Approach to Hematuria
Dr. Salma Elgazzar
Learning Objectives
- Define hematuria.
- Discuss the methods of detection of hematuria.
- Recognize the general classification of hematuria.
- Discuss the commonest causes of hematuria in pediatrics.
- Discuss the key components from the history and physical examination in evaluating a child with hematuria.
- Identify the distinguishing features between glomerular and non-glomerular causes of hematuria based on urine analysis.
- Formulate an appropriate management plan to evaluate an infant with hematuria.
- List the indication of renal biopsy in the evaluation of hematuria.
Definition
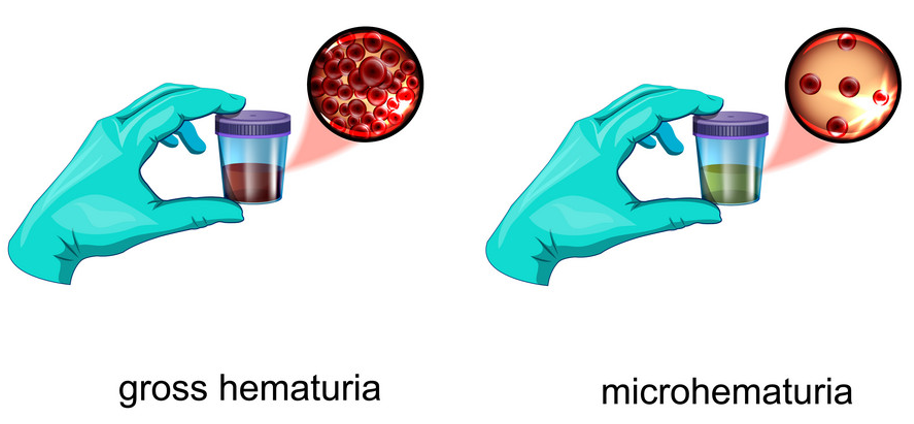
Hematuria is defined as the persistent presence of more than five red blood cells (RBCs) per high-power field (hpf) on freshly voided and centrifuged urine. It occurs in 4–6% of urine samples from school-age children.
- Microscopic hematuria: Urine appears normal.
- Gross hematuria: Blood visible to the naked eye.
Important Question
Is it true hematuria? Or any colored urine?
To Answer the Question
-
History & Clinical Examination + Check urine for blood by dipstick & microscopic examination
-
Positive hemostick and negative RBCs by microscopic could be either:
- Hemoglobinuria
- Myoglobinuria
-
Positive RBCs in microscopic examination means real hematuria.
-
Heme negative, negative RBCs by microscopy:
- Foods: Beet roots, blackberries.
- Drugs: Rifampicin, Desferal, Nitrofurantoin.
- Urate crystals (red diaper).
-
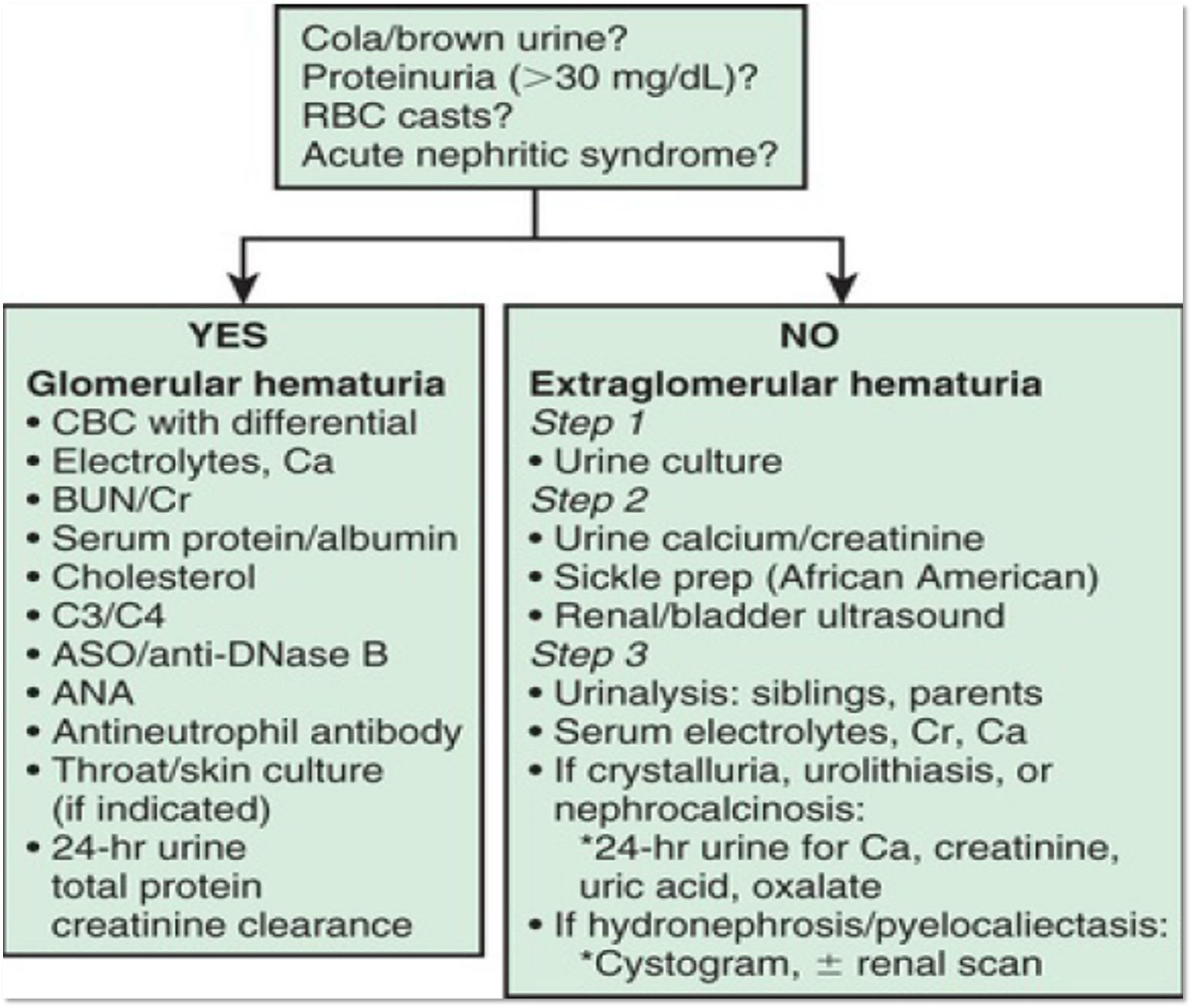
Non-glomerular & glomerular
| Category | Nonglomerular Causes | Glomerular Causes |
|---|---|---|
| Causes | - Infection (bacterial, viral, tuberculosis, schistosomiasis) | - Acute glomerulonephritis (usually with proteinuria) |
| - Trauma to genitalia, urinary tract, or kidneys | - Chronic glomerulonephritis (usually with proteinuria) | |
| - Stones | - IgA nephropathy | |
| - Tumors | - Familial nephritis, e.g., Alport syndrome | |
| - Sickle cell disease | - Thin basement membrane disease | |
| - Bleeding disorders | ||
| - Renal vein thrombosis | ||
| - Hypercalciuria | ||
| Characteristic | Non-Glomerular Hematuria | Glomerular Hematuria |
| Urine Color | Red dark urine | Brown or tea-colored (coca-colored) urine |
| Casts | Blood clots | Red blood cell casts, cellular casts, tubular cells |
| Proteinuria | No proteinuria or < +2 in the absence of gross hematuria | Proteinuria > +2 by dipstick in the absence of gross hematuria |
| RBC Morphology | Normal morphology of erythrocytes | Dysmorphic RBCs by phase contrast microscopy |
| Erythrocyte Volume | Erythrocytes volume > 50 | Erythrocyte volume < 50 |
Presentations
-
UTI Pathophysiology & Etiology
-
Acute Post-Streptococcal Glomerulonephritis
-
IgA Nephropathy
-
Alport Syndrome
-
Henoch–Schönlein Purpura
Common Causes of Gross Hematuria
- Urinary tract infection
- Meatal stenosis with ulcer
- Perineal irritation
- Trauma
- Urolithiasis
- Hypercalciuria
- Obstruction
- Coagulopathy
- Tumor
- Glomerular disease
- Postinfectious glomerulonephritis
- Henoch-Schönlein purpura nephritis
- IgA nephropathy
- Alport syndrome (hereditary nephritis)
- Thin glomerular basement membrane disease
- Systemic lupus erythematosus nephritis
Y OSCE
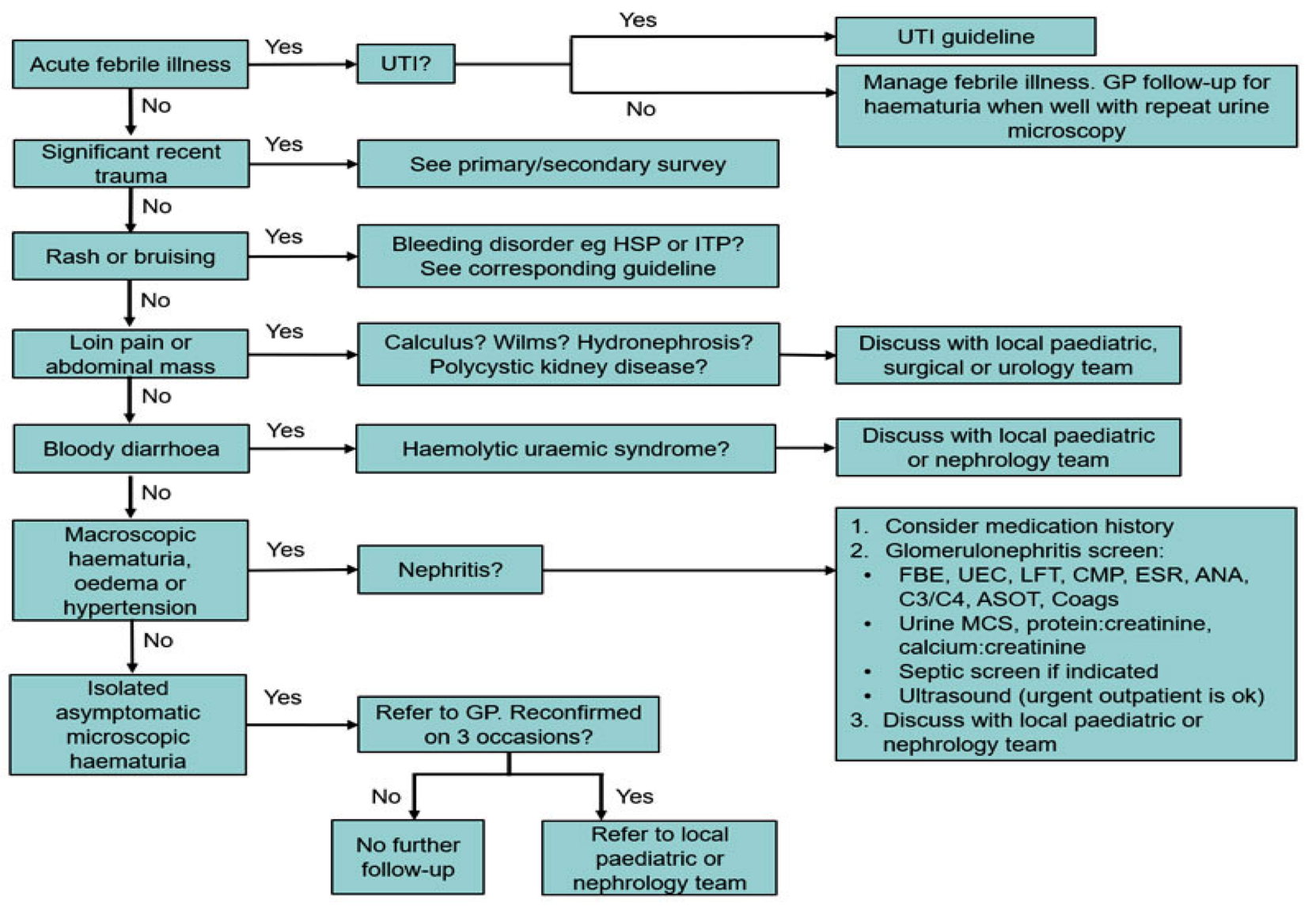
Evaluation of the Child with Hematuria
History
Patients with hematuria can present with a number of symptoms:
- Tea- or cola-colored urine
- Facial or body edema
- Hypertension
- Oliguria
- Flank pain
- Frequency, dysuria
- Unexplained fevers
- Renal colic
- Headache
- Mental status changes
- Visual changes (diplopia)
- Epistaxis
- Heart failure
- Rash and joint complaints
Open questions about the chief complaint:
- Color: Pink to red (extra glomerular), brown cola-colored (glomerular), smell, stones, clots (extra glomerular)
- Phase of urination, duration of the problem
- Time at night or with activity
- Frequent & amount in each episode of urination or not
- Previous similar problem
- Recent history of:
- Recent febrile illness
- Recent pharyngitis
- Recent streptococcal skin infection
- Recent trauma, menstruation, or strenuous exercise
- Association symptoms (fever, dysuria, pain, edema, headache, weight loss, fatigue, FTT, pallor, jaundice)
Systemic Review
- Respiratory system (URTI): IgA GN, post-GABS
- CVS: Exercise intolerance, fatigue (acute secondary to HTN), infective endocarditis
- GIT: Bloody diarrhea HUS, abdominal mass
- CNS: Headache, loss of consciousness, convulsion e.g., hypertensive encephalopathy
- Musculoskeletal: Arthritis e.g., SLE
- Skin: (rash/ HSP) (photosensitivity / SLE), (petechial / bleeding tendency) (skin infection / post-strep) (Jane way & Osler nodules / infective endocarditis)
- Eyes & Ear: Deafness, cataract & keratoconus e.g., Alport syndrome
- Hematology: Bleeding tendency, sickle cell anemia. Hb urea: Intravascular hemolysis e.g., G6PD & PNH
Past History
- Medical history: Kidney diseases, recurrent URTI, trauma & exercise
- Drug hx & food intake
- Developmental history: Deafness / Alport syndrome
- Family History: H.urea, renal diseases, tendency to form stones, deafness / Alport syndrome
Physical Examination
Physical examination may also suggest possible causes of hematuria.
- Temperature
- Measuring blood pressure: Presence of hypertension, edema, or signs of heart failure suggests acute glomerulonephritis.
- Abdominal masses may be:
- Bladder distention in posterior urethral valves
- Hydronephrosis in ureteropelvic junction obstruction
- Polycystic kidney disease, or Wilms tumor
- A flank mass: Hydronephrosis, renal cystic diseases, renal vein thrombosis, or tumor
- Several malformation syndromes are associated with renal disease.
Rash and Joint Complaints
- HSP or SLE nephritis
Eye Examination
- Visual changes (diplopia) may be associated with severe hypertension.
- Alport syndrome: Anterior lenticonus, cataract, fundus
Perineum and Urethral Meatus
- Anatomic abnormalities of the external genitalia
- Unexplained perineal bruising and hematuria: Child abuse must always be suspected.
Investigations
All Patients
- Urine microscopy (with phase contrast) and culture
- Protein and calcium excretion
- Kidney and urinary tract ultrasound
- Plasma urea, electrolytes, creatinine, calcium, phosphate, albumin
- Full blood count, platelets, coagulation screen, sickle cell screen
If Suggestive of Glomerular Hematuria
- ESR, complement levels, and anti-DNA antibodies
- Throat swab and antistreptolysin O/anti-DNAse B titres
- Hepatitis B and C screen
- Renal biopsy if indicated
- Test mother’s urine for blood (if Alport syndrome suspected)
- Hearing test (if Alport syndrome suspected)
Indication of Renal Biopsy in the Evaluation of Hematuria
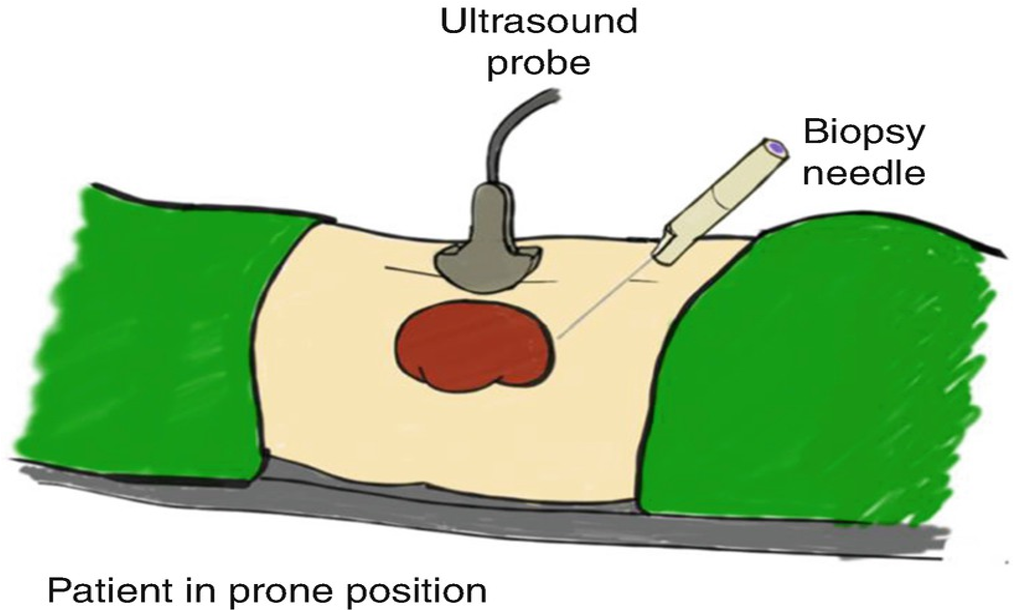
A renal biopsy may be indicated if:
- There is significant persistent proteinuria
- There is recurrent macroscopic hematuria
- Renal function is abnormal
- The complement levels are persistently abnormal
- Lupus nephritis
- Unexplained acute renal failure