History & Clinical Examination in Orthopedics
Prof. Mamoun Kremli
Dr. Tarif Al-Akhras
History Taking in Orthopedics
History taking
- Patient’s story
- Doctor/student reconstructs the history
- Open ended questions
- How do you feel now
- Leading questions
- What increases the pain?
- Can you open a door key?
- Can you comb your hair?
- Open ended questions
Orthopedics History
-
History Structure:
- Patient Demographic
- Chief Complaint
- History of Presenting Complaint
- Past medical/surgical history
- Medication history
- Family history
- Personal history and background
- Diet
- Activity
- Systemic review
-
Patient Demographic
- Name
- Age
- Occupation
- Hand Dominant
-
Chief Complaint:
- Site
- Onset
- Progression
- Management
-
History of Presenting Complaint
- Pain
- Swelling
- Deformity
- Limping
- Stiffness
- Usually related to function
- Loss (altered) function
- Caused by: stiffness / pain / deformity / instability / weakness
- Altered sensation
-
Pain
- Site
- Onset
- Character
- Radiation
- Associations
- Time course
- Exacerbating/relieving factors
- Severity
SOCRATES
-
Site:
- Referred Pain perceived at a location other than the site of the painful stimulus. this pain referred along the tissues developed from the same sclerotome -somite. e.g. Discogenic pain with no thecal or root compression radiated from L-S spine to groin, gluteal region, but not down to the knee. Hip: to the medial aspect of the thigh and knee
- Radiating pain: pain begins in one place and travels to another location along the path of a nerve. e.g. Sciatica :root pain radiated to lower limb below the knee
-
Onset:
- When did it start?
-
Was it
- Gradual or sudden? (acute – related to incident/action)
- Constant or intermittent?
-
Character:
- What is the pain like e.g.
- Sharp,
- Burning
- Tight?
- What is the pain like e.g.
-
Radiation:
- Pain perceived at the site of stimulus and radiate to another site
- Does it radiate/move anywhere?
-
Associations:
- Is there anything else associated with the pain e.g.
- Swelling
- Sweating
- Fever
- Vomiting
- Is there anything else associated with the pain e.g.
-
Time course:
- Does it follow any time pattern, how long did it last?
-
Exacerbating/relieving factors:
- Does anything make it better or worse?
-
Severity:
- How severe is the pain
- Consider using the 1-10 scale
SOCRATES
-
Stiffness
- Patients complain of loss of/altered function, not stiffness
- Can not comb hair, can not bend forward, can not sit cross-legged, can not sit in prayer, …
- Joint involved
- Cause:
- Real stiffness of joint / mechanical block
- Protective mechanism:
- Muscle spasm to avoid pain on movement of joint
- Generalized: systemic disease
- e.g. Rheumatoid Arthritis, Ankylosing spondylitis
- Localized
- To a particular joint
- Patients complain of loss of/altered function, not stiffness
-
Swelling
- Soft tissue, joint, bone
- After trauma:
- Injury or reactive
- Rapid or Slow developing
- Rapid: bleeding / Slow: effusion
- Painful vs. Painless
- Constant vs. comes and goes
- Size:
- Same, increasing, decreasing
-
Deformity
- Progressive, or improving?
- Impairing function?
- Associated with
- Pain
- Stiffness
- Other metabolic diseases
-
Functional affection:
- Relate to normal function of part
- Walking
- Bending, Praying
- Going to toilet
- Sitting cross-legged
- Eating
- Reaching,
- Holding,
- Opening,
- etc…
- Relate to normal function of part
-
Instability
- Joint “gives way” or “jumps out of place”
-
Weakness
- Generalized: part of a systemic disease
- Localized: Patients usually describe it as:
- The limb is “dead” / “heavy”
-
Associated conditions / other diseases
-
Careful about history of mild trauma
- History of mild trauma, especially in children, can be a normal daily occurrence
-
Past medical/surgical history
-
Medication & Allergy history
-
Family history
- Genetic - e.g. RA, CDH
- Communicable - e.g. TB
-
Personal history and background
- Occupation
- Travel
- Recreation
- Home condition
- Drug or Alcohol abuse
-
Diet
- Food / drinks (good and bad!)
- Sun exposure
-
Activity
-
Systemic review
- Respiratory – e.g. TB
- UTI – source of infection
- GIT – deficiency
- Renal – disease
Summary - History-taking
- Chief complaint
- Onset, Progression, Management
- Pain
- Swelling
- Deformity
- Limping
- Stiffness
- Loss (altered) function
- Altered sensation
- Detailed mechanism of injury in trauma
- High velocity Vs. Low velocity
- Open Vs. Closed
- Onset, Progression, Management
- Relate to function
Clinical Examination in Orthopedics
Clinical examination
- The examination begins from the moment we set eyes on the patient. Observe:
- General appearance
- Posture
- Gait:
- limping, in pain, using stick, …
- Deformities:
- Knock-knees? Spinal curvature? short limb? paralyzed arm?
- Pain?
- …The clues are endless

Principles of Assessment
- Proper interaction with patient
- Normal side first
- Compare to other side/joint
- Do not cause pain
- Watch facial expressions
- Extra careful with children
- Proceed slowly, do no attack!
- Play with child!
Orthopedic Examination
- Which system to use?
- Look
- Feel
- Move
- Special tests
LOOK
-
What do we look at ?
-
What do we look for ?
-
General on patient.
-
General local (shoulder, back, hip, thigh, …):
- Position
- Major deformity, swelling
- Extra: cast, splint, traction, dressing …
-
Anatomic local:
- Skin: swelling, scars, color, hair, dryness …
- Subcut.: LN, veins, nerves, tendons …
- Muscles: bulk, wasting, twitches …
- Bones: landmarks, swelling, angulation, deformity.
- Joints: position, swelling, redness…
-
General on patient
- Patient in pain, sitting on a chair holding the right wrist and hand
- Lying comfortably in bed not in pain.
- Lying supine, in pain, holding R thigh in flexion.
- Patients is restless in bed



- General on patient.
- General local (shoulder, back, hip, thigh,.. ):
- Position of joint
- Major deformity, swelling
- Extra: cast, splint, traction, dressing …etc.




- Important Considerations:
- Amount of exposure
- Duration of exposure
- Persons present during exposure
- Place of exposure
- Attitude and behavior during exposure
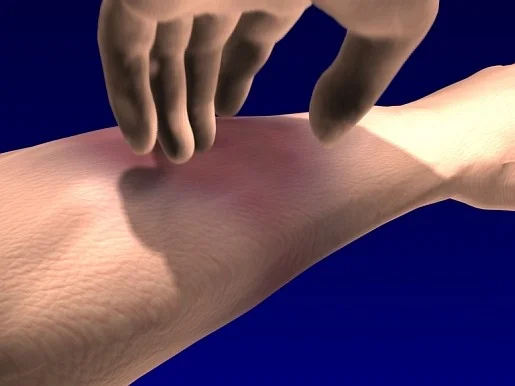
Feel
- Ask for pain or tenderness before you put your hands on the patient!
- Inform patient (take permission) you are going to touch him/her and ask to inform you if it hurts
-
What do we feel for ?
- Tenderness
- Temperature
- Anatomical
-
Tenderness:
- Generalized - Specific
-
Temperature:
- Compare distal / proximal, R / L
-
Anatomic:
- Skin: dryness, hyper/hyposthesia, scars
- Subcut.: LN, nerves, vessels, tendons, nodules
- Muscle: tone, bulk, twitches, gaps, tenderness
- Bone: landmarks, tenderness, mass, crepitus
- Joint: swelling, effusion, crepitation, synovial thickening, joint line tenderness (if joint accessible)
Move
Active Vs. Passive
- Active
- Always to start with / not to cause pain
- More used in upper limb
- A must for assessment of muscle power
- Passive
- If need to see difference from active
- In muscle weakness /neurological problems
- More used in lower limbs
- If need to see difference from active
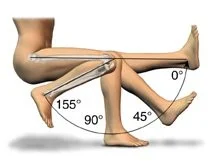
Range of Movement
- Recorded in degrees!
- Range of motion:
- Starting from resting xx degrees to xx degrees where motion stops
- Zero is the neutral or anatomical position of the joint
- Do NOT use the words:
- ‘full’, ‘good’, ‘limited’, ‘poor’
-
Examples:
- e.g, ‘knee flexion 0–140° means
- range of flexion from zero (the knee absolutely straight) through an arc of 140°
- e.g, ‘knee flexion 20–90° means
- flexion begins at 20° (i.e. the joint cannot extend fully) and continues only to 90°
- e.g, ‘knee flexion 0–140° means
-
Assess painful arc, if present
- e.g. Shoulder painful abduction
- At initial abduction
- In mid-abduction
- At extreme of abduction
- e.g. Shoulder painful abduction
-
Painful range of motion
- e.g. Knee flexion from zero to 90°, with pain from 90° to 110° then could not flex more because of pain
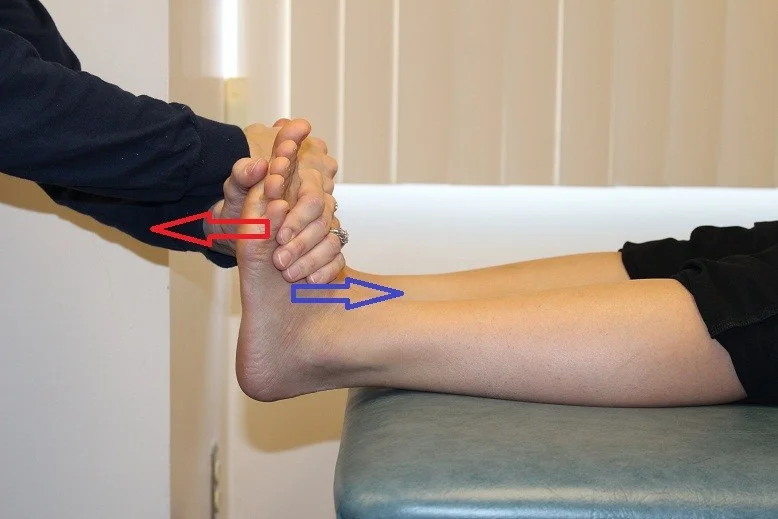
Special Tests
-
Different for different joints
- e.g. Anterior Drawer Test for ACL tear in Knee
- e.g. Patellar Tap for knee effusion
- e.g. Thomas Test for fixed flexion deformity of Hip
-
Weight-bearing / gait
- Examination of all weight-bearing joints is not complete until weight-bearing is assessed!

Bony Lumps
- Size
- Site
- Margin
- Consistency
- Tenderness
- Multiplicity
Motor Power Grading
- 0 = No power
- I = fasciculation of muscle fibers - no movement
- II = move with gravity eliminated
- III = move against gravity
- IV = less than full power
- V = full power - normal
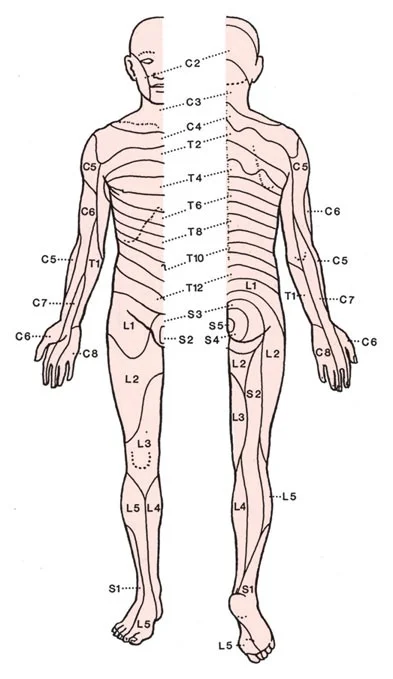
Nerve Roots LL
- Hip
- Flexion: L1,2,3
- Extension: L5, S1
- Knee
- Extension: L3,4
- Flexion: L5, S1
- Ankle
- Dorsiflexion: L4,5
- Plantarflexion: S1,2
- Inversion: L4,5
- Eversion: L5,S1
- Toe
- Extension: L5
- Flexion: S1
- Abduction: S1,2
Nerve Roots UL
-
Deltoid: C5,6
-
Supra/Infraspinatus: C5,6
-
Serratus anterior: C5,6,7
-
Elbow
- Flexion: C5,6
- Extension: C7
-
Supination: C5,6
-
Pronation: C6
-
Wrist
- Extension:C6
- Flexion: C7
-
Finger
-
Extension: C7
-
Flexion: C7,8, T1
-
Abd/Adduction: C8, T1
-
Sensation
- Dermatomes:
Trauma – Clinical Exam
-
General medical condition
- Should be evaluated to exclude
- Shock
- Brain injury
- Other problems
- Should be evaluated to exclude
-
Vital signs
- Should be observed and followed up
- Head/neck, Chest

Trauma – Clinical Exam
- Look:
- Adequate exposure
- General on patient
- Local:
- Swelling, deformity, bruises, color, …
- Special attention is to be paid to wounds
- Do not forget the back!
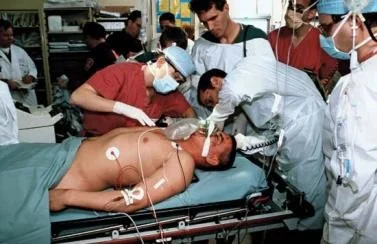

Trauma – Clinical Exam
-
Feel:
- Tenderness, temperature and crepitus on movement
- Sensory and motor deficits
- Pulse distal to injury
- Compartment syndrome
-
Move:
- With care
- Make sure not to cause more pain or injury
- Crepitus & abnormal movement indicates a fracture
- Joints distal to the affected area
- With care
Trauma – Clinical Exam
- Examination of the viscera
- Liver and spleen in rib fractures
- Urinary bladder and urethra in pelvic fractures
- Neurological examination in head and spinal injury
Summary
- Examination:
- Look
- General on patient, general local, anatomical
- Feel
- Tenderness, temperature, anatomical
- Move
- Passive, active - differs from joint to another
- Special tests
- Differ from joint to another
- Look