digitalis
Mechanism of action:
Positive inotropic action:
-
Digitalis ↑ cardiac contractility by increasing free intracellular Ca2+ through inhibition of membrane-bound Na+/K+ ATPase enzyme. This result in inhibition of Na+/K+ pump with subsequent accumulation of intracellular Na+ and Ca2+ via:
-
↑ Ca2+ release from the sarcoplasmic reticulum.
-
Displacement of intracellular Ca2+ from its binding sites.
-
↑ Ca2+ entry into the cardiac ms cells.
-
↓ exchange of extracellular Na+ for the intracellular Ca2+.
Autonomic effects:
It restores the vagal tone and abolishes the sympathetic over activity.
a. Vagal actions:
- Direct stimulation of central vagal nucleus.
- Reflex vagal stimulation due to increased sensitivity of baroreceptors.
b. Sympathetic action:
- In therapeutic doses, digitalis reduces sympathetic discharge to the heart but toxic doses may increase cardiac sympathetic activity.
Pharmacological effects:
CVS: ↑↑ Cardiac contractility and COP leading to better tissue perfusion.
HR: Bradycardia due to:
- Vagal effect: …..see before
- Extravagal effects: Direct inhibition of the A-V conducting system. ↓ sympathetic discharge to the heart due to relieve of hypoxia and improved hemodynamics
Conduction velocity:
- Atrial conduction: small dose ↑ it (vagal stimulation) but toxic dose ↓ it (direct effect).
- A-V conduction: ↓↓ by direct and vagal effects.
Kidney effects:
- ↑ diuresis “The best diuretic in case of CHF is digitalis” due to:
- ↑ COP → ↑ RBF and ↑ GFR.
GIT effects:
- Stimulation of CTZ → nausea and vomiting. = Anorexia and diarrhea.
CNS effects:
- CNS stimulation → excitation and convulsions (in high dose).
- Stimulation of the visual area causing yellow vision
Therapeutic indications:
Absolute:
-
They can be used in case of rapid ventricular rate and other therapeutic options e.g beta blocker fail or contraindicated. The major indication is chronic CHF associated with atrial fibrillation.
-
In patients who have symptoms of heart failure in spite of vasodilators, beta blockers and diuretics. Treatment of heart failure failing to respond to other drugs.
Relative:
- Atrial flutter: (the atria beat regularly at 200-400 bpm) due to: ↓ A-V conduction and protects the ventricles from the accelerated atria. Improvement of ventricular function.
2) Atrial fibrillation: (the atria beat irregularly at 400-600 bpm) The same mechanism as atrial flutter. 3) Paroxysmal atrial tachycardia: To ↓ A-V conduction → protects the ventricles from the accelerated atria.
Absolute contraindications:
-
Heart block: because digitalis ↓ conduction by direct and vagal effects.
-
Hypertrophic obstructive cardiomyopathy (IHSS): because increasing cardiac contractility will ↑ the outflow tract resistance and accelerate heart failure.
-
Wolff-Parkinson-White (WPW) syndrome: although digitalis (also BB and verapamil) ↓ conduction in the normal pathway, they can ↑ conduction in the abnormal pathway leading to ↑ arrhythmia
-
Paroxysmal ventricular tachycardia: because digitalis ↑ excitability and automaticity.
Other Relative Contraindications:
(= Factors modifying the response to digitalis)
-
Bradycardia or sick sinus syndrome…. Severe bradycardia may occur.
-
Hypersensitive carotid sinus…………. Severe bradycardia may occur.
-
With beta-blockers or with verapamil… Severe bradycardia may occur.
-
In hypertensive HF: digitalis will ↑ the strain of the left ventricle.
-
Cardiopulmonary diseases: pulmonary hypertension, chronic lung disease, severe hypoxia, etc.
-
Renal or hepatic diseases: digoxin must be avoided in renal patients while digitoxin must be avoided in hepatic patients.
-
Myxedema: renders the heart more sensitive to digitalis.
-
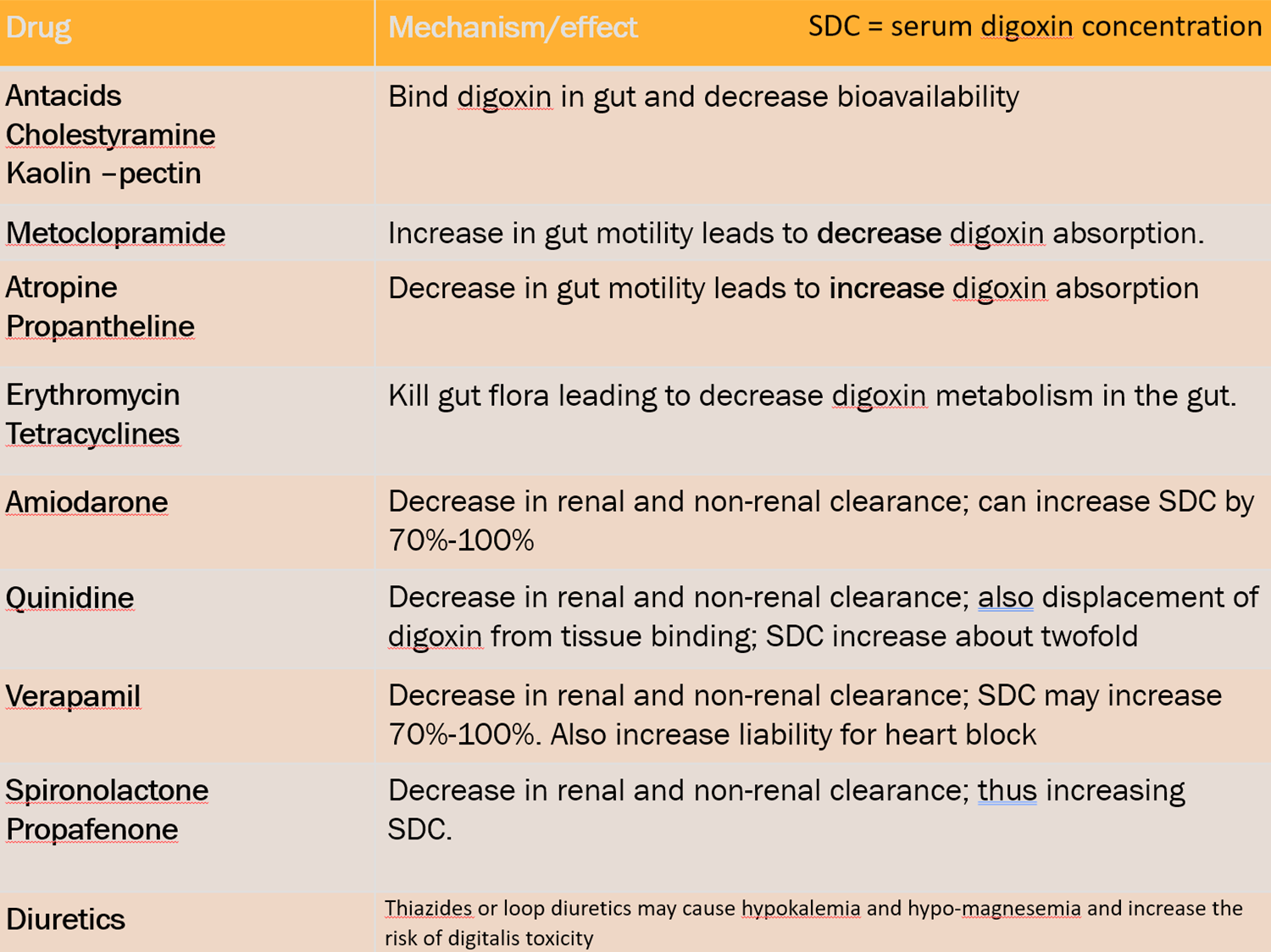
Concomitant drugs: Narrow therapeutic index
Dosage and administration:
1-Initial digitalization:
- Slow (cumulative) method:
- It is done by giving the daily maintenance dose (one tablet 0.25 mg /day → 5 days/week) from the start.
- The steady state plasma conc (Cpss) will be achieved after 5 half-lives (i.e. after one week for digoxin and after one month for digitoxin).
- It is the safest method for digitalis administration.
2-Rapid (loading) method:
- It is done to achieve early Cpss and in emergency conditions e.g. in acute heart failure or in rapid AF.
- 2 tablets (0.5 mg) twice daily for 2 days then maintain on one tab/d (2x2x2)
- 2 tablets (0.5 mg) t.d.s for one day then maintain on one tab/d (2x3x1)
3- Maintenance dose: 0.25 mg/day, 5 days/week (AF requires slightly higher dose).
N.B
- The optimum therapeutic plasma level is 1-2 ng/ml
- Arrhythmia occurs when level exceeds 2 ng/ml
Evaluation of EffectivenessAssessment of response to digitalis:
- Relief of dyspnea and orthopnea.
- Relief of tachycardia and tachypnea.
- Relief of edema, lung congestion, and fatigue.
- Increased urinary output
- Improved peripheral pulses.
- Serum digoxin levels 0.5 to 2 ng/mL.
Precautions during digitalis therapy:
-
Never give digitalis i.v. before being sure that the patient has not received digitalis during the last 14 days to avoid digitalis toxicity
- Continuous monitoring of plasma K+ level.
- Reduce digoxin dose in elderly people because renal function is ↓.
- Other factors modifying the response to digitalis.
Management: Stop digitalis administration.
Correct hypokalemia:
- Stop drugs that cause hypokalemia (e.g. diuretics).
- Give K+ either i.v. or oral (2 gm/4 h).
Antiarrhythmic drugs:
-
Lidocaine (ventricular arrhythmia): 1-2 mg/kg i.v. bolus then 1-2 mg /min i.v.i.
-
Phenytoin (in ventricular arrhythmia): 100 mg i.v.i. (anti-arrhythmic of choice).
-
Atropine: if there is bradycardia or heart block.
-
Beta-blockers: if there is tachyarrhythmia.
Specific digitalis antibodies (Fab fragments) to bind digitalis and ↑ its excretion (the most specific therapy).
Prevention of digitalis toxicity:
- Avoid predisposing factors (all…………….).
- Therapeutic drug monitoring for digitalis therapy (mention therapeutic level)
- Allow weekly drug holiday (2 days/week) to prevent digitalis cumulation.
- if bradycardia (heart rate less than 60 bpm) or new arrhythmias occur. No drug intake
Laboratory Values:
- Electrolyte imbalance: potassium, calcium and magnesium values need to be monitored
- Hypokalemia (low potassium)
- Hypomagnesemia (low magnesium)
- (Both can lead to irregular heart rate).