Cesarean Section
History
- According to legend, Julius Caesar was born by this operation and hence the origin of the term caesarean. ???
- Most important modification was the lower segment transverse incision. First done by Kehrer and popularized by Munro Kerr

Definitions
- Cesarean delivery is defined as the delivery of a fetus through surgical incisions made through the abdominal wall (laparotomy) and the uterine wall
- Hysterotomy, the surgical removal of the uterine contents (either viable or non-viable fetus), may be used during the second trimester or later (lower uterine segment not well formed). It can be performed for various reasons including preterm caesarean section, fetal surgery, delayed abortion.
Indications
Fetal Indications
- Nonreassuring FHT
- (malpresentation/malposition)
- Fetal anomalies, such as hydrocephalus, that would make successful vaginal delivery unlikely
- Umbilical cord prolapse
- Conjoined twins
Maternal Indications
- Obstruction of the lower genital tract (e.g., large condyloma)
- Previous cesarean section (if vaginal birth after cesarean [VBAC] is declined by patient or not appropriate)
- Previous uterine surgery involving the contractile portion of the uterus (i.e., classical cesarean, transmural myomectomy)
- failed forceps or vacuum/failed induction
- History of severe pelvic floor injury from a prior vaginal delivery
- Abdominal cerclage
- Medical disorders e.g., -preeclampsia and eclampsia, coarctation of aorta
Maternal and Fetal Indications
- Abruptio placentae
- Active maternal herpes simplex virus infection
- Labor dystocia (slow or Failure to progress) or cephalopelvic disproportion
- Placenta previa or known vasa previa (absolute indication)
Types of Cesarean Section
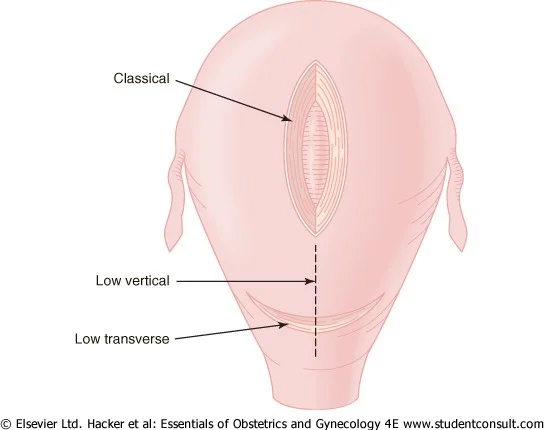
- Lower Segment Caesarean Section (LSCS):
- Most commonly type
- Lower segment vertical incision
- Classical CS
- Caesarean hysterectomy
Classical Caesarean Section
- Classical Caesarean section: Uterine incision – on the anterior uterine wall in the upper segment.
Indications: rarely performed:
- Lower segment is unapproachable due to severe adhesions or myomas
- Ca cervix
- Some cases of anterior placenta praevia with a previous caesarean
- Some cases of transverse lie (back down)
- Conjoined twins
- Post-mortem C-Section
- Poorly developed lower uterine segment (e.g., extremely preterm breech presentation)
Disadvantages
- Chance of scar rupture more
- General peritonitis, if infection occurs
Caesarean Hysterectomy
- Life-saving measure
Indications:
- Severe atonic PPH
- Placenta accreta, increta, percreta
- Severe sepsis
- Multiple large myomas
- Carcinoma in situ of the cervix
Anesthesia in C-Section
-
Anesthesia for c-section
- G.A
- Spinal
- Epidural
-
Antibiotic prophylaxis: should be given 1 hour before skin incision (single dose of cefazoline)
Complications of C-Section
Complications of Anesthesia
Complications of Operation
Maternal
-
Intraoperative
- hemorrhage, visceral injuries and infection
-
Immediate post-operative
- chest infection. Urinary retention, UTI. wound infection
-
Remote
- Rupture of scar in next pregnancy, adhesions, Gut obstruction from adhesion formation (specially repeated), Incisional hernia
Fetal
- Risks of anesthesia/Iatrogenic prematurity of baby
Reducing C-Section RateZ
- External cephalic version (ECV) SUCCESS RATE 60%
- Vaginal birth after c-section (VBAC) SUCCESS RATE 70%
Vaginal Birth After Cesarean Section (VBAC)
-
Provided there are no contraindications to vaginal delivery, a patient may be counseled and offered a trial of labor after previous cesarean delivery (TOLAC).
-
Success rates of VBAC are higher for patients with nonrecurring conditions, such as malpresentation or fetal distress in labor (60% to 85%), than for those with a prior diagnosis of dystocia (15% to 30%).Z
-
Patients should be counseled regarding the risk of uterine rupture (0.9% to 3.7%), failed trial of labor, and need for cesarean delivery.
-
Contraindications include
- previous classical or inverted T-shaped uterine incision
- transfundal uterine surgery
- history of uterine rupture, contracted pelvis
- medical or obstetric contraindications to vaginal delivery (e.g., transverse lie, PP).
Additional Considerations for VBAC
-
Induction of labor is not contraindicated.
-
A clear recommendation for or against prostaglandin E2 for labor induction is difficult to make because of limited data (to use it or not depend on your hospital policy).
-
Someone with a history of two prior C-sections may consider a TOLAC, depending on prior indications, although some providers may choose not to offer it.
-
Macrosomia should not be considered a contraindication to TOLAC.
-
Patients with twin gestations and one previous cesarean delivery are candidates for TOLAC. - sometimes
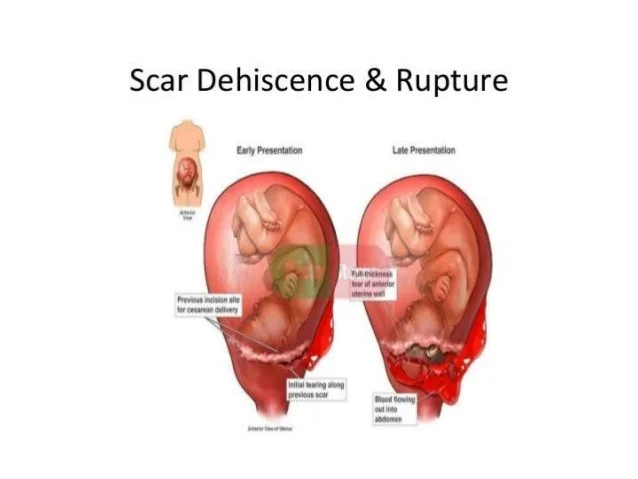
Uterine Dehiscence or Rupture
-
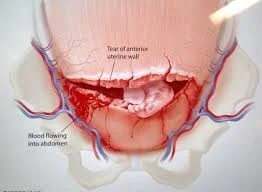
Dehiscence is defined as lower uterine scar separation that does not breach the serosa; it rarely causes significant bleeding.
-
Rupture is defined as complete separation of the uterine wall and may lead to fetal distress and significant maternal hemorrhage.
-
Incidence:
- 0.2% to 1.8% of patients with one or more previous low-segment transverse cesarean sections
- 4% to 9% of patients with a prior uterine active segment incision (classical cesarean or T-incision).
Scar Dehiscence & Rupture
Diagnosis and Management of Uterine Rupture
-
Fetal bradycardia is clinically manifested in 33% to 70% of cases. Fetal distress may be the initial and common presentation in uterine rupture.
-
In more subtle cases, the initial presentation may be a simple rise in fetal station.
-
Maternal signs and symptoms include hypotension, tachycardia vaginal bleeding, uterine tenderness, a change in uterine shape, or constant abdominal pain
-
When uterine rupture is suspected, it is important to proceed emergently to laparotomy with delivery of the infant and repair of the uterine rupture.
-
Rates of recurrent rupture in subsequent pregnancies carried to term approach 22%. Recommendations are for early delivery via cesarean section by 36 weeks.

C VID
External Cephalic Version (ECV)
- At 36-37 weeks.
- Make sure that there is no fetal anomaly and the placenta is not low lying and liquor is adequate.
- By doing US (or revising anomaly scar)
- Then do the procedure under ultrasound guidance and after giving tocolytics (to relax the uterus).
- Hold the head by one hand and buttocks by other hand then turn the baby gently
- Procedure can be done with or without assistant
- ECV is considered for:
- Breech position
- Transverse lie
- Head-down position
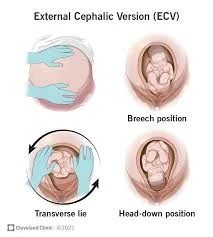
complications failure, fetal distress, abprutptio,