Table of Contents
- How to Read Musculoskeletal X-Rays
- Prof. Mamoun Kremli
- Dr. Tarif Alakhras
- Introduction
- X-ray Request Form
- Example of X-ray Request Form
- Reading X-rays
- General Information
- Reading Bone
- Reading Bone (Continued)
- Reading Bone (Continued)
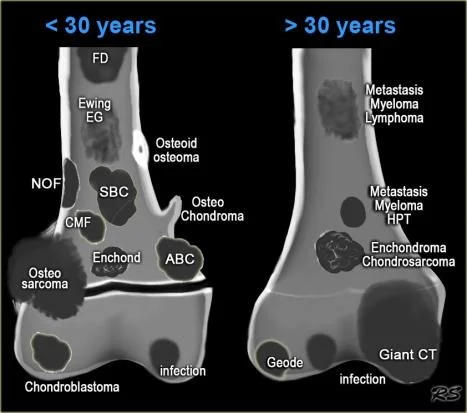
- Bone Destruction by Age
- < 30 years
-
30 years
- Reading Joints
- Joint Position
- Joint Relations
- Reading Joint Anatomy
- Bone and Joint Alignment
- Joint Space
- Bone and Joint
- Soft Tissue Reading
- Look for the Unexpected
- Artifacts Obscuring Diagnosis
- The fabella - Normal
- Bipartite patella - Normal
- Reading Joints (Continued)
- Patellar position
- Reading Joints (Continued)
- Arthroplasty
- Infected arthroplasty
- Reading of bone lesions
- Location
- Radiographic features
- The Border
- The Matrix
- Type of Bone Destruction
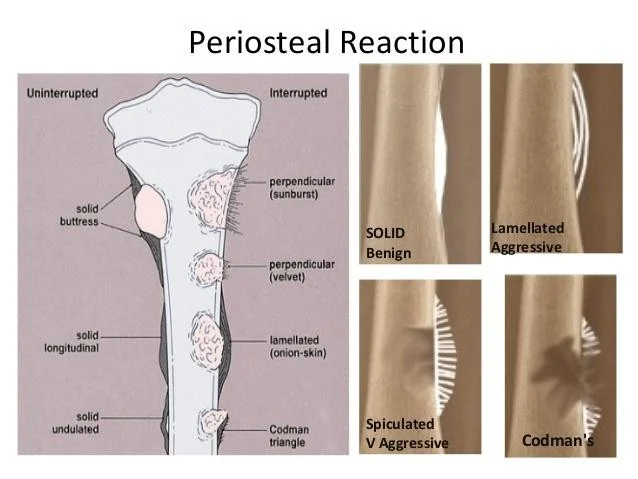
- Type of Periosteal Reaction
- Soft Tissue Extension
- Benign Vs. malignant
- Type of Periosteal Reaction (Continued)
- Type of Periosteal Reaction (Continued)
- Bone Lesions and Imaging
- Overview of Bone Lesions
- Case Studies
- Case 1: 45-year-old Lady with Knee Pain
- Case 2: 15-year-old Boy - Asymptomatic
- Case 3: 12-year-old Boy with Swelling Lower Leg
- Case 4: 45-year-old with Pain R Thigh
- Case 5: 45-year-old with Pain R Thigh - Osteomyelitis
- Case 6: 2-year-old with Fever, Vomiting, Pain L Hip
- Case 7: 2-year-old with Fever, Pain L Hip - Septic Arthritis
- Case 8: 10-year-old with Pain L Hip
- Case 9: 10-year-old with Pain L Hip - Osteoid Osteoma
- Case 10: 17-year-old with Painful Swelling Lower Thigh
- Case Studies
- Other Imaging Techniques
- Overview
- Summary of Key Points
- General Guidelines
- Reading Bone Lesions
- Reading Joints
- Resources
- Overview of Bone Lesions
How to Read Musculoskeletal X-Rays
Prof. Mamoun Kremli
Dr. Tarif Alakhras
Introduction
- X-rays are part of diagnostic tools
- When requesting an X-ray, information given (written) helps in reaching a diagnosis
- Important points in history
- Relevant physical findings
- Age and sex
- Differential diagnosis
- Question(s) to be answered
- Required views should be mentioned
X-ray Request Form
- Name of the institution
- Name of the patient, including UR number, date of birth, gender
- Indicates if the patient is ambulant, arriving in a wheel chair or confined to a bed
- Any allergies applicable to the imaging procedure e.g. allergy to contrast media
- The name of the referring doctor, signature and date of request
- Contact details of referring doctor, in this case an internal pager number is given
- Clinical details of the patient, to enable the radiographer to perform the most beneficial views and information for the radiologist to assist with reporting
- indicates if previous imaging studies have been performed for this patient at this department, old films are an excellent source of information as they enable you to compare images over time
- What examination has been requested e.g. chest x-ray
- Where is the patient located e.g. Emergency Department
- The head of the department of the referring doctor, often for billing purposes
Example of X-ray Request Form
- wikiRadiography medical centre
- CITIZEN, JOHN 01/01/1950
-
- Private
- Compens.
- Hospital
- Non Compens.
- Ambulance
- Chair
- Bed
- Ward
- Theatre
- Abbey
- N/A
- 1/2/2008
- 1 2 3 4
- SOB O2 ?APO
- YES
- View:
- (Marked as “YES” in the image)
- CXR
- ED
- Date of Presentation
- DR ANDY C
Reading X-rays
- General information
- Reading bone
- Reading joints
- Reading soft tissues
General Information
- Identify patient’s information
- Name, sex, age, file number, date of X-ray
- Anatomical area
- What parts are seen on the film
- View(s)
- AP, Lat., Oblique, Special, …
- X-ray quality
- Extra:
- In full cast. cast slab, splint, traction pin, implants…
Reading Bone
- Bone age
- Epiphyseal plates open/closed (child Vs. adult)
- Bone Quality (Texture)
- Generalized
- Local area
- Cortex
- Medulla
- Bone Morphology
- Shape, size, deformities,
Reading Bone (Continued)
- Periosteal reaction
- Solid: Benign
- Interrupted: Aggressive
- Lamellated / Sun-burst / Codman’s triangle
- Bone growth
- Bone destruction
Reading Bone (Continued)
- Periosteal reaction
- Bone growth
- Bone destruction
Bone Destruction by Age
< 30 years
- FD
- Ewing EG
- NOF
- SBC
- CMF
- Enchond
- Osteo sarcoma
- Chondroblastoma
- Osteoid osteoma
- Osteo Chondroma
- ABC
- infection
> 30 years
- Metastasis Myeloma Lymphoma
- Metastasis Myeloma HPT
- Enchondroma Chondrosarcoma
- Giant CT
- Geode
- infection
Reading Joints
- Position
- Relations
- Alignment
- Joint “Space”
- Joint line
- Subchondral bone
Joint Position
Joint Relations
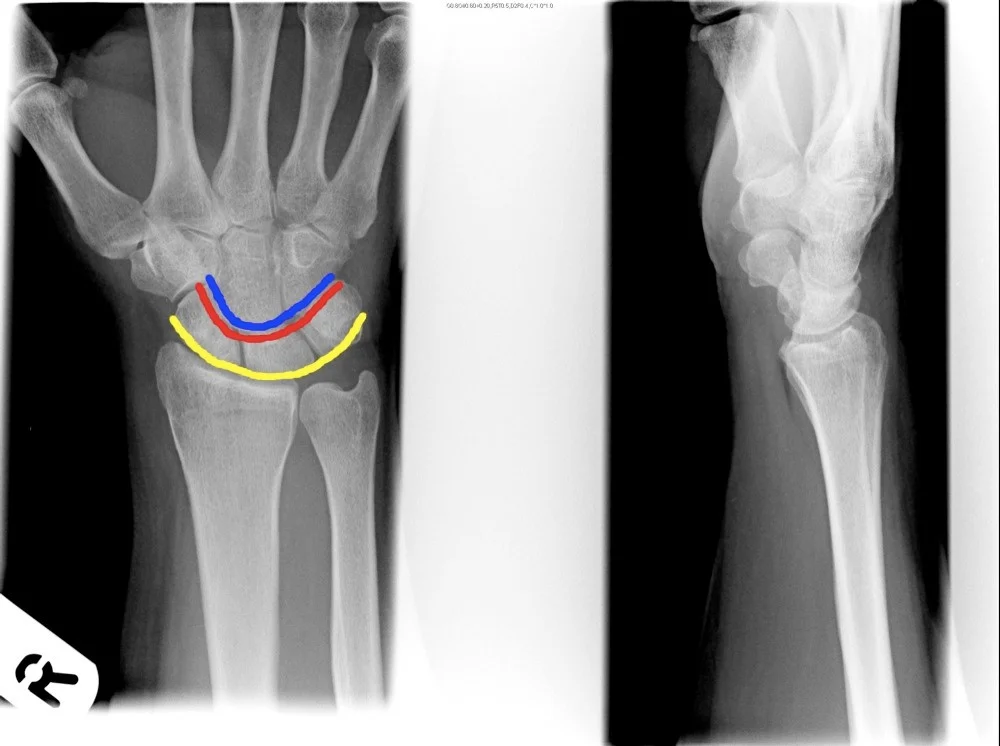
Reading Joint Anatomy
- The image presents two X-ray views of a joint, likely a knee joint, with the second image annotated to highlight specific anatomical features.
- The annotations include:
- Joint space
- Cartilage
- Meniscus
- Joint soft tissues
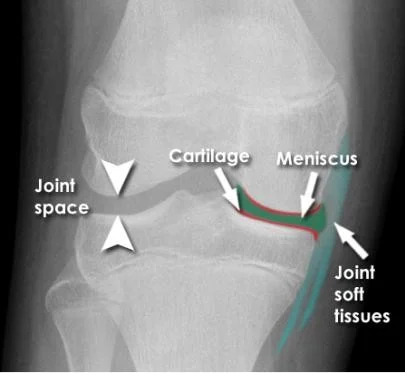
Bone and Joint Alignment
Joint Space
- The image presents two X-ray images of a joint, with the right image annotated to highlight specific features.
- The annotated image includes labels for:
- Joint narrowing
- Osteophytes
- The annotated image includes labels for:
Bone and Joint
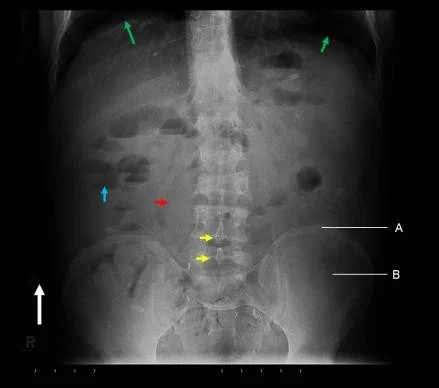
35 year old male with normal pelvis and no arthritis
- greater trochanter
- joint space
- calcar
- lesser trochanter
- femoral cortex
- acetabulum
- femoral head
- femoral canal
53 year old female with osteopenia (low bone mineral density) and no significant arthritis
- the bone in the area of the calcar is less robust
- the cortex of the femur is thinner
Elderly female with left hip osteoarthritis
- greater trochanter
- femoral head
- acetabulum
- lesser trochanter
- severely narrowed joint space (arthritis)
- femoral canal
Soft Tissue Reading
- In relation to bone cortex
- Next to bone
- e.g. fat pad
- Muscles
- Muscle planes, bulk
- Other soft tissues
- Vessels, lungs, organs, cartilage
- Calcifications, Air, Fluid, …
Look for the Unexpected
- Minor narrowing of the subacromial space (arrowheads) - suggesting rotator cuff disease - very common cause of shoulder pain
- It would be easy to consider this the only abnormality if not checking the image systematically
- Unexpected apical lung mass!
- Clinically suspected rotator cuff disease
- Pain distal to the elbow - rarely if ever caused by shoulder pathology
- Diagnosis
- Minor rotator cuff disease
- ‘Pancoast’ tumour - apical lung cancer (cause of distal pain - referred from brachial plexus)

Artifacts Obscuring Diagnosis
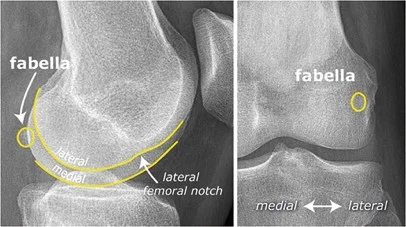
The fabella - Normal
- The image contains two X-ray images of a knee.
- The left image is labeled with:
- fabella
- lateral femoral notch
- A curved line highlighting the lateral medial area.
- The right image is labeled with:
- fabella
- medial
- lateral
- A circle around a specific area within the fabella.
- The left image is labeled with:
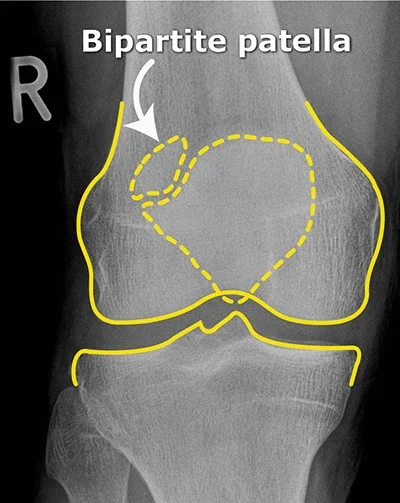
Bipartite patella - Normal
- No localized tenderness
- Superolateral
- Line not that of a fresh fracture
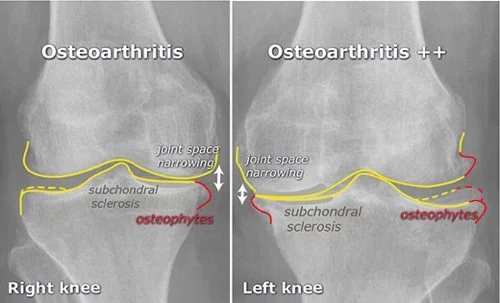
Reading Joints (Continued)
The image presents a comparative analysis of two knee X-rays, labeled as “Right knee” and “Left knee,” both diagnosed with osteoarthritis. The X-rays are accompanied by annotations highlighting specific features associated with the condition.
- Right Knee (Osteoarthritis)
- Joint Space Narrowing: Indicated by white arrows pointing upwards.
- Subchondral Sclerosis: Highlighted in gray text.
- Osteophytes: Marked in red.
- Left Knee (Osteoarthritis ++)
- Joint Space Narrowing: Also indicated by white arrows pointing upwards, similar to the right knee.
- Subchondral Sclerosis: Again highlighted in gray text.
- Osteophytes: Similarly marked in red.
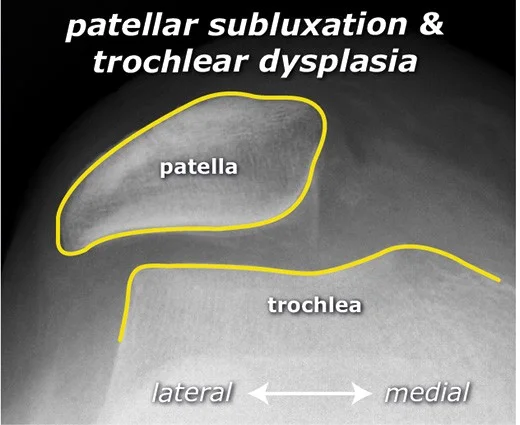
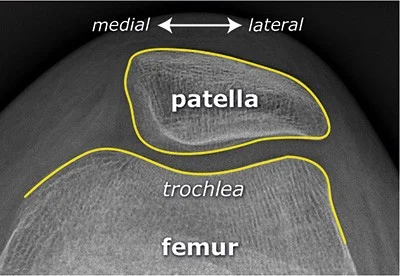
Patellar position
Normal
- X-ray image labeled with:
- medial and lateral directions
- Annotated structures:
- patella
- trochlea
- femur
patellar subluxation & trochlear dysplasia
- X-ray image labeled with:
- lateral and medial directions
- Annotated structures:
- patella
- trochlea
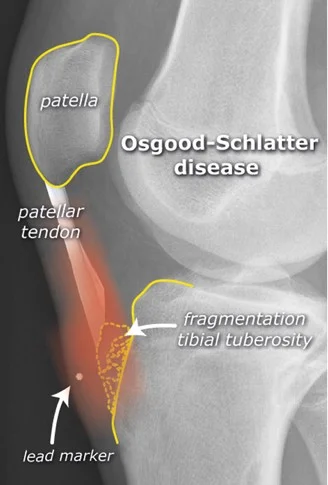
Reading Joints (Continued)
- Traction apophysitis
- Osgood Schlatter
Arthroplasty
- Total Hip Arthroplasty (THA)
- Hemiarthroplasty (HAP)

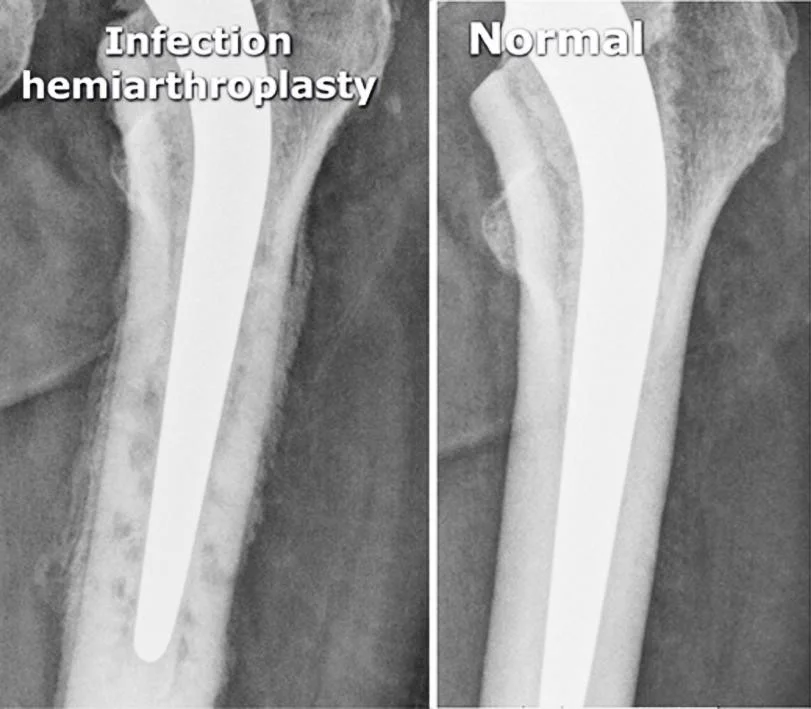
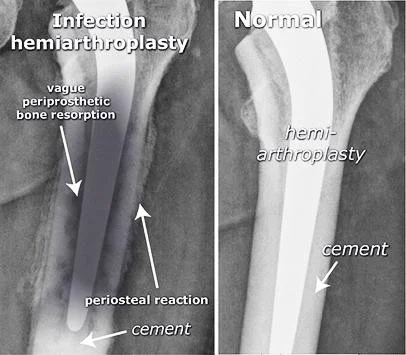
Infected arthroplasty
- Pain after arthroplasty
- Mild fever
Infection hemiarthroplasty
- vague periprosthetic bone resorption
- periosteal reaction
- cement
Normal
- hemi-arthroplasty
- cement
Reading of bone lesions
- Which bone, and which site in bone?
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-defined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
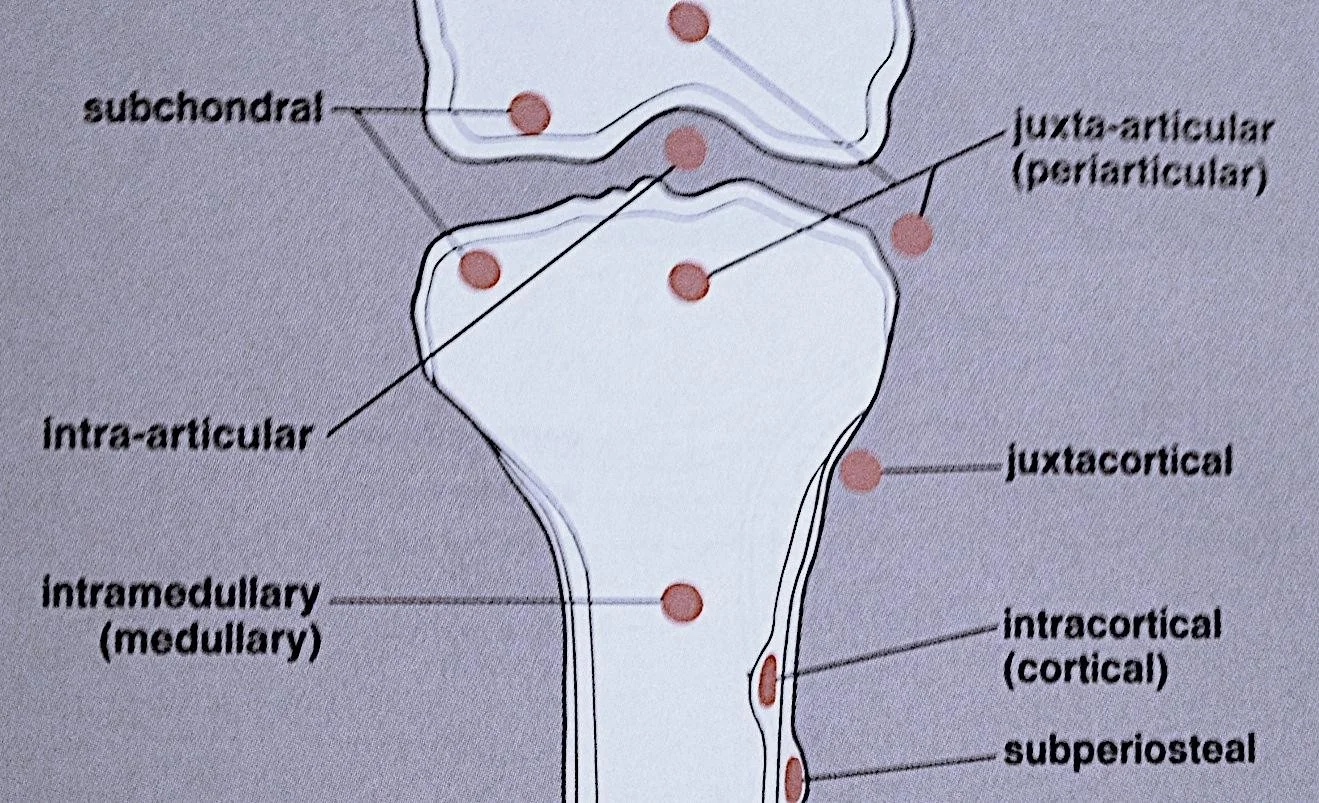
Location
- subchondral
- intra-articular
- intramedullary (medullary)
- juxta-articular (periarticular)
- juxtacortical
- intracortical (cortical)
- subperiosteal
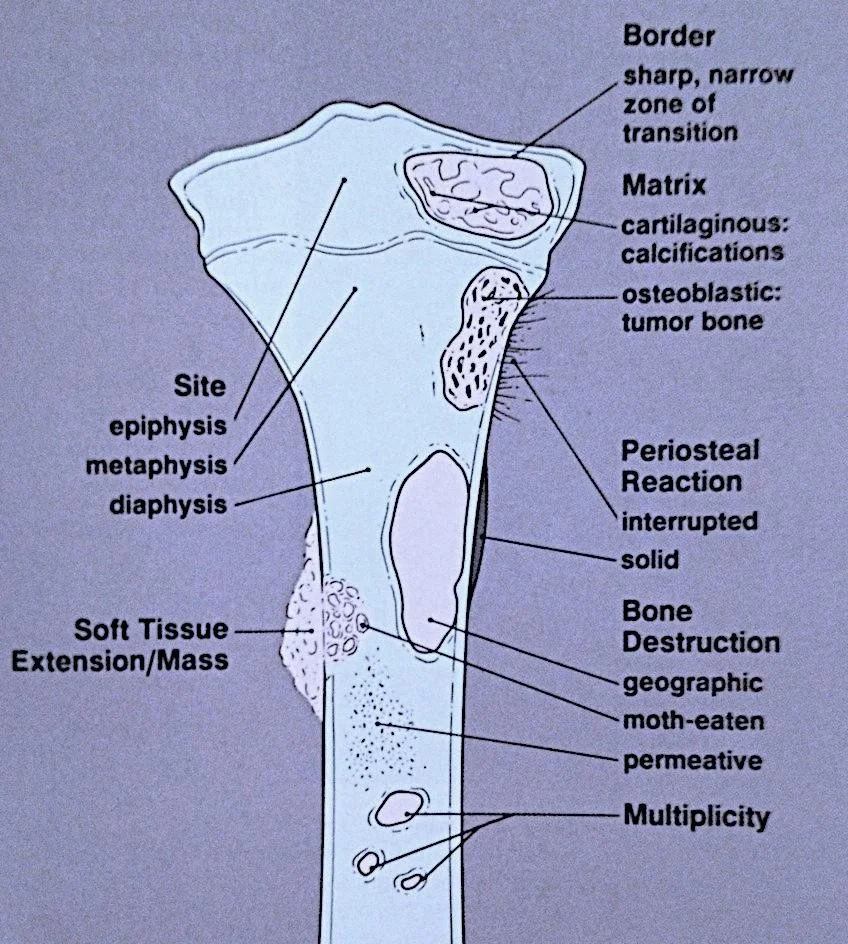
Radiographic features
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-defined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
- Border
- sharp, narrow zone of transition
- Matrix
- cartilaginous: calcifications
- osteoblastic: tumor bone
- Site
- epiphysis
- metaphysis
- diaphysis
- Periosteal Reaction
- interrupted
- solid
- Bone Destruction
- geographic
- moth-eaten
- permeative
- Multiplicity
- Soft Tissue Extension/Mass
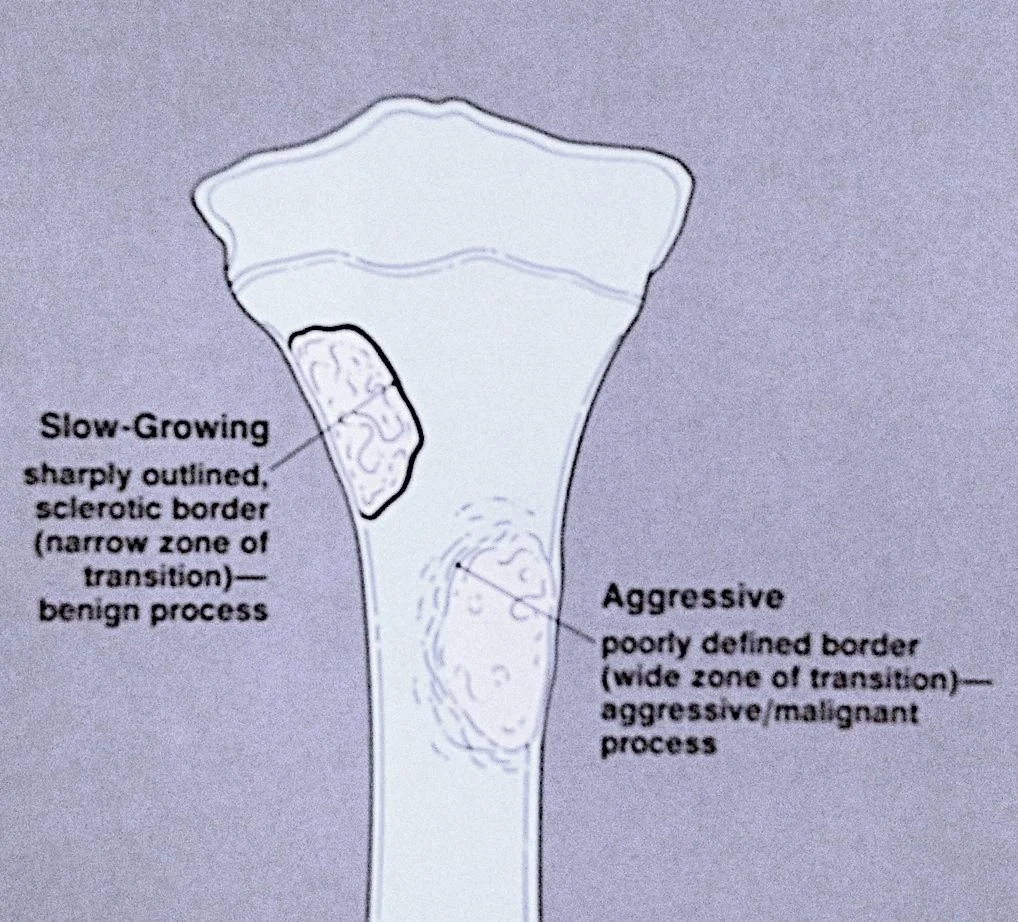
The Border
- Slow-Growing
- sharply outlined, sclerotic border (narrow zone of transition)—benign process
- Aggressive
- poorly defined border (wide zone of transition)—aggressive/malignant process
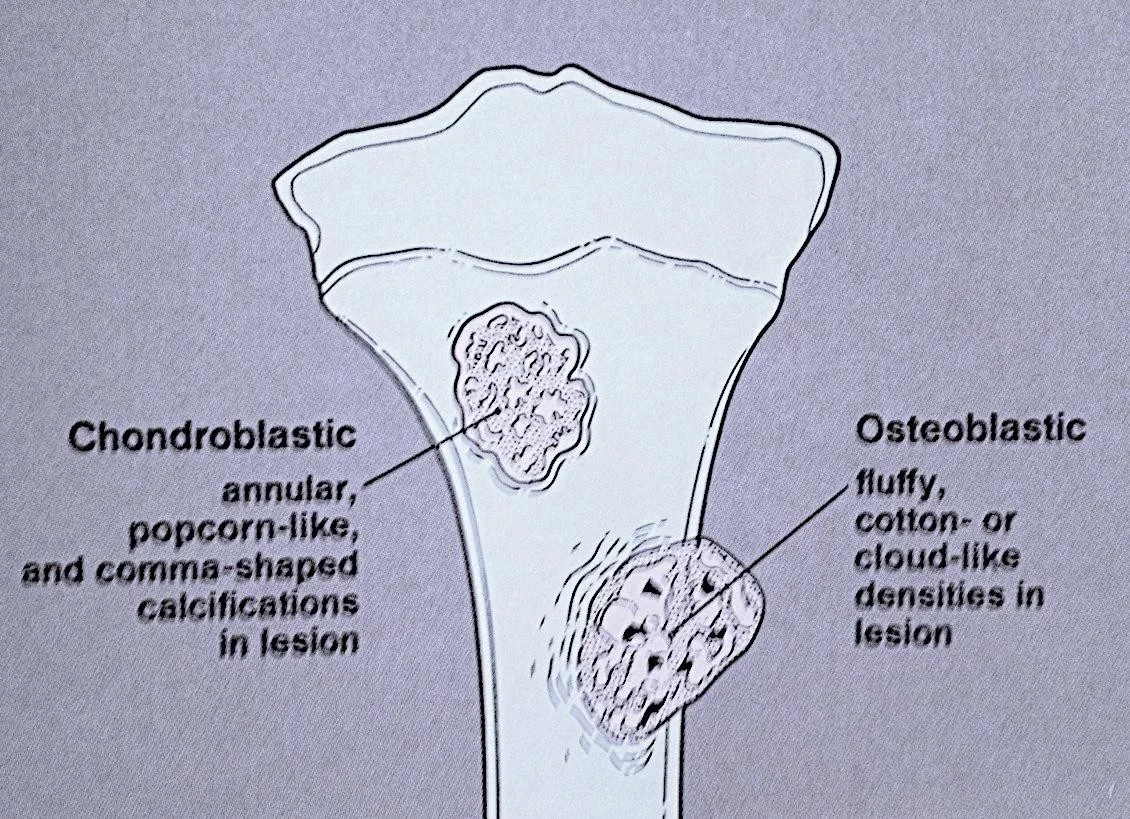
The Matrix
-
Chondroblastic
- annular, popcorn-like, and comma-shaped calcifications in lesion
-
Osteoblastic
- fluffy, cotton- or cloud-like densities in lesion
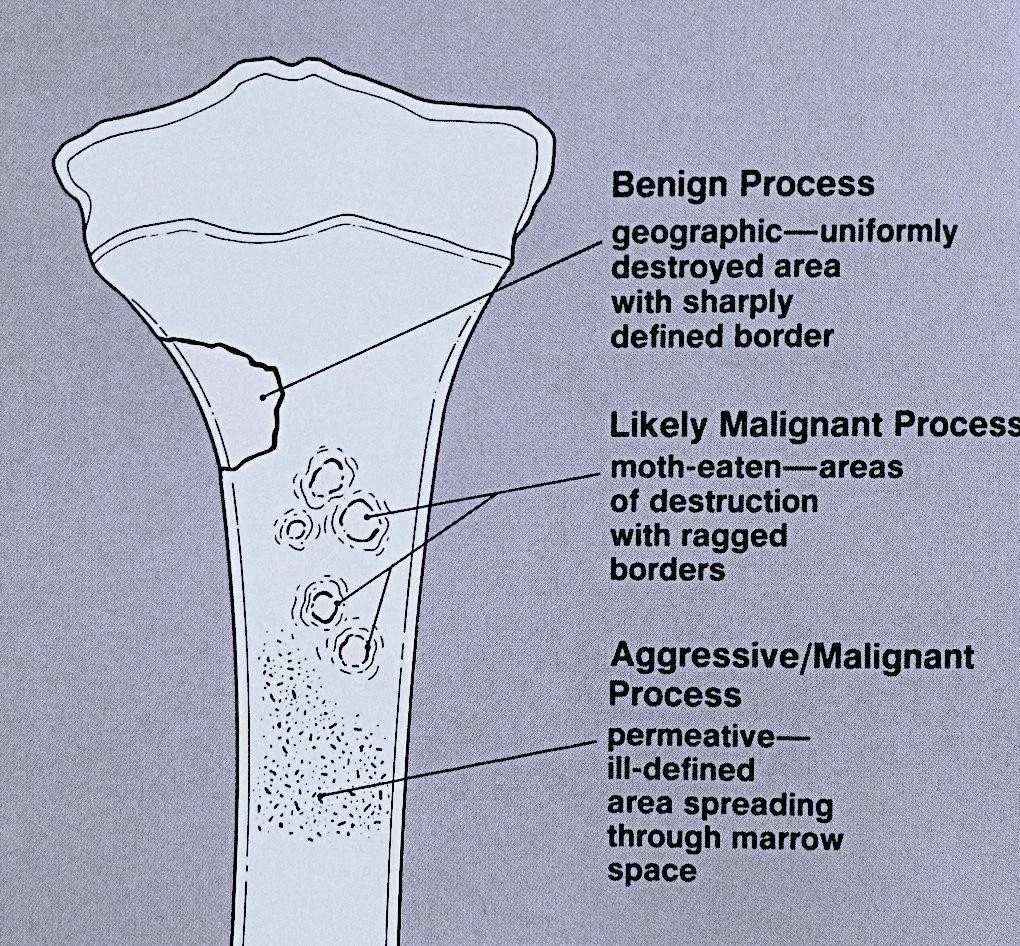
Type of Bone Destruction
-
Benign Process
- geographic—uniformly destroyed area with sharply defined border
-
Likely Malignant Process
- moth-eaten—areas of destruction with ragged borders
-
Aggressive/Malignant Process
- permeative—ill-defined area spreading through marrow space
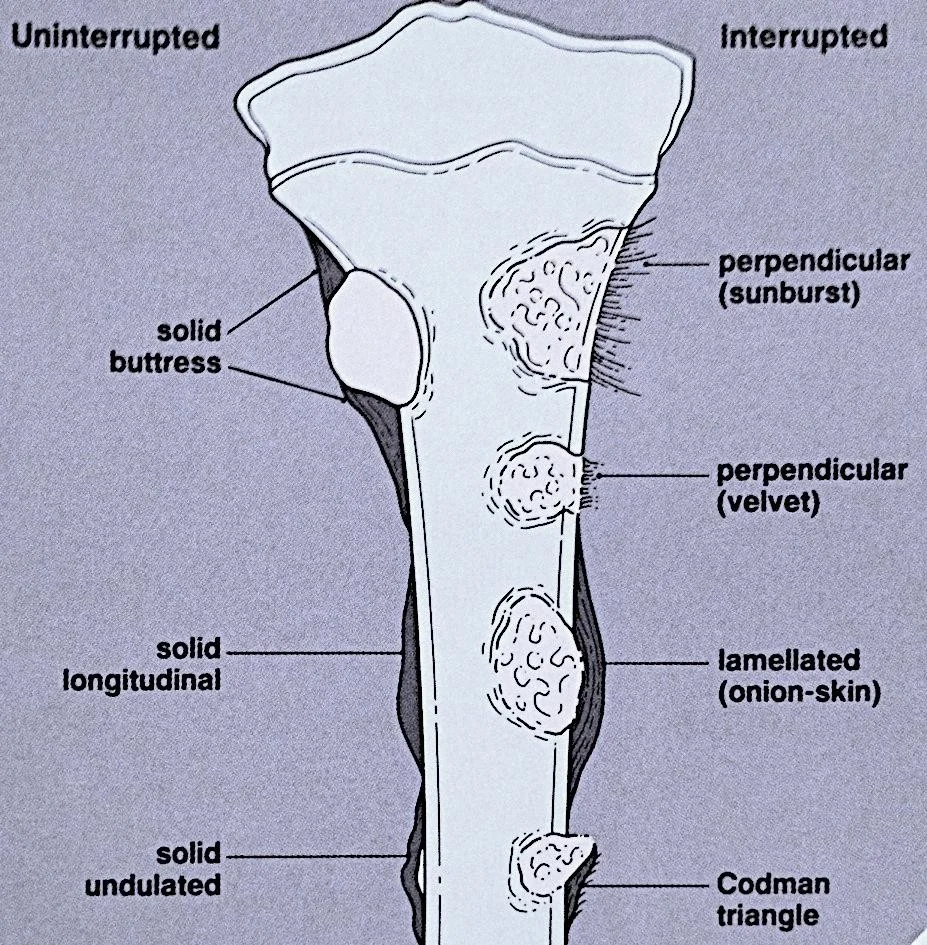
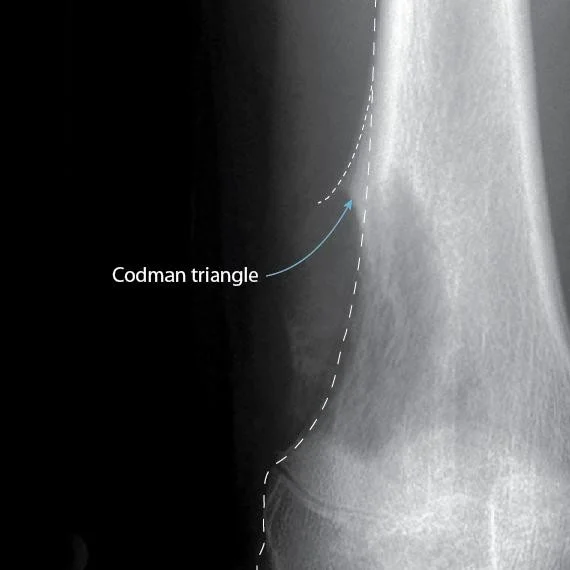
Type of Periosteal Reaction
-
Uninterrupted
- solid buttress
- solid longitudinal
- solid undulated
-
Interrupted
- perpendicular (sunburst)
- perpendicular (velvet)
- lamellated (onion-skin)
- Codman triangle
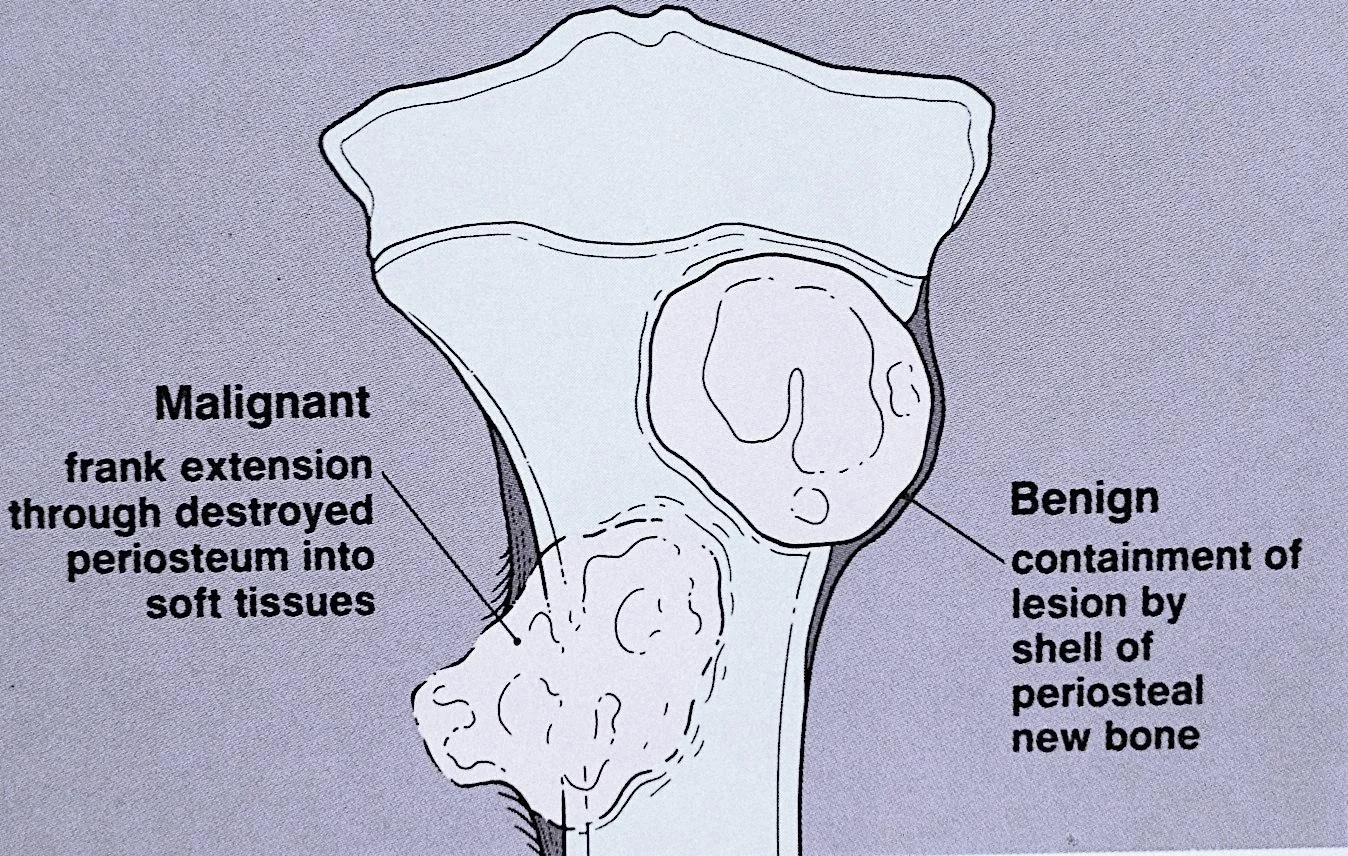
Soft Tissue Extension
-
Malignant
- frank extension through destroyed periosteum into soft tissues
-
Benign
- containment of lesion by shell of periosteal new bone
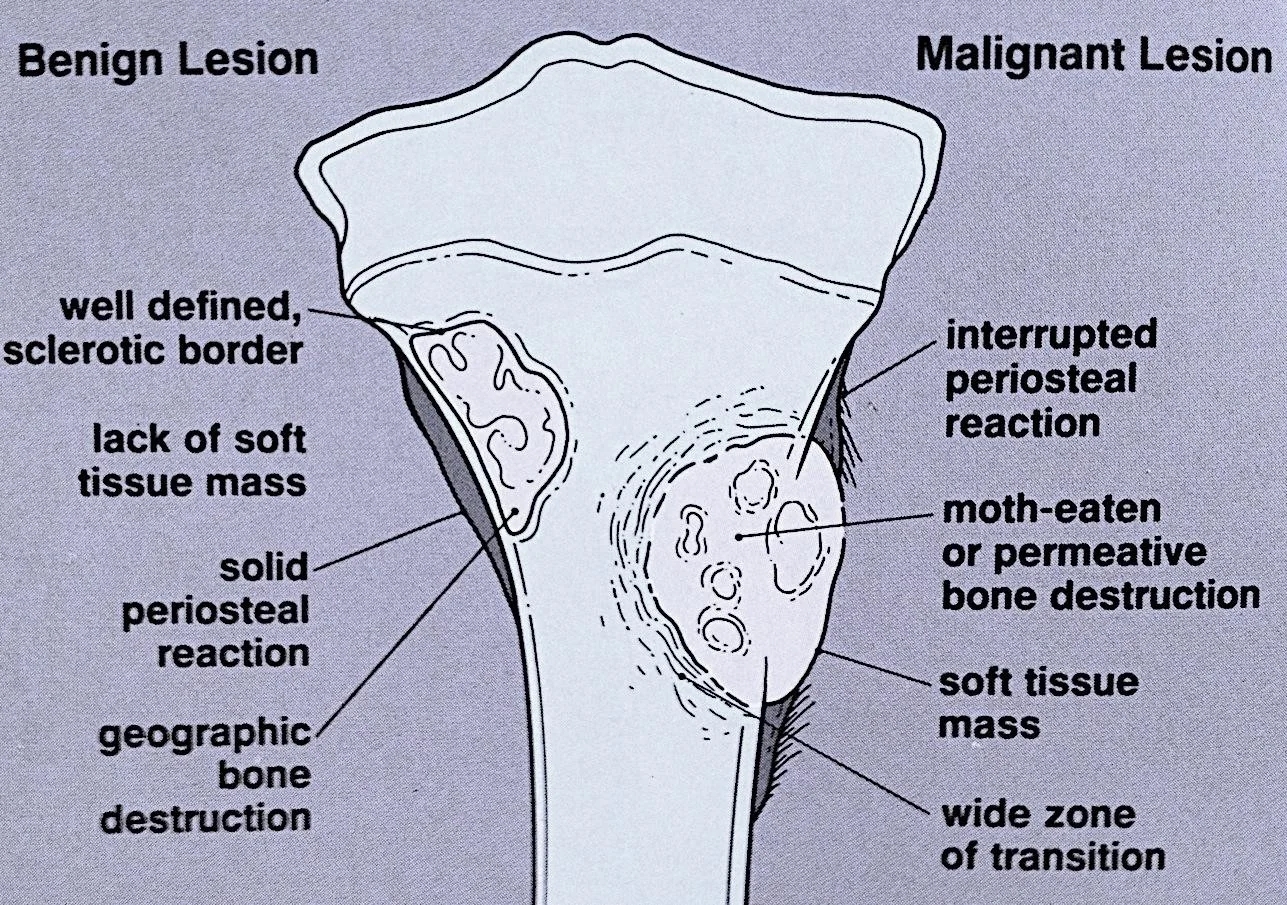
Benign Vs. malignant
Benign Lesion
- well defined, sclerotic border
- lack of soft tissue mass
- solid periosteal reaction
- geographic bone destruction
Malignant Lesion
- interrupted periosteal reaction
- moth-eaten or permeative bone destruction
- soft tissue mass
- wide zone of transition
Type of Periosteal Reaction (Continued)
The image shows an X-ray with a highlighted area indicating a Codman triangle.
- The Codman triangle is labeled in white text.
- A blue arrow points to the Codman triangle.
Type of Periosteal Reaction (Continued)
Sunburst

Bone Lesions and Imaging
Overview of Bone Lesions
Case Studies
Case 1: 45-year-old Lady with Knee Pain
- Patient Profile: 45-year-old lady with knee pain
- Initial Assessment:
- ![ [How to Read X-rays -Orthopedics-ps66-1.webp]]
- Key Observations:
- Osteopenic lesion
- Eccentric
- Clear narrow zone of transition
- Breaking through posterior cortex
- Periosteal reaction
- Further Investigation: MRI recommended
- MRI Findings: Soft tissue extension
- Diagnosis: Biopsy showed mammary carcinoma - had undiagnosed Ca Breast
Case 2: 15-year-old Boy - Asymptomatic
- Patient Profile: 15-year-old boy, asymptomatic
- Diagnosis: Simple bone cyst
- Key Features:
- Osteopenic lesion
- Uniform consistency
- Eccentric
- Clear narrow zone of transition
- Respecting cortex
- No periosteal reaction
Case 3: 12-year-old Boy with Swelling Lower Leg
- Patient Profile: 12-year-old boy with swelling lower leg
- Diagnosis: Aneurysmal bone cyst
- Key Features:
- Osteopenic lesion
- Eccentric
- Clear narrow zone of transition
- Respecting cortex
- Ballooning cortex
- No periosteal reaction
Case 4: 45-year-old with Pain R Thigh
- Patient Profile: 45-year-old with pain R thigh, swollen, tender
- Key Features:
- Osteopenic lesion
- Inside medulla
- Unclear /Wide zone of transition
- Ill-defined
- Respecting cortex
- No periosteal reaction
- Assessment: Aggressive lesion, could be Tumor / infection, Need further investigation
Case 5: 45-year-old with Pain R Thigh - Osteomyelitis
- Patient Profile: 45-year-old with pain R thigh, swollen, tender
- Key Features:
- Widely spread inside medulla
- Extends to soft tissues
- Edema in soft tissues
- Diagnosis: Osteomyelitis
- ![ [How to Read X-rays -Orthopedics-ps71-1.webp]]
Case 6: 2-year-old with Fever, Vomiting, Pain L Hip
- Patient Profile: 2-year-old with fever, vomiting, pain L hip, limited ROM
- Key Features:
- Localized osteopenic lesion upper metaphysis L femur
- Reaching epiphyseal plate
- Differential Diagnosis: ?Osteomyelitis, ?Septic arthritis
- Further Investigation:
- CBC, Diff. WBC, CRP, ESR
- Ultrasound
- MRI
Case 7: 2-year-old with Fever, Pain L Hip - Septic Arthritis
- Patient Profile: 2-year-old with fever, vomiting, pain L hip, limited ROM
- Ultrasound Findings: U/S: large hip effusion with echogenic content (Pus)
- ![ [How to Read X-rays -Orthopedics-ps73-1.webp]]
- MRI Findings: MRI: hyperintense T2, Oedema, Fluid collection outside bone, Effusion in hip joint
Case 8: 10-year-old with Pain L Hip
- Patient Profile: 10-year-old with pain L hip, no tenderness, full ROM
- Key Features:
- Osteopenic lesion
- Sclerosis in intertrochanteric area
- Further Investigation: Need CT
Case 9: 10-year-old with Pain L Hip - Osteoid Osteoma
- Patient Profile: 10-year-old with pain L hip, no tenderness, full ROM
- CT Findings:
- Osteopenic lesion with nidus
- Surrounded by sclerosis
- No periosteal reaction
- Diagnosis: Osteoid osteoma
Case 10: 17-year-old with Painful Swelling Lower Thigh
- Patient Profile: 17-year-old with painful swelling lower thigh
- Key Features:
- Osteosclerotic lesion
- Inside and outside medulla
- Unclear /Wide zone of transition
- Ill-defined
- Not respecting cortex
- Extending into soft tissue
- Periosteal reaction
- Diagnosis: Osteogenic sarcoma
Other Imaging Techniques
Overview
- Bone scan (Tc99):
- Shows the site of lesion / skip lesions / metastasis
- CT:
- Intra-osseous and extra-osseous structure and extension
- Good in deep bones (pelvis, spine)
- MRI:
- Shows:
- Soft tissue and cartilage
- Spread of lesion/tumor:
- Within bone, into joints, into soft tissue
- Relation to vessels
- Shows:
Summary of Key Points
General Guidelines
- Systematic approach:
- General information
- Reading bone
- Reading joints
- Reading soft tissue
Reading Bone Lesions
- Key Questions:
- Which bone, and which site in bone?
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-defined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
Reading Joints
- Key Aspects:
- Position
- Relations
- Alignment
- Joint “Space”
- Joint line
- Subchondral bone