeutics
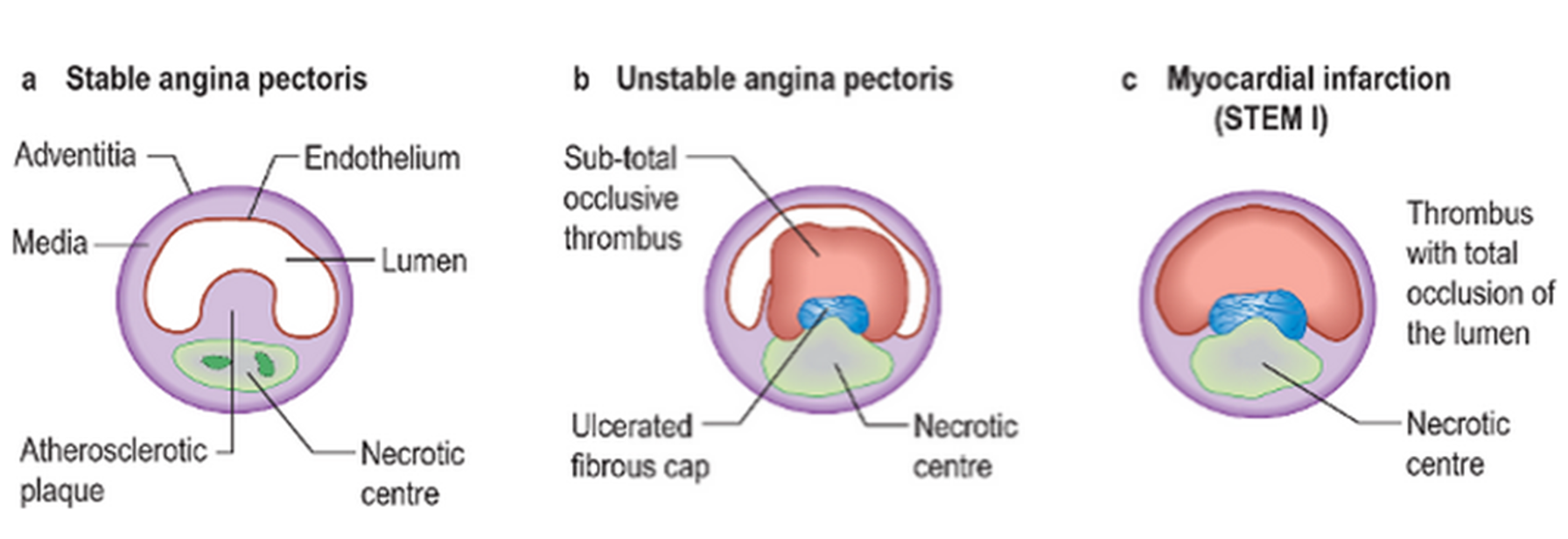
The degree of occlusion and ischemia determines the diagnosis
- Stable angina
- NSTEMI & UNSTABLE ANGINA (UAP)
- Non-ST elevation MI (NSTEMI)
- ST elevation MI (STEMI)
90% of AMI result of completely occluded vessel
Myocardial infarction is the death of part of the heart muscle due to its sudden loss of blood supply usually caused by thrombus formation on coronary atheroma
Classifications of MI Y
- According to the site and artery affected:
- Anterior ( left anterior descending)
- Lateral ( circumflex CA)
- Inferior ( Right CA) According to the duration:
- Recent
- Late pattern
- Old According to the extent of wall affection:
- Transmural
- Subendocardial According to the complications:
- Non-complicated
- complicated
ACS: histology
Physical findings: Y
-
a) Pallor is common, diaphoresis, fever during first week of MI.
-
b) Manifestation of sympathetic hyperactivity (tachycardia and/or hypertension) especially with anterior infarction.
-
c) Evidence of parasympathetic hyperactivity (bradycardia and/or hypotension) with inferior infarction.
-
d) However, hypotension occurs with right ventricular myocardial infarction or severe left ventricular dysfunction.
-
e) The pulse may be irregular because of ventricular ectopy, an accelerated idioventricular rhythm, ventricular tachycardia, atrial fibrillation or flutter, or other supraventricular arrhythmias; bradyarrhythmias may be present.
-
f) The precordium is usually quiet, however there may be signs of ventricular dysfunction (S4) and (S3).
-
g) Mitral regurgitation secondary to papillary muscle dysfunction.
-
h) A pericardial rub is heard in many patients with transmural MI.
COMPLICATIONS Y
Early:
- Arrhythmias all types most common is sinus tachycardia, VPCs
- Conduction defects
- LVF and pulmonary edema
- Cardiogenic shock
- Myocardial rupture
- Pericarditis and hemopericardium
- Acute MR
- Acquired VSD
- Mural thrombi and systemic embolization
Late:
- Dressler syndrome
- Post MI angina
- Frozen shoulder
- Ischemic cardiomyopathy
Investigations:
ECG: It may show:
- ST segment elevation or depression.
- T wave inversion
- Pathological Q wave.
NB: When coronary artery occlusion is not totally occluded, ST segment is not elevated and Q wave will not develop (non-Q wave M.I.).
Cardiac enzymes: are elevated.
-
C K “creatine kinase” rises within 4-8 hr. for 48 hr. MB isoenzyme of CK is more specific as it is found mainly in cardiac muscle.
-
Troponin T & I: protein of sarcomere, not normally present in blood. Rises 2-4 hr. after infarction, remain raised for 5 to 14 days. Their long persistence has allowed them to replace lactic dehydrogenase for diagnosis of MI.
Echocardiography: I- Assesses global and regional cardiac function. 2- Evaluates suspected complications of acute Ml. Non specific laboratory tests: Polymorphonuclear leucocytosis ( 12,000 to 15,000 /µL),
C-reactive protein and ESR increase with acute MI.
Diagnosis:
At least 2 of the following 3 criteria:
- Classic chest pain
- ECG changes
- Positive biomarkers