CNS
History
Stroke any neurological loss, slurred speech, loss of function sensory or motor, neck stiffness etc… sudden or gradual?
Components; •Medications and allergies - past and current medications
e.g anti-convulsants, OC, steroids, anti-hypertensives, anti-coagulants
- Presenting complaint
- One or several? Useful to list.
- Allow uninterrupted narrative, so far as possible
Clarify
- Date of onset CNS
- Frequency of recurrence
- Duration of episodes
- Evolution
- Nature of main symptom, in detail
- Tempo
- Associated features
- Triggers
- Exacerbating/relieving factors CNS; Conditions which exacerbate and remit
- Treatments;
- Patients may have taken drugs or other forms of therapy
- Such drugs may not have been taken properly
- adverse effects by themselves
- worsened or alleviated the symptoms
- no effect whatsoever except
HOPI
Symptoms are analyzed in relation to each other (further clarification of each symptom) and chronologically.
Onset: Sudden ,acute or gradual.
- (acute, subacute, chronic, insidious)
Duration
Course:
- Progressive
- Stationary
- Regressive
- Fluctuating
- Response to Tx
Associated symptoms
such as pain, Headaches, nausea, vomiting, vertigo, numbness, weakness, and seizures
| Aspect | Pain should be defined |
|---|---|
| Site | Where is the pain? Or the maximal site of the pain |
| Onset | When did the pain start, and was it sudden or gradual? Include also whether it is progressive or regressive. |
| Character | What is the pain like? An ache Stabbing |
| Radiation | Does the pain radiate anywhere? |
| Association | Any other signs or symptoms associated with the pain |
| Time Course | Does the pain follow any pattern? |
| Exacerbating Relieving Factors | Does anything change the pain? |
| Severity | How bad is the pain? |
Stroke
Common presenting complaints – Weakness on one side of the body. Facial deviation or asymmetry. Loss of consciousness.
History of presenting illness –
- Start ((as my patient was apparently asymptomatic _ days back when he developed weakness on one side of the body.))
- The weakness was acute/insidious in onset and gradually progressive/static in nature.
- Activity Pt was involved in at the time when this weakness developed.
- PT fell down and hurt themselves as the attack occurred.
- What limb(s) or muscles affected; affected equally or not?
- First time or a previous similar condition had occurred.
Examination - order
- General Appearance; posture, motor activity, vital signs and perhaps meningeal signs if indicated.
- higher mental status - Mini Mental Status Exam, including speech observation.
- Cranial Nerves (CN 1-12)
- Motor (bulk; muscle atrophy, fasciculation, tone, power)
- Sensory; Proprioception; *Cotton - close eyes both sides compare *
- superficial; touch, pinprick, pressure, temprature
- Deep: position sense, vibration sense,
- cortical sensation: Stereognosis, graphesthesia
- Reflexes
- Cerebellar; coordination; rapid alternating movement - finger nose test, bradykinesia; gait
- Signs of meningeal irritation
Meningitis S/S (any of the following may be present)
-
Headache (may be more severe when lying down)
-
Fevers
-
Nausea and vomiting
-
Stiff, painful neck
-
Malaise
-
Photophobia
-
Alteration in mental status (confusion, lethargy, even coma)
-
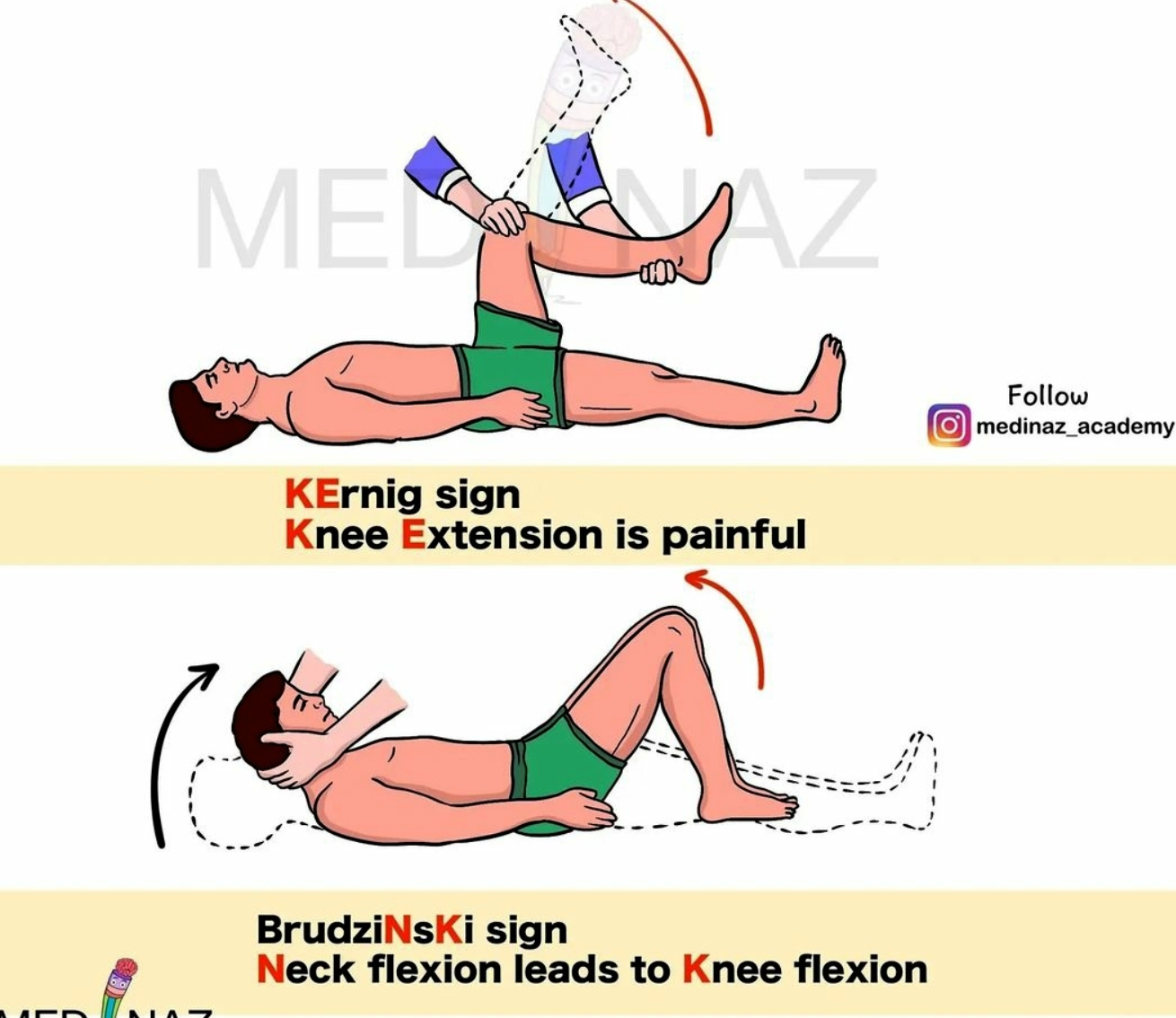
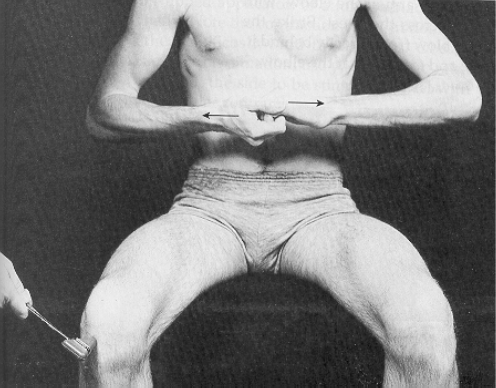
Kernig sign—inability to fully extend knees when patient is supine with hips flexed (90 degrees) caused by irritation of the meninges. Only present in approximately half of patients with bacterial meningitis
-
Brudzinski sign—flexion of legs and thighs that is brought on by passive flexion of neck for same reason as above; also present in only half of patients with bacterial meningitis
-
Jolt test—worsening headache when patient is asked to turn head back and forth quickly at frequency of at least 3 turns per second. Most sensitive and specific for acute bacterial meningitis.
1) General Appearance
The patient appears alert, well-groomed, and oriented to person, place, and time. No signs of acute distress are noted. Posture is upright, and gait is steady without any assistive devices. The patient maintains appropriate eye contact and follows commands without difficulty. There are no involuntary movements, tremors, or abnormal posturing observed. Speech is clear, coherent, and fluent, with normal rate and rhythm. Mood and affect are appropriate to the situation. No obvious signs of pain or discomfort are present during the examination.
2) Higher mental status
Alertness
Level of Consciousness (GCS)
Orientation
Person, Place, Time, & Situation
Appearance & Behavior
Cognitive function
- Attention
- Perception
-Illusions = misinterpretations of real external stimuli
-Hallucinations = subjective sensory perceptions in the absence of stimuli
Memory
- Immediate, Short-term & long-term
Speech
- Rate & rhythm
- Spontaneity
- Fluency
- Simple vs. complex
Cognitive = content, sequence, logic, coherence, and relevance
Attention = ability to focus or concentrate (over time) on one task or activity; “serial 7’s
Varies with the patient’s age
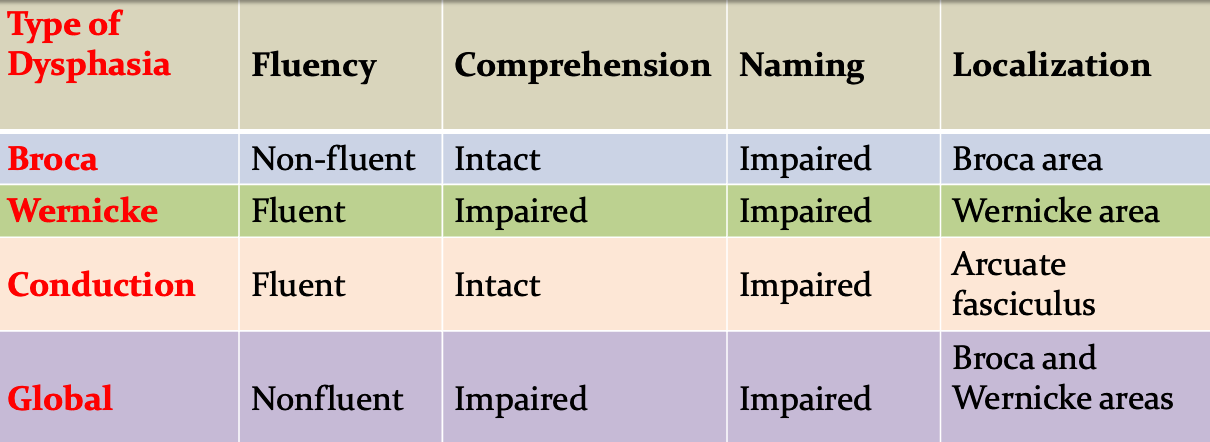
Essential Features of Common Dysphasias
Scores
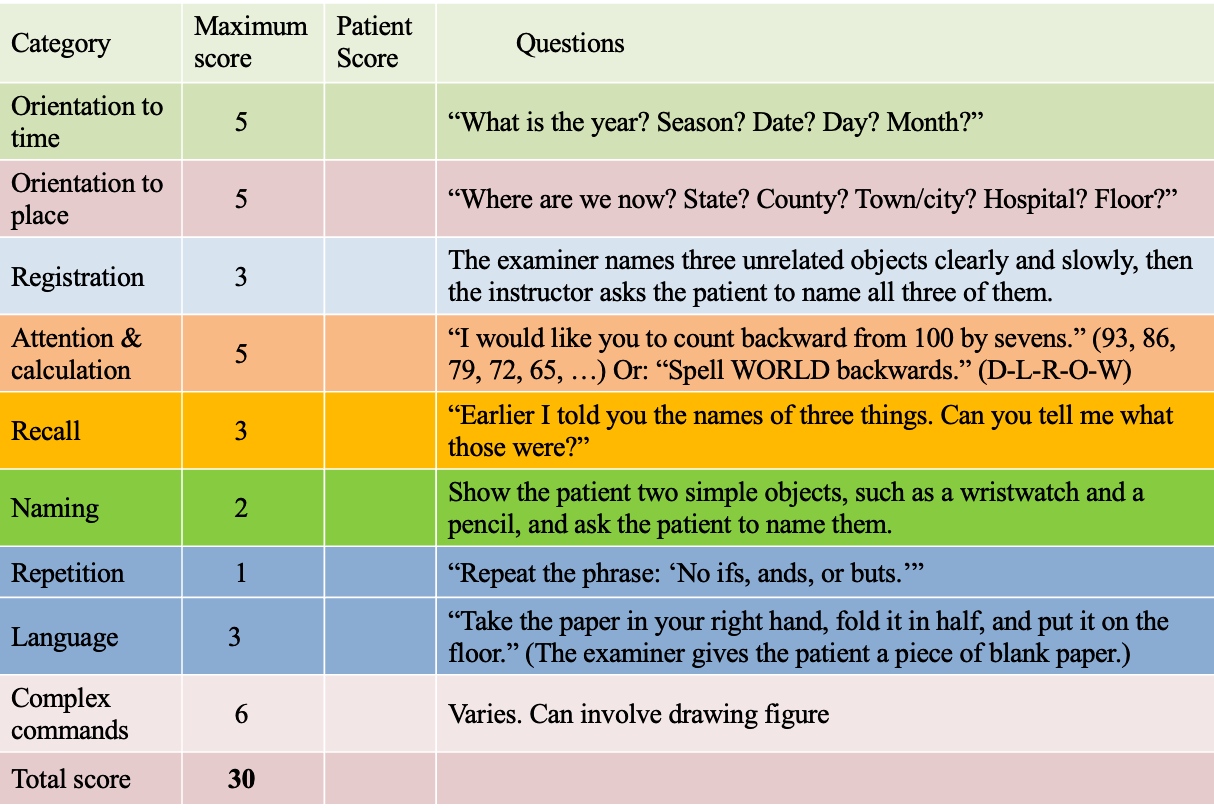
A) Mini–mental state examination
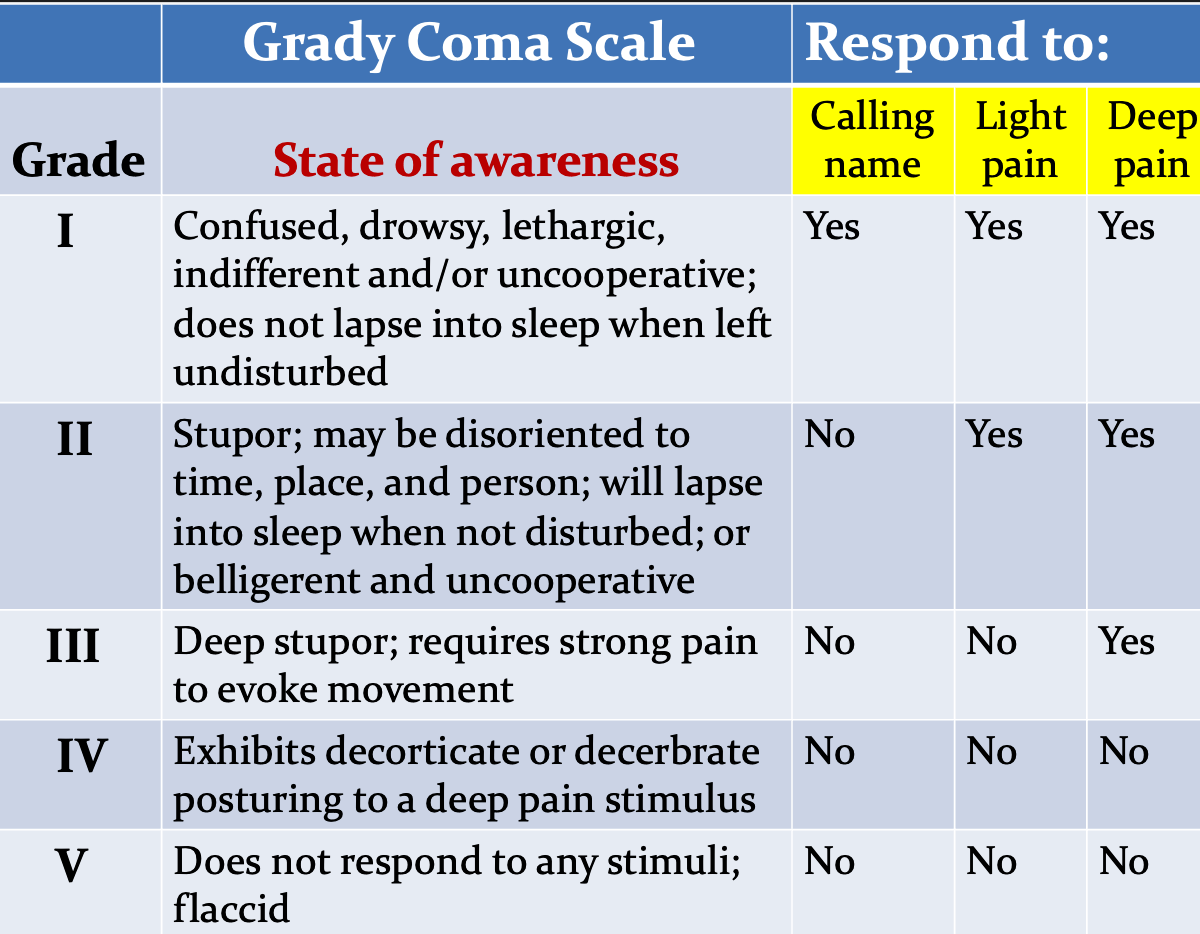
B) Grady Coma Scale
C) Glasgow Coma Scale (GCC) - Assessing LOC
Assesses patient’s neurological condition
Three Categories:
- Eye opening
- Best motor response
- Best verbal response
Score Value range 3 -15
- 3 totally comatose patient - lowest worst possible score
- Score <8 Indicates coma
- 9-12 Moderate altered level of conscious
3) CN examination
Simplified
①: Anosmia
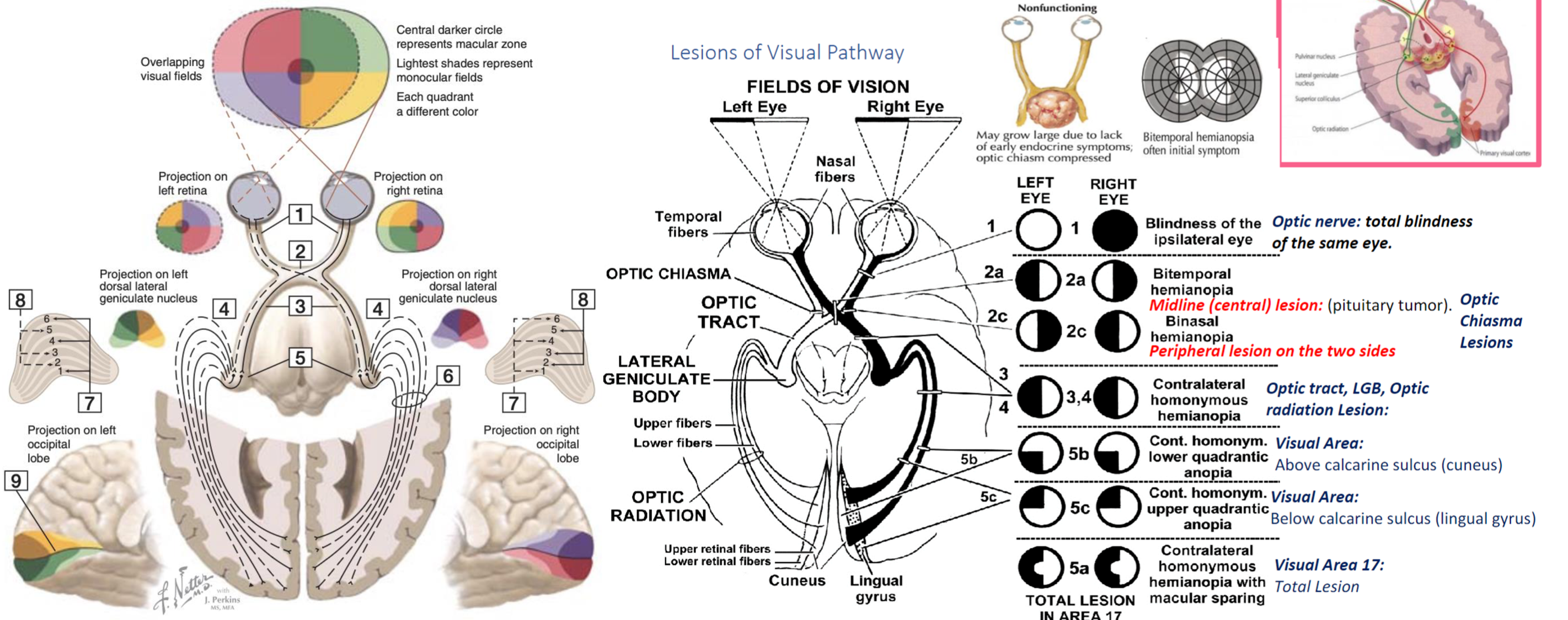
②: Acuity, Field, Color
③,④,⑥: Diplopia, Ptosis, Squint
⑤: Sensory, Pain, Temp, Motor, Masticatication, jaw reflex
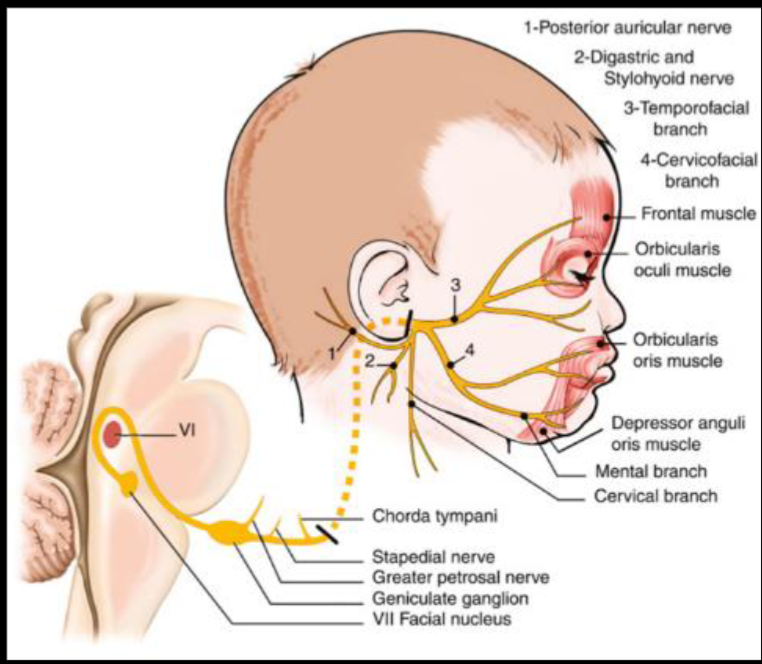
⑦: Sensory; Tast ant ⅔, sound sensitivity | Motor; Eye clos, Mouth close, blow, whistle, smile
⑧: Deaf, Tinnitus, Vertigo
⑨, ⑩: Dysph (phar), N. regur (palat), N. tone (palat), Hoarsn (lary)
⑪: Shoulder elev, neck side mov
⑫: Tongue movement
- The Olfactory Nerve CN I
- Optic Nerve CN II
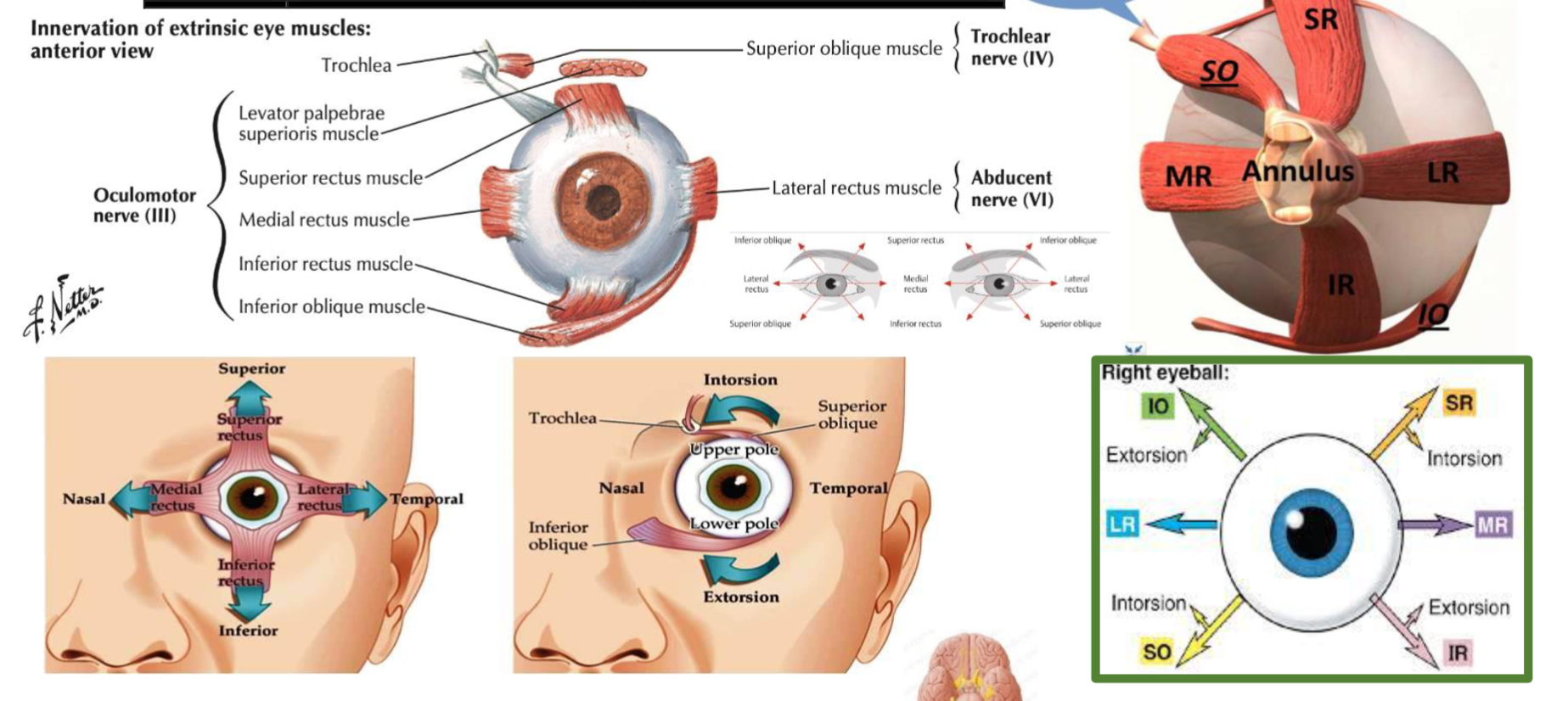
- , 4, 6 Oculomotor, Trochlear, Abducens- CN III, IV, VI; H test
- Trigeminal Nerve CN V; light touch sensation, Clench teeth - observe masseter/Temporalis, Jaw Jerk
- Facial Nerve; Keep eyes closed against resistance, blow cheeks, show teeth
- Vestibulocochlear Nerve CR VIII Tuning test Rinne’s test; mastoid/ear & Webers test; forehead
- Glossopharyngeal Nerve CR IX Test gag reflex
- Vagus Nerve CR X Uvula Deviation
- Accessory Nerve CR XI Shrug shoulders, turn head against resistance
- Hypoglossal Nerve CR XII (same side) same as .. Tongue deviation
Cranial Nerves
CN I - Olfactory;
Smell test, close one nostril, test the other. Disease that effect it: - COVID 19, Cold, flu - Meningioma - Truama - Surgery - Frontal Lobotomy - Congenital - Kallman’s syndrome -FSH LG = Hypogonad, anosmia
CN II - Optic Nerve
Disease that effect it: - Multiple Sclerosis - Diabetes - Pituitary Tumor
Examination - Visual acuity - (snellen chart) - 6 meters, if negative, test with numbers of fingers, then movement of hand, then light stimulation otherwise the patient is light blind. - Ischehara test - Color blindness related conditions; (X-Linked, Digoxin or anti-tuberculosis; Ethambutol) - Visual Field - Confrontation test - stay in same level to the patient, test one eye, close the other same as you - let the patient stare at your eyes without any movement. pull your finger towards center to confirm first sight with finger shaking, use your visual field as reference point. - testing temporal outer and nasal from central
Its important to know diseases related to the damaged lesion; Aforementioned in this graph
Other Tests includes
Indirect Light Reflex Testing:
- Use a dim torch as a light source rather than a phone to avoid excessive brightness.
- optic nerve, following its pathway to the midbrain and the Edinger-Westphal nucleus, which relays information to the oculomotor nerve, resulting in pupillary constriction.
Accommodation Reflex:
- Observes pupillary constriction when focusing on an object moving from a far to a near distance, assessing the accommodation ability of the eye.
Funduscopy:
- For a direct examination of the patient’s fundus, align your eye with to the patient’s right eye - your left arm on left shoulder of patient.
- Close your own opposite eye to avoid distraction and move closer progressively until you identify the yellow optic disc area surrounded by blood vessels.
- During this examination, observe the light reflex, which can provide additional information on the reflective properties and health of the optic nerve and retina.
CN III, IV, VI -
Superior orbital fissure Signs: - H test switch fingers at middle - to test otherwise
Occulomotor nerve palsy: - SLE , - Diabetes, - Tumor from outside emergency for surgery - if no papillary reflexes - cavernous sinus thrombosis
| Muscle | Innervation | Action |
|---|---|---|
| Superior Rectus | Oculomotor nerve (CN III) | Elevates, adducts, and medially rotates the eyeball |
| Inferior Rectus | Oculomotor nerve (CN III) | Depresses, adducts, and laterally rotates the eyeball |
| Medial Rectus | Oculomotor nerve (CN III) | Adducts the eyeball |
| Lateral Rectus | Abducens nerve (CN VI) | Abducts the eyeball |
| Superior Oblique | Trochlear nerve (CN IV) | Depresses, abducts, and medially rotates the eyeball |
| Inferior Oblique | Oculomotor nerve (CN III) | Elevates, abducts, and laterally rotates the eyeball |
| Levator Palpebrae Superioris | Oculomotor nerve (CN III) | Elevates the upper eyelid |
 | ||
| ![[Note Pyramidal System-20240426004827251.webp | 292]] |
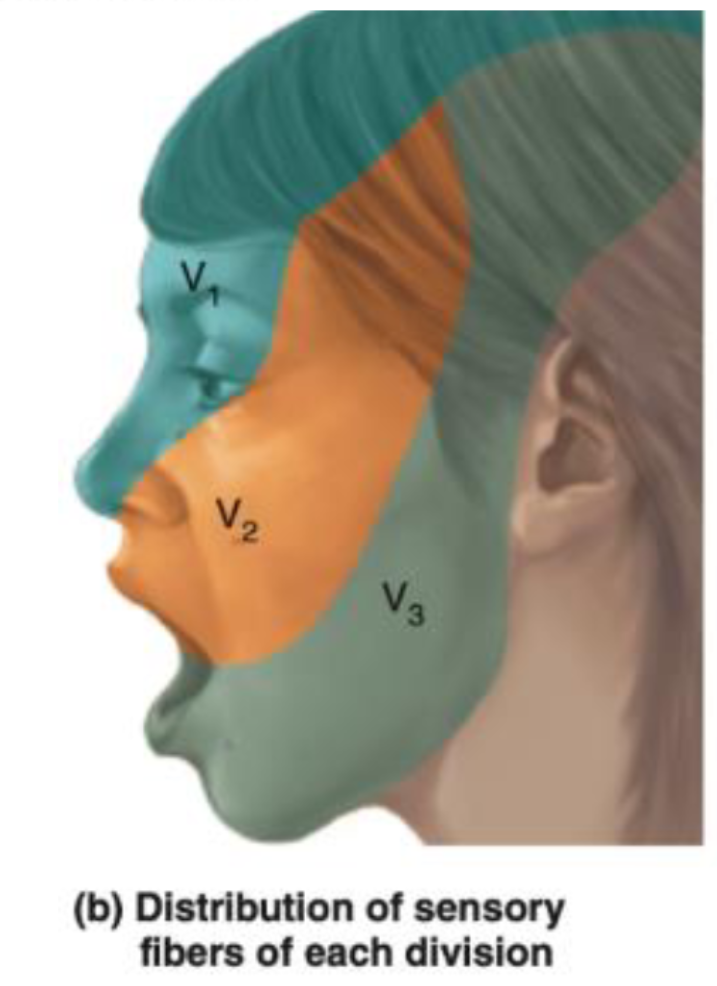
CN V – Trigeminal Nerve
-
Ophthalmic (V1) - Passes through the superior orbital fissure.
- Supplies: Sensation to the forehead, upper eyelid, and cornea.
- Involved in the corneal reflex: The afferent limb (sensory input) of the corneal reflex is through the ophthalmic branch of the trigeminal nerve. The efferent limb (motor output, which closes the eye) is via the facial nerve (CN VII).
-
Maxillary (V2) - Passes through the foramen rotundum.
- Supplies: Sensation to the middle part of the face, cheek, upper lip, and upper teeth.
-
Mandibular (V3) - Passes through the foramen ovale.
- Supplies: Sensation to the lower part of the face, lower lip, and lower teeth. It also carries motor fibers to the muscles of mastication.
- The anterior two-thirds of the tongue receives general sensation (not taste) via the lingual nerve, a branch of the mandibular division.
- Taste from the anterior two-thirds of the tongue is carried by the chorda tympani nerve (a branch of the facial nerve, CN VII), not the trigeminal nerve.
Examination process
-
Sensory Testing:
- Cotton Test: Use a soft piece of cotton to lightly touch different areas of the face. This tests the sensory function of all three branches of the trigeminal nerve. The patient should have their eyes closed during the test to rely solely on their sensory perception. Specifically, test:
- The forehead, upper eyelids, and cornea (ophthalmic branch).
- The cheeks, upper jaw, and upper teeth (maxillary branch).
- The lower jaw, lower teeth, and part of the tongue for general sensation (mandibular branch).
- Cotton Test: Use a soft piece of cotton to lightly touch different areas of the face. This tests the sensory function of all three branches of the trigeminal nerve. The patient should have their eyes closed during the test to rely solely on their sensory perception. Specifically, test:
-
Motor Testing: power (Medial and Lateral pterygoid, temporalis, masseter)
- Mandibular Movements:
- Ask the patient to clench their jaw to test the muscles of mastication, assessing the motor function of the mandibular branch (V3).
- Have the patient open their mouth and then move their jaw side to side, observing for any deviations or difficulties, which might indicate an issue with trigeminal motor function or asymmetrical muscle weakness.
- Mandibular Movements:
buccinator supplied by facial
-
Reflex: Jaw Reflex (afferent efferent) - Pure reflex Gently tap the jaw with the mouth slightly open to check the reflex. A normal response would be a slight and quick involuntary clenching of the jaw. An exaggerated response might suggest abnormalities in the reflex arc, which is primarily controlled by the sensory and motor roots of the mandibular branch.
Corneal reflex (Afferent Opthalmic - efferent by facial)
CN VII - Facial Nerve
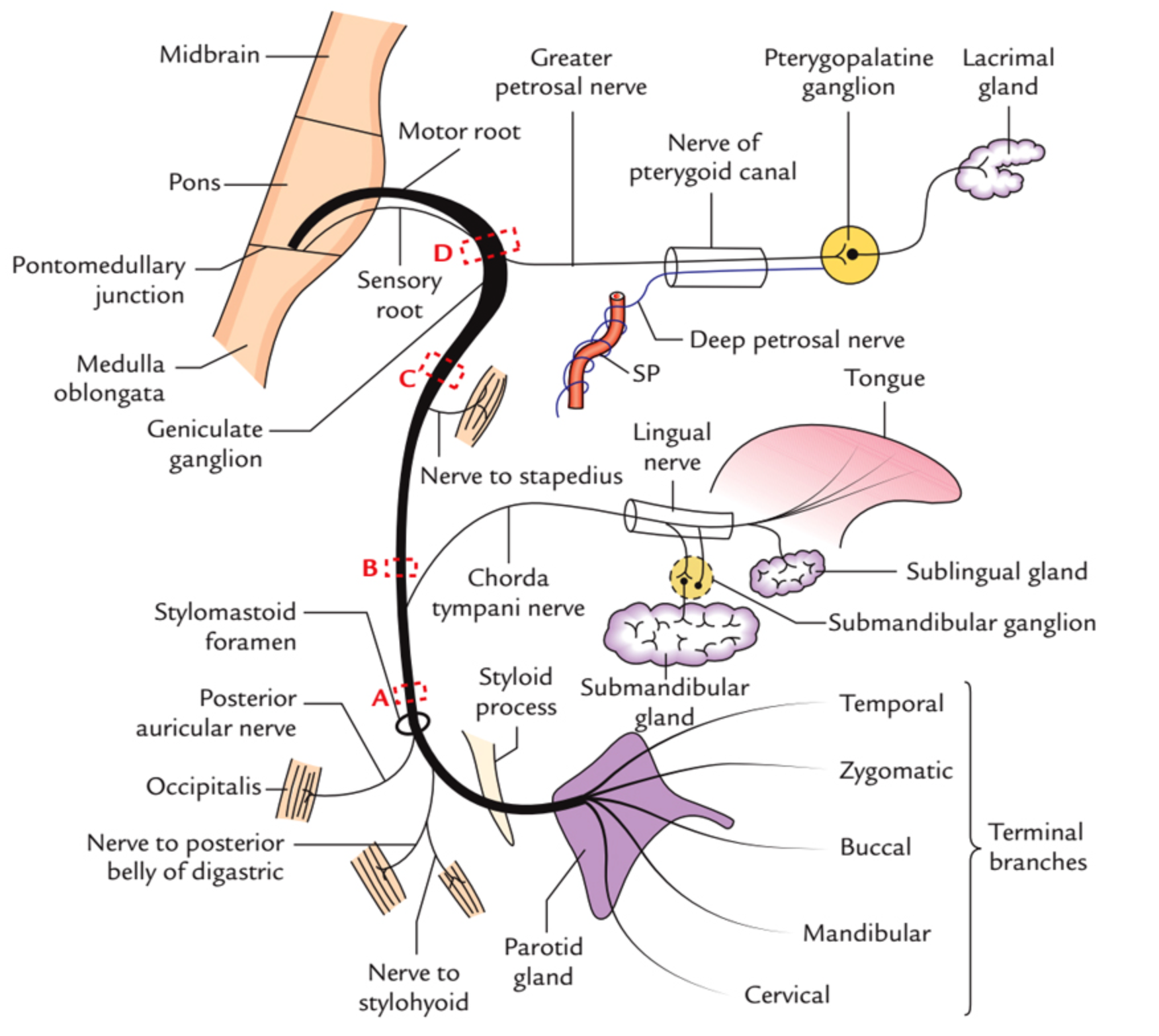 Course???
Course???
in middle ear gives two branches to chorda tympani & Stapedius (ear distrubance)
Innervations - External acoustic meatus - for sensation of ear - Motor - Movement of the face - Sternomastoid - branches nerve to stapedius - Loud sounds middle ear - & nerve to chorda tympani - Parasympathatic Submandibular & Sublingual gland
Tests
- Temporalis - raise eye brows (dont use hands )
- Orbicularis Oculi - check for resistance when eyes close
- Buccinator - Blow (palpate)
- Levator Anguli Superioris - smile
- Orbicularis Oris - whistle
- Taste anterior 2/3
 UMN Palsy - Causes Includes; (hyperreflexia)
- stroke
- MS
- trumours
- Internal capsule palsy
- Eyebrow raise is normal - if botox, contraindicated for the test
UMN Palsy - Causes Includes; (hyperreflexia)
- stroke
- MS
- trumours
- Internal capsule palsy
- Eyebrow raise is normal - if botox, contraindicated for the test
LMN Palsy - Causes includes
- Bells palsy
- Cavernous sinus thrombosis
- Fracture (truama) base of skull
- Acoustic neuroma
- Shingles
- Ramsay Hunt Syndrome with skin lesioned shingles on face and ear due to varicella ,
- Eyebrow doesn’t raise compared to contra-lateral
Bilateral facial nerve palsy - Sarcoidosis - Guillain-Barré Syndrome - Lyme disease
other notes botox mask symptoms of UMNL of facial nerve
most common causes of stroke? DVT - Stroke may transfer DVT to brain ASD - ventricular - patent foramin ovale
CN VIII - Vestibulocochlear
internal acoustic meatus enters to the skull depolization through potassium -
Cochlear division;
-
Whisper on ear while other is closed - tell him to repeat to confirm.
-
Rinne Test:
- This test compares air conduction to bone conduction. A tuning fork is used initially to assess bone conduction by placing it on the mastoid process. It is then held near the ear canal to assess air conduction.
- A positive Rinne test (air conduction is better than bone conduction) indicates normal hearing or sensorineural hearing loss.
- A negative Rinne test (bone conduction is better than or equal to air conduction) suggests conductive hearing loss.
-
Weber Test:
- This test assesses bone conduction using a tuning fork, which is placed on the center of the forehead.
- The purpose is to determine the lateralization of sound. Sound lateralization to one ear typically indicates sensorineural hearing loss in the opposite ear or conductive hearing loss in the ear to which sound is lateralized.
sensorineural causes - Neurofibromatosis type 2 - Noise pollution - Aminoglycosiedes - Gentamycin - Test, with ringing on frontal head - check for which ear hears most = laterilzation of normal side - Pendred Syndrome = Goiter + hearing loss (thyroid manifestations are rare, but may be presentaiton)
Conductive deafness - Wax / foreign objects - Otitis Media - - Tympanic membrane rupture - Otosclerosis. - Swimmers ear - Foreign body
Note
Fracture at the base of the skull can cause sensorineural hearing loss and bleeding, with lateralization. This is a result of conductive deafness, as the vestibulocochlear nerve passes through the petrous part of the temporal bone.
CN IX - Glossopharyngeal
Tests for Gag reflex Jugular foramen - Upper motor neuron palsy - glossopharyngeal special sense, pain and temperature autonomic to the parotid
examination by gag reflex with Glossopharyngeal & Vagus open mouth check uvula for Vagus for the tongue Hypoglossal
Main Causes - Neuralgias - Compression - Surgical
CN X - VAGUS
Cough, Gag reflex -
UML pseudobulbar palsy, - hot potato speech
bulbur palsy; LML - appear as nasal speech
9,10,11,12 bulbar palsy - by speech
CN XI - Accessory
-shrug, head switch
XII - Hypoglossal
-
All intrinsic and extrinsic muscles of tongue except palatoglossus by vagus
-
UML - Pseudobulbar palsy; Hot potato; Spastic
-
LML Bulbar Palsy; Nasal speech, appear as Fasucilation; Flaccid
-
Tongue goes to the side which is damaged
-
then check power of intrisic muscles of the tongue
4) Motor
UMNs
Transmit impulses from cortical nerve bodies to:
- motor nuclei in brainstem (CNs)
- Anterior horn cells of spinal cord
LMNs
Transmit impulses from anterior horn cells through anterior root into peripheral nerves
- Terminate at the neuromuscular junction
Motor Function Assessment
Inspection
- symmetry
- muscle bulk
- size and contours
- flat or concave; unilateral or bilateral; proximal or distal
- atrophy
Palpation
- muscle tone
Percussion fasciculations; Looks likes irregular ripples or twitches under the skin overlying muscles at rest commonly seen in LMN lesions.
They may be benign (physiologic) or drug induced (cholinergic). Check motor strength
Body position
- during movement and at rest
Involuntary movements
- location, quality, rate, rhythm, amplitude
- relation to posture, activity, fatigue, or emotions
Causes of atrophy
- motor neuron diseases
- disuse of muscles
- rheumatoid arthritis
- protein-calorie malnutrition
Causes of decreased muscle tone
- disease of PNS
- cerebellum dysfunction
- acute spinal cord injury
comparing both sides to note abnormalities:
- Bulk and nutrition of muscles.
- Tone of muscles.
- Power of muscles.
- Reflexes.
- Coordination of movements.
- Involuntary movements.
- Gait.
Test muscle strength
Grade 0 to 5
Muscle strength
- wide variance - stronger dominant side
- test by asking patient to actively resist movement
- if muscles too weak - test against gravity only or eliminate gravity
- if patient fails to move, watch or feel for weak contraction
| Grade | Muscular Respone |
|---|---|
| 0 | No contraction detected |
| 1 | Barely detectable flicker or trace of contraction |
| 2 | Active movement with gravity eliminated |
| 3 | Active movement against gravity (raise leg / arm) |
| 4 | Active movement against gravity and some resistance |
| 5 | Active movement against resistance without evident fatigue - “Normal” |
Tone & Power
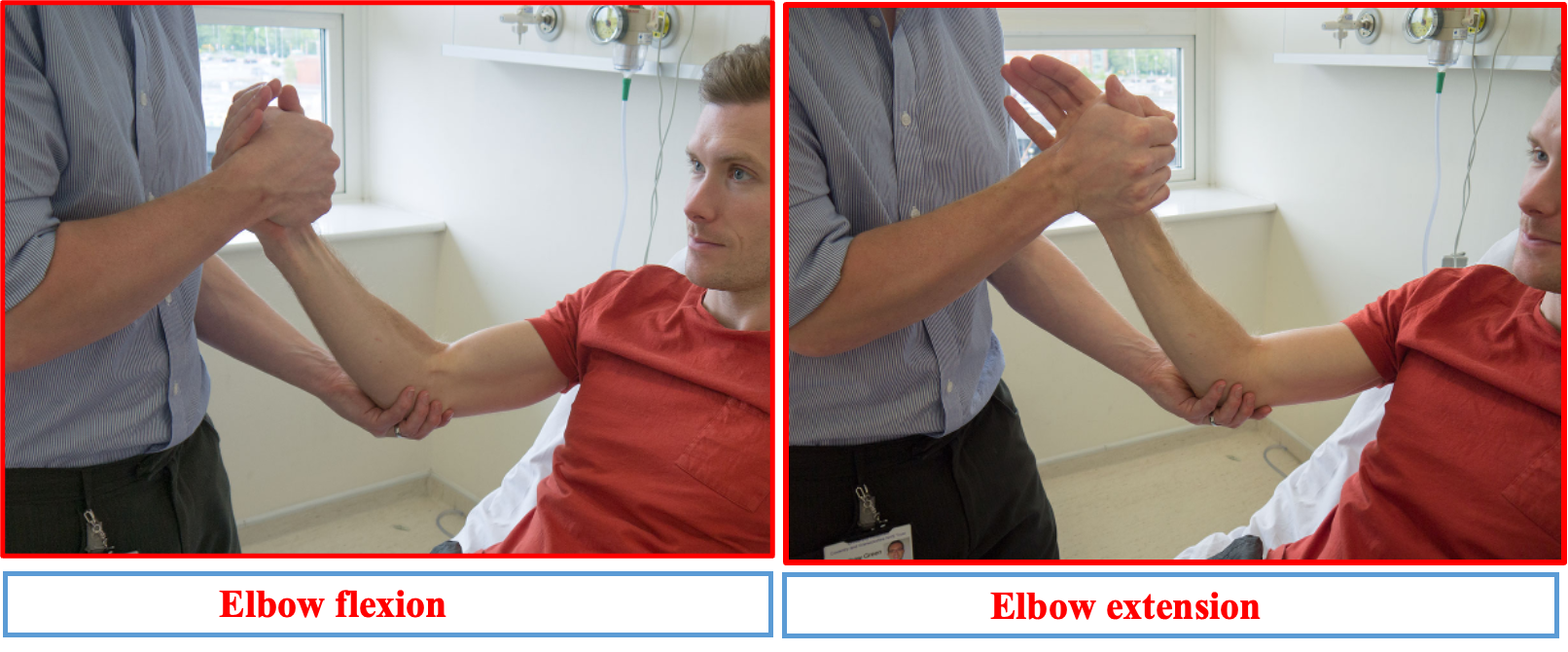
UL MOTOR EXMINATION
Tone Start proximally at the shoulder, feeling how easy the joint is to move passively. Then move down to the elbow, wrist and hand joints, again assessing each one’s tone in turn.

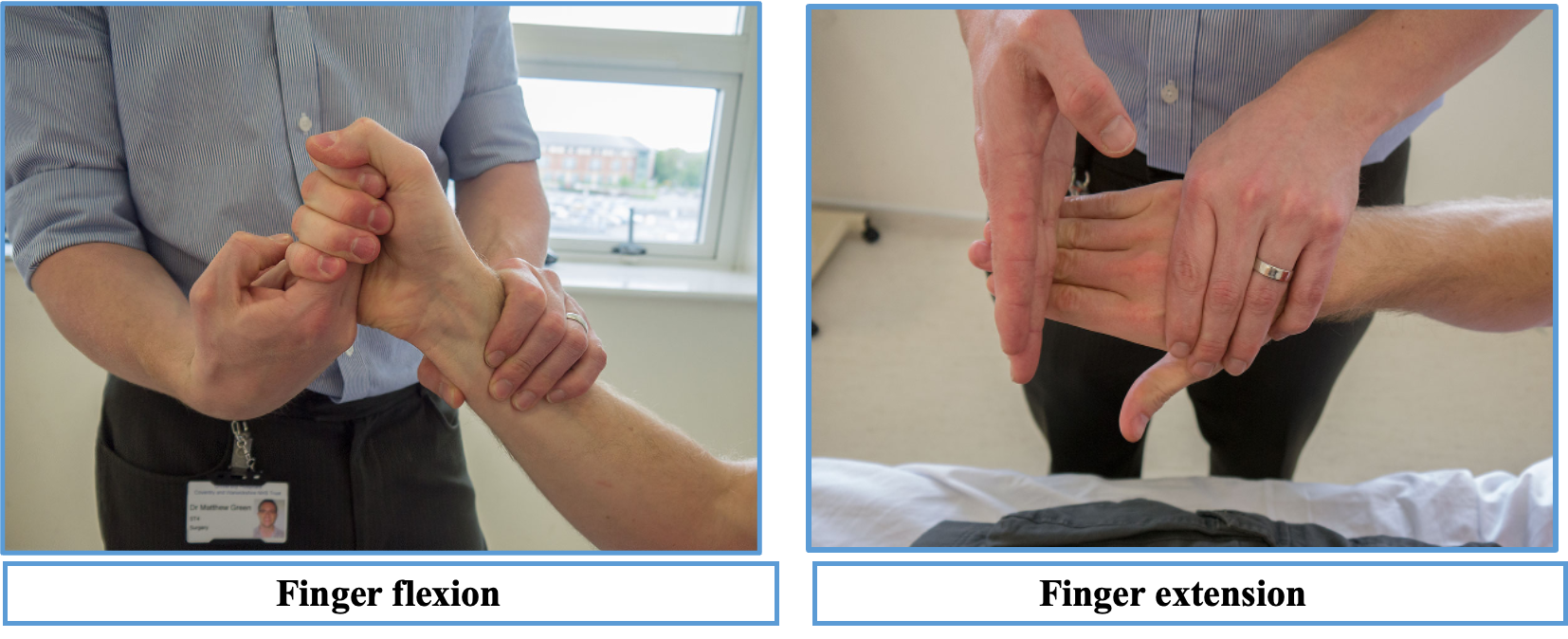
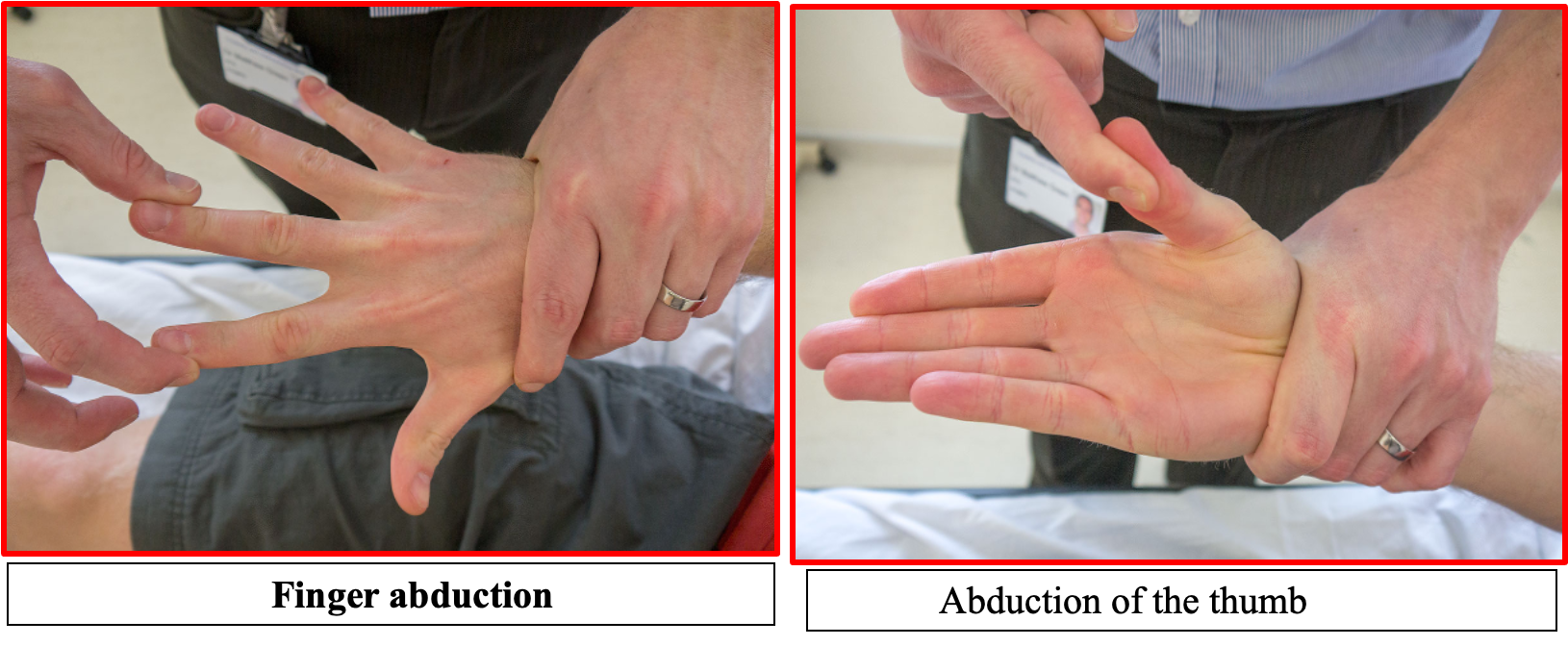
Power
Start at the shoulder asking the patient to abduct and adduct against your hand so you can assess how much force they can overcome. Do the same for flexion and extension at the elbow and wrist, as well as the fingers; also checking abduction and adduction of the thumb.


LL MOTOR EXMINATION
Tone As with all examinations, the best method is your own – one with which you are comfortable and familiar. The one explained here takes the following format:
- Tone.
- Power.
- Reflexes.
- Function.
- Sensation.
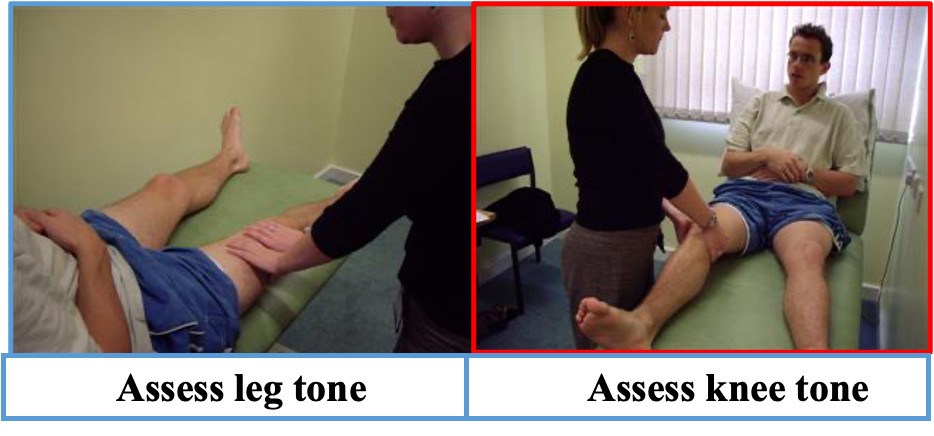
Power A full motor system examination includes assessment of the legs and the following format:
- Tone.
- Power.
- Reflexes.
- Function.
- Sensation.
Start at the hip asking the patient to abduct, adduct, flex and extend against your hand so you can assess how much force they can overcome.
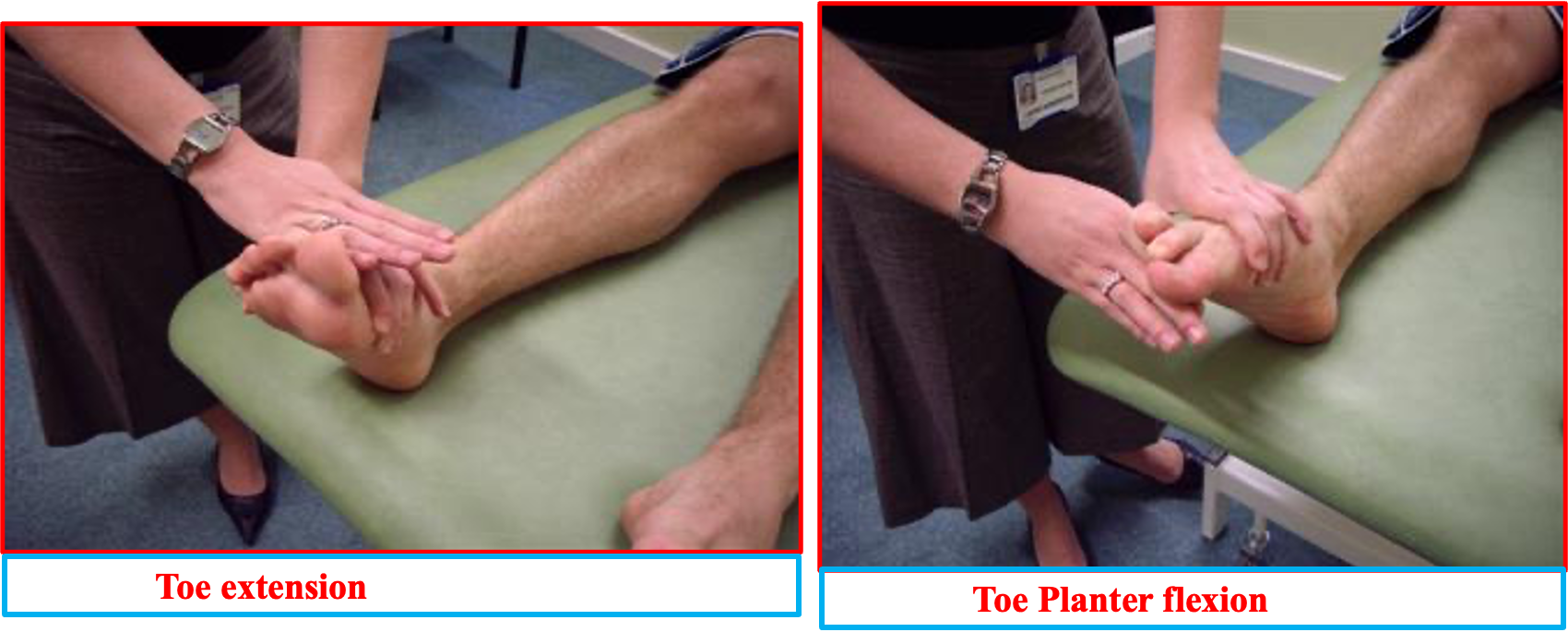
Do the same for flexion and extension at the knee and ankle as well as the toes.

KNEE FLEXORS/ AND XTENSORS

Toe extention and flexion power assessment)
Toe extension involves extending the toes away the sole of the foot. The muscle of the toe extension is extensor digitorum longus, and the intrinsic foot muscles.
Toe flexion involves bending the toes towards the sole of the foot. The muscle and tendon involved in toe flexion is flexor digitorum longus and intrinsic foot muscles.
Hypotonia:
It is decreased tone and usually associated with muscle wasting,weakness and hyporeflexia. Feature of cerebellar disease and occurs in early phases of cerebral or spinal shock
Hypertonia:
There are 2 principal types hypertonia; Spasticity & Rigidity
A- Spasticity: increased tone throughout range of motion, and then there is a sudden release (catch). Seen in UMN lesion. Spasticity is velocity dependent(sudden release).
Usually accompanied by
- weakness
- hyperreflexia
- extensor planter response
- clonus
B- Rigidity: increased tone throughout the range of motion. If intermittent and regular interruption to the movement gives jerky feeling, is called cogwheel rigidity, which is seen in extrapyramidal diseases such as Parkinson’s disease. Rigidity is not velocity dependent (continuous)
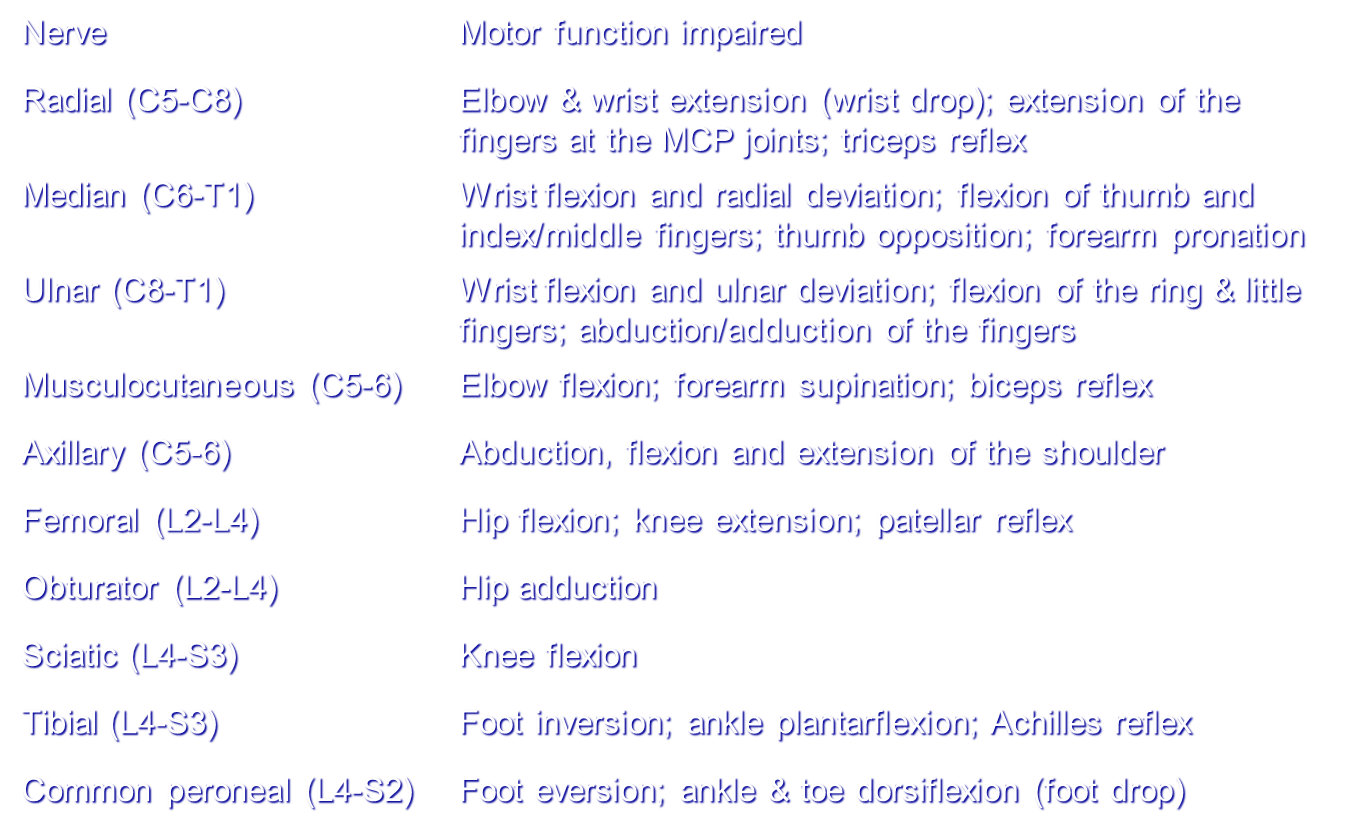
Function and Innervations
Other tests
Hoffman’s sign is an involuntary flexion movement of the thumb and or index finger when the examiner flicks the fingernail of the middle finger down. This has sensitivity of 59% and a specificity of 49% to screen for upper motor neuron lesion (UMN lesions).

5) Sensory / Proprioception
Spinothalamic Tract
- Pain and Temperature
- Crude touch (Light Touch without localization)
- Fibers cross & pass upward into thalamus
Posterior Columns
- Position and vibration
- Fine touch
- Synapse in medulla, cross & continue on to thalamus
Sensory specific testing
- Temperature
- Vibration (tuning fork applied on various points)
- Proprioception (Up, Down fingers)
- Tactile localization (eyes closed, ask patient what place is touched)
- Discriminative sensations
- Stereognosis (identify object whilst closed eye)
- Graphesthesia (Identify number written hand while eyes closed)
- Two-Point Discrimination (Two Pin differentiation)
Peripheral Nerve Injuries
- Median nerve = atrophy of thenar emminence
- Ulnar nerve = atrophy of the hypothenar emminence
UL
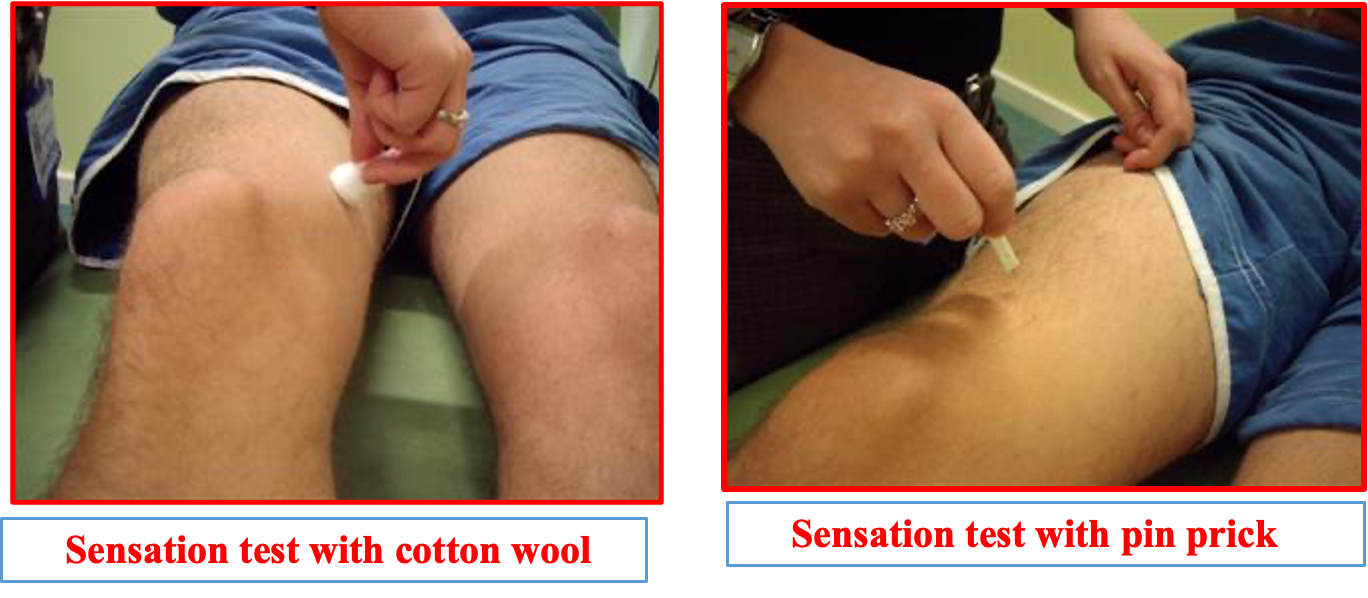
Sensation
- Testing light touch, pin prick, vibration, and joint position sense, or proprioception.

Light Touch
-
Ask the patient to place their arms by their sides with their palms facing forwards. Lightly touch the patient’s sternum with a piece of cotton wool so that they know how it feels.
-
Then, with the patient’s eyes shut, lightly touch their arm with the cotton wool. The places to touch them should test each of the dermatomes – make sure you know these! Tell the patient to say “yes” every time they feel the cotton wool as it

UL Proprioception/tuning fork test)
Vibration
-
To assess vibration you should use a sounding tuning fork. Place the fork on the patient’s sternum to show them how it should feel.
-
Now place it on the bony prominence at the base of their thumb and ask them if it feels the same. If it does, there is no need to check any higher. If it feels different you should move to the radial stylus and then to the olecranon until it feels

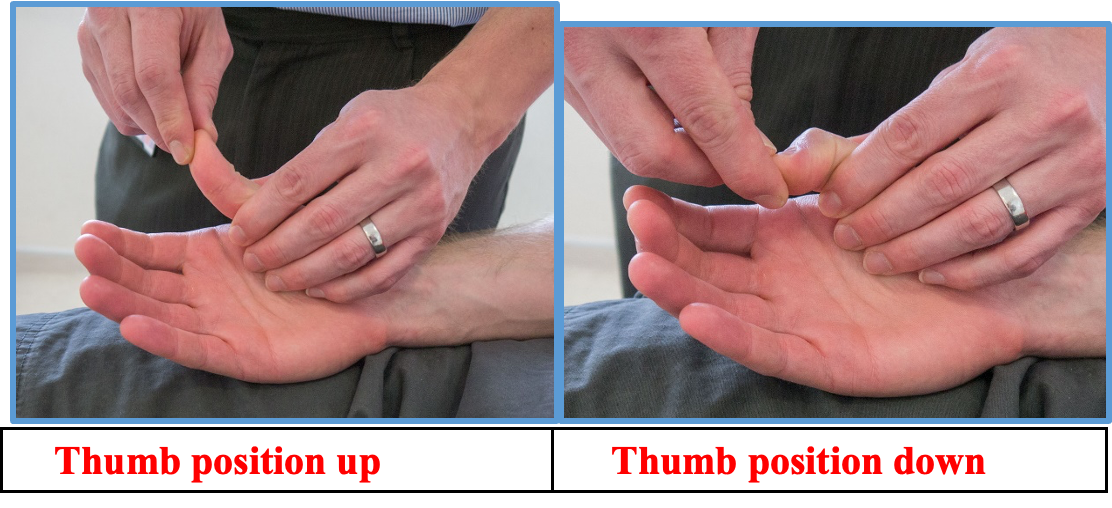
UL Proprioception joint position
Proprioception
-
Assess proprioception Hold the distal phalanx of the thumb on either side so that you can flex the interphalangeal joint.
-
Show the patient that when you hold the joint extended, that represents Up whereas when you hold it flexed that represents Down. Ask the patient to close their eyes and, having moved the joint a few times hold it in one position – up or down. Ask the patient which position the joint is in.
 LL
LL
(Lower limb touch and pain assessment)
Sensation Sensations to be tested include light touch, pin prick, vibration, and joint position sense, or proprioception.
Light Touch
Ask the patient to place their legs out straight on the bed. Lightly touch the patient’s sternum with a piece of cotton wool so that they know how it feels.
With the patient’s eyes shut, lightly touch their leg with the cotton wool. The places to touch the patient should test each of the dermatomes
Lower limb proprioception JPS
Proprioception Hold the distal phalanx of the great toe on either side so that you can flex the interphalangeal joint. Show the patient that when you hold the joint extended, that represents Up whereas when you hold it flexed that represents Down. Ask the patient to close their eyes and, having moved the joint a few times hold it in one position – up or down. Ask the patient which position the joint is in.

Lower limb proprioception (vibration)
Vibration
To assess vibration, use a sounding tuning fork. Place the fork on the patient’s sternum to show them how it should feel.
Now place the tuning fork on their great toe and ask them if it feels the same. If it does, there is no need to check any higher. If it feels different you should move to the tibial epicondyle and then to the greater trochanter until it feels normal.

6) Reflexes
- Corneal
- Pharyngeal
- Biceps Reflex
- Triceps Reflex
- Brachioradialis Reflex - Supinator Reflexes
- Abdominal reflexes
- Patellar (knee jerk)
- Achilles (ankle jerk)
- Anal Reflex
Deep Tendon Reflexes Hyperactive reflexes
- suggest CNS disease
- sustained clonus (confirms)
Diminished or absent reflexes
- loss of sensation
- damage to spinal segments
- damage to peripheral nerves
- diseases of muscles
- diseases of the neuromuscular junctions
Spinal Reflexes: DTRs Z https://www.youtube.com/watch?v=3DTXyIoXfJI
| Reflex | Segmental Level |
|---|---|
| Supinator Reflexes | C5, 6 |
| Biceps Reflex | C5, 6 |
| Triceps Reflex | C6, 7 |
| Abdominal reflexes - upper | T8, 9, 10 |
| Abdominal reflexes - lower | T10, 11, 12 |
| Knee (Patellar Reflex) | L2, 3, 4 |
| Plantar Reflex - Babinski | L5, S1 |
| Achilles Reflex | S1 primarily |
| Anal Reflex | S2 - S4 |
| Plantar Reflex | |
| Upgoing/extensor (Babinski positive) |
Lower motor neuron lesion (Extensors are abnormal, Flexors are normal)
Deep Tendon Reflexes: Grading
| Grade | Response |
|---|---|
| 4+ | Very brisk, hyperactive, with clonus |
| 3 | Brisker than average, slightly hyperreflexic |
| 2 | Average, expected response; normal |
| 1 | Somewhat diminished, low normal |
| 0 | No response, absent |
Jendrassik’s Maneuver Reinforcement technique Upper extremities
- clench teeth
- squeeze thigh
Lower extremities
- lock fingers and pull one against the other
Other tests
ANKLE AND PATELLAR CLONUS
Clonus: is an abnormal reflex response that involves involuntary and rhythmic muscle contractions. Like other signs of upper motor neuron syndrome clonus indicates some insult to the central rather than peripheral nervous system, so part of its utility as a clinical examination skill is in differentiating the two.

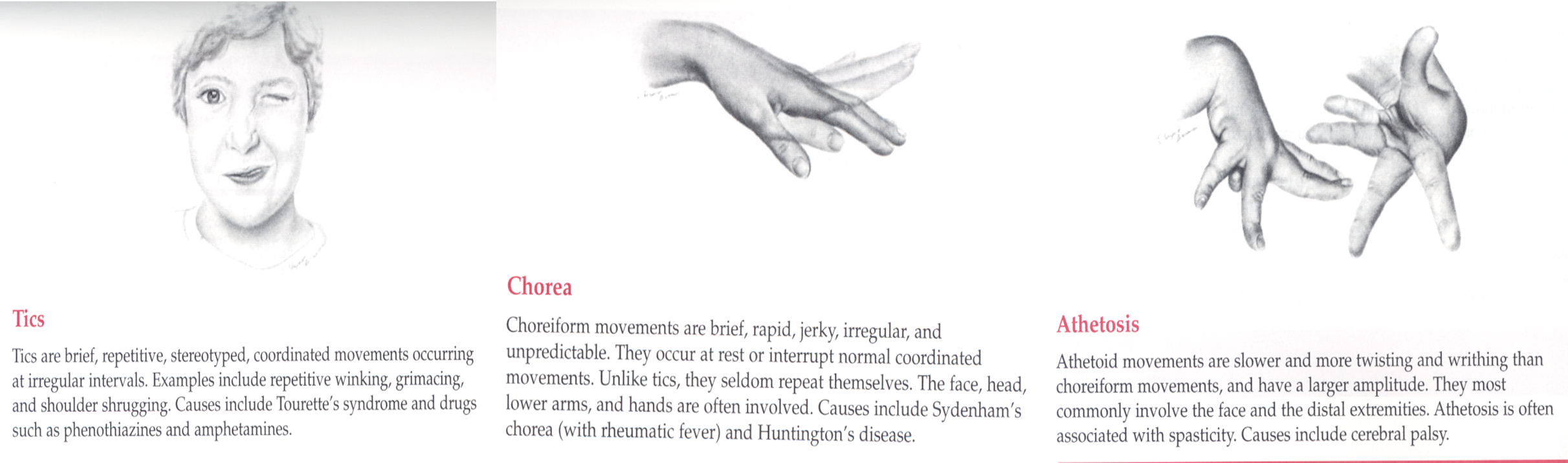
Abnormal Movements
7) Cerebellar
Common causes
- Trauma; RTA ⇒ Post. Cranial Fossa fracture
- Demyelination (Multiple sclerosis) - Myelin sheath gives whitish color, if destruction, neuron conduction would be slow (T2 enhancement MRI) “((tachycardia, ataxia, Lower motor neuron lesion, cardiomyopathy”
- Tumor (Very rare, except meningioma) paraneuroblastic tumor, PCE, or Cerebellum itself + SOL- Irreversible damage
- SOL manifestation - due abscess, tumor, etc..
- Ischemia PICA Occlusion
- Degeneration (Multiple system Atrophy)
- Paraneoplastic syndrome if there is no manifestation to cerebellum due to metastasis
- Drug Induced; (Alcoholism, Phenytoin)
- Celiac disease
Coordination
Cerebellar disease
- incoordination is worse with eyes closed
dysmetria
- point-to-point movements are clumsy, unsteady, inappropriately varying in speed, force, & direction
- may initially overshoot mark but finally reaches it
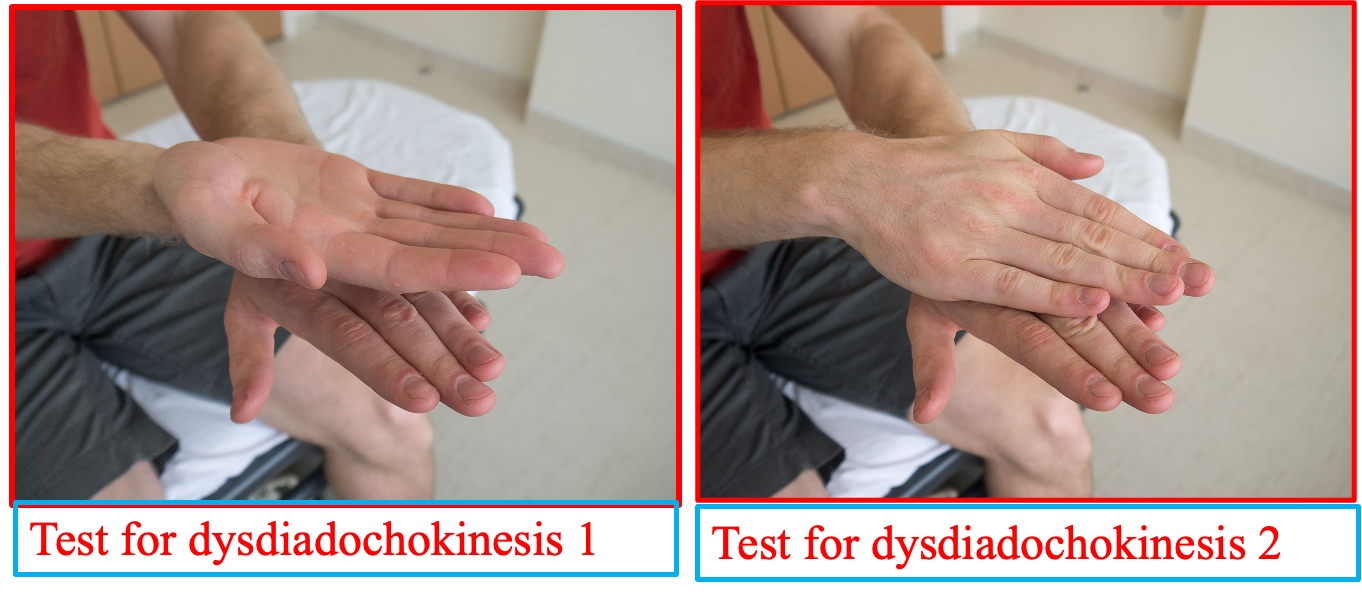
Cerebellar Function
Assessed by:
- Rapid alternating movements
- Tremor & Tone assessment
- Finger-to-Nose Test
- Heel-to-Knee Test
- Romberg’s Test + Pronator Drift
- Gait
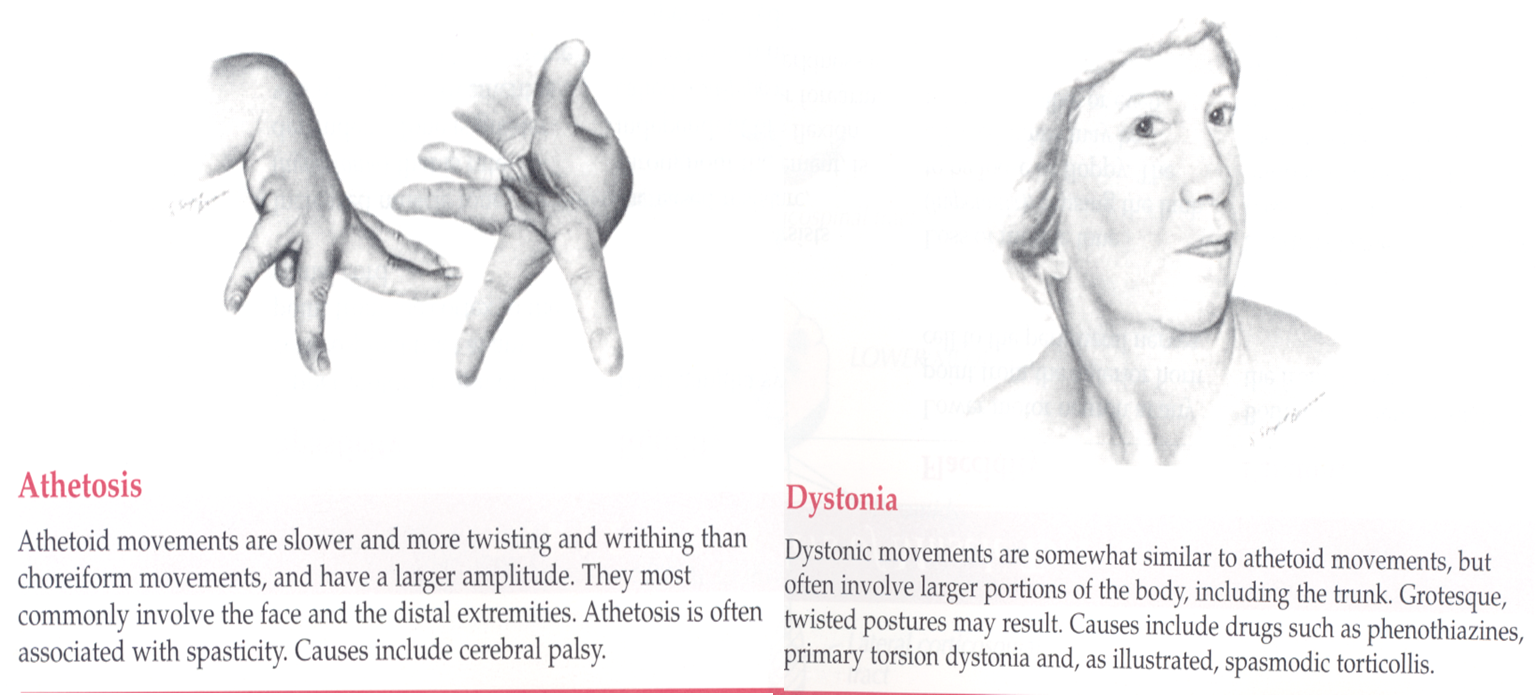
A) Rapid Alternating movements
- First with hands
- Repeat with feet
- Diadochokinesia = ability to perform RAM
- Dysdiadochokinesis = slow, irregular, clumsy movements

Cerebellar function (dysdiadochokinesis)
Co-ordination: Test for dysdiadochokinesis by showing the patient how to clap by alternating the palmar and dorsal surfaces of the hand. Ask them to do this as fast as possible and repeat the test with the other hand.
B) Cerebellar function (tremor & tone assessment)
Check for a resting tremor in the hands by placing a piece of paper on the patient’s outstretched hands.
Test tone in the arms (shoulder, elbow, wrist).

Cerebellar vs. Basal Ganglia lesions
| Region | Signs and Symptoms |
|---|---|
| Cerebellar | - Awkwardness of intended movements |
| - Intention tremor | |
| - Ataxia | |
| Basal Ganglia | - Involuntary movements |
| - Resting tremor | |
| - Chorea | |
| - Athetosis | |
| - Hemiballismus |
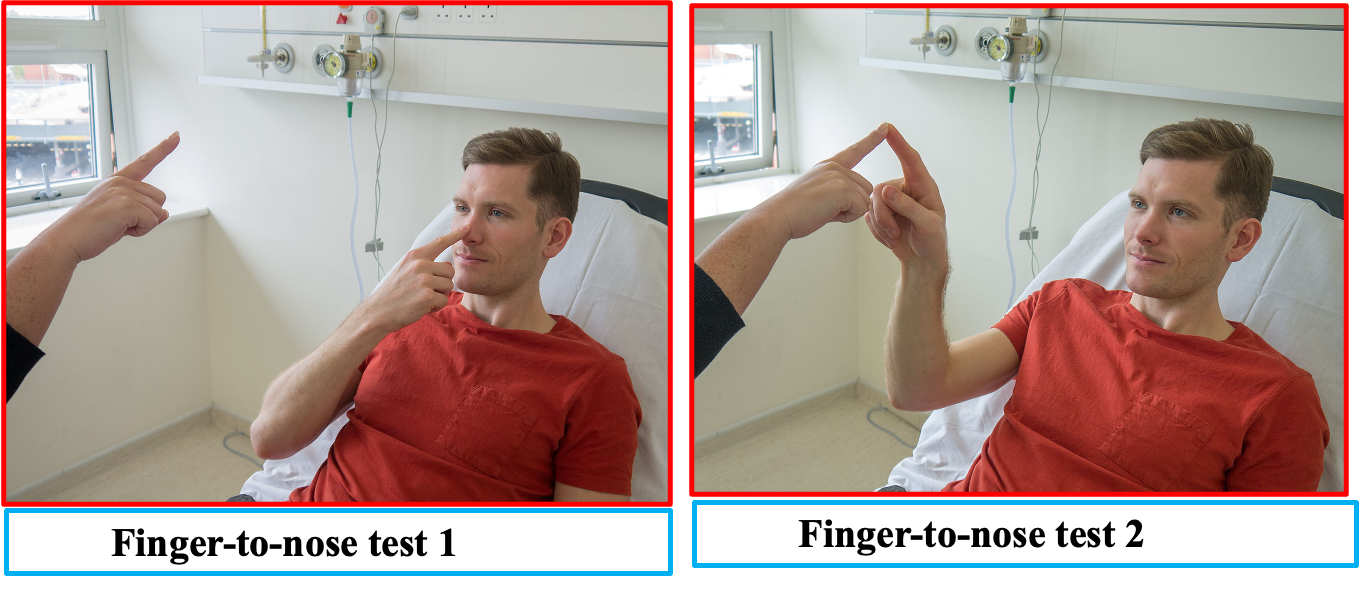
C) Fingers-nose
Finger-to-nose with moving target
Stationary finger-to-nose with eyes closed
FINGER NOSE TEST
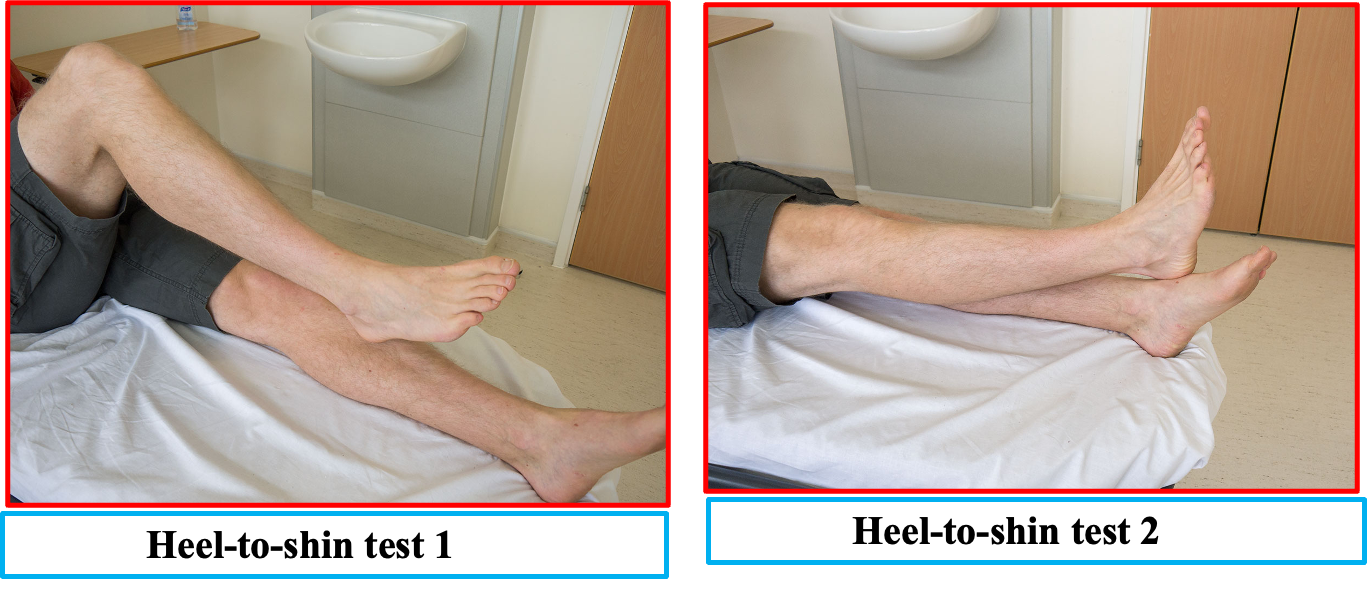
D) Heel-to-Knee Test
HEEL SHIN TEST
Perform the heel-to-shin test. Have the patient lying down for this and get them to run the heel of one foot down the shin of the other leg, and then to bring the heel back up to the knee and start again. Repeat the test with the other leg.
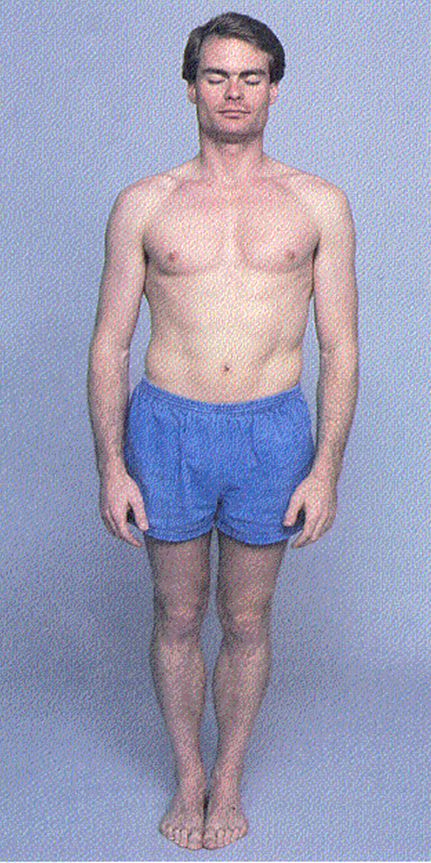
E) Romberg’s test
Station, Stance & Romberg’s Test
Station & Stance
- Pt stand with feet together
- First, eyes open
Romberg Test
- Then, close eyes
- If okay with eyes open, but sways w/ eyes closed = + Romberg
- Mainly tests position sense
- Vision can compensate for loss of position sense
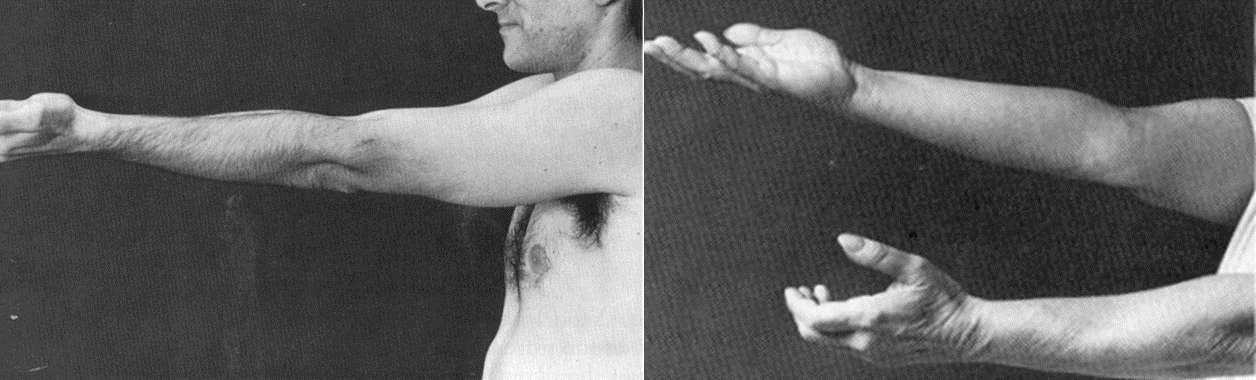
F) Pronator Drift
Often performed in conjunction with Romberg test
- Pronator drift
- Muscular strength
- Coordination
- Position sense
G) Gait
\The cerebellar examination is performed in patients with neurological signs or symptoms of cerebellar pathology, for example: dizziness, loss of balance, or poor co-ordination. There are many causes of cerebellar dysfunction and include vascular, for example: stroke, space-occupying lesions, multiple sclerosis, and genetic conditions such as Friedreich’s Ataxia.


The cerebellar examination needs to reflect these symptoms and as such involves examining the gait, balance and co-ordination.
Tandem gait: The examiner asks the patient to walk in a straight line with the heel of the leading foot touching the toes of the lagging foot as if walking on a tightrope.
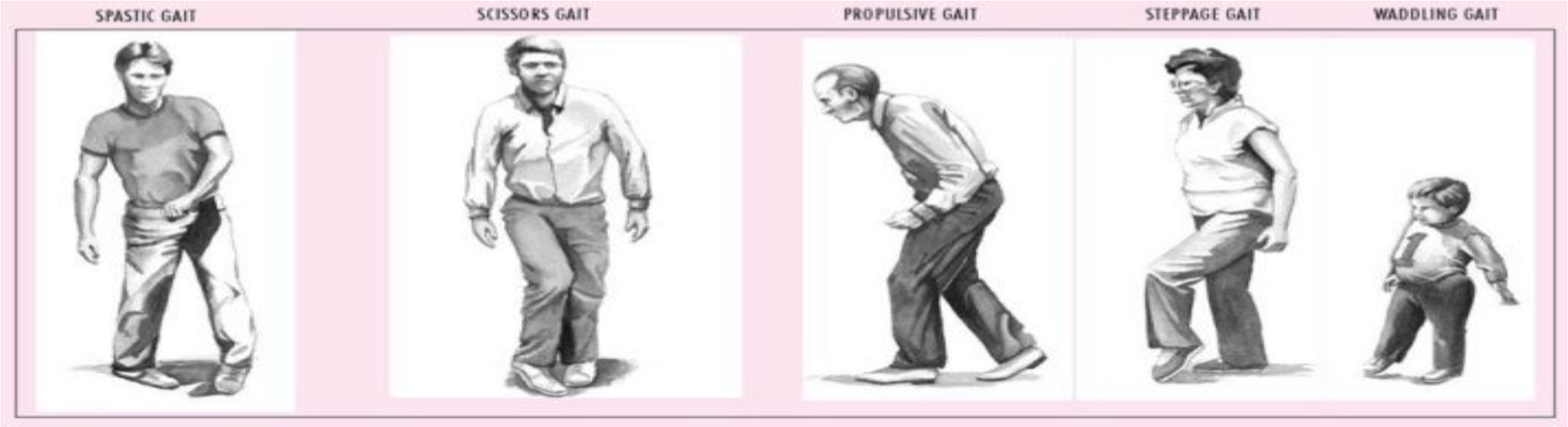
| Gait Type | Description | Causes |
|---|---|---|
| Spastic Gait | Stiff, awkward movements with legs held close together and dragging feet. | - Cerebral palsy - Multiple sclerosis - Stroke - Spinal cord injury - Brain injury |
| Scissor Gait | Legs cross over each other while walking, resembling the motion of scissors. | - Cerebral palsy - Spinal cord injury - Multiple sclerosis - Spastic diplegia |
| Propulsive Gait | Stooped, rigid posture with small, shuffling steps, often leaning forward. | - Parkinson’s disease - Progressive supranuclear palsy - Basal ganglia disorders |
| Steppage Gait | High stepping, lifting the foot higher than usual to avoid dragging toes. | - Peripheral neuropathy - Foot drop (due to peroneal nerve injury) - Guillain-Barré syndrome |
| Waddling Gait | Swaying from side to side, often with a wide stance. | - Muscular dystrophy - Hip dysplasia - Myopathy - Congenital hip dislocation |
| Tandem Gait | Walking in a straight line, heel-to-toe, often used in neurological exams. | - Cerebellar ataxia - Alcohol intoxication - Vestibular disorders - Multiple sclerosis |
| Hemiplegic Gait | One leg is stiff and swings in a semicircle, with the arm on the same side flexed. | - Stroke - Traumatic brain injury - Cerebral palsy (hemiplegic type) - Multiple sclerosis |
| Spastic Hemiplegic Gait | Similar to hemiplegic gait but with increased muscle tone and stiffness. | - Stroke - Cerebral palsy (spastic hemiplegia) - Traumatic brain injury - Multiple sclerosis |
Other Notes
Spinal thalamic track
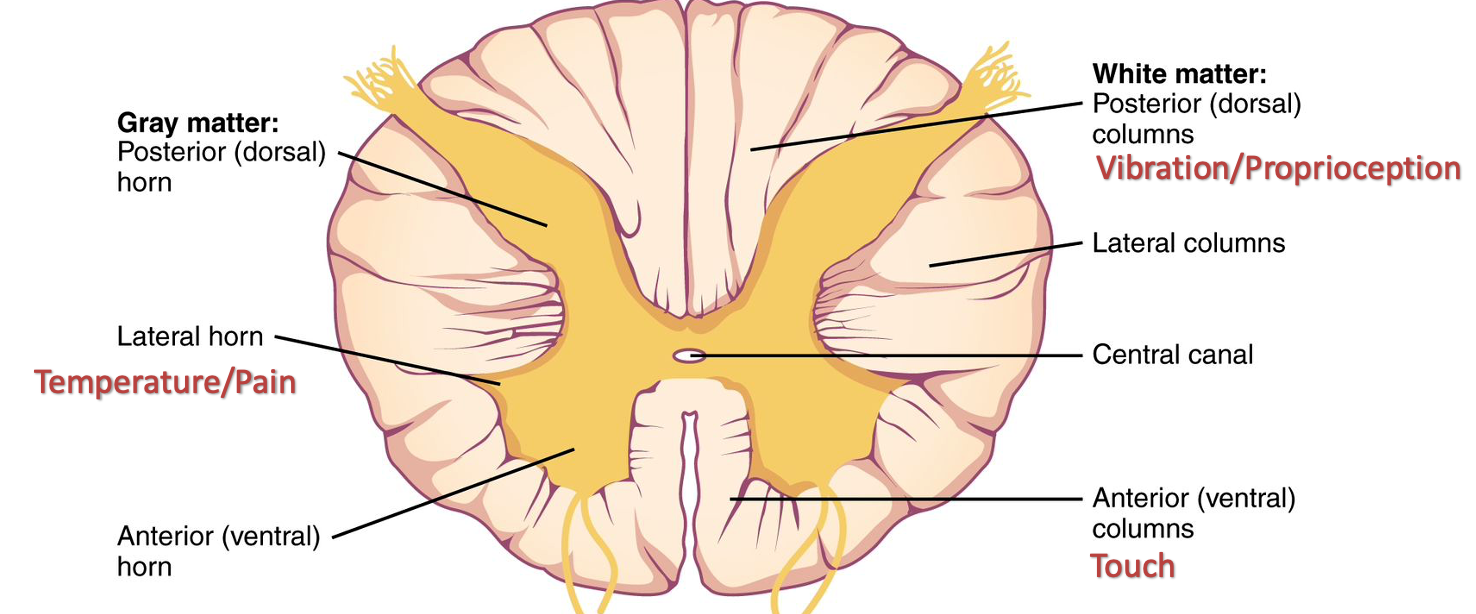
- Posterior Column; Vibration/Proprioception
- Anterior (ventral) Column; Touch
- Lateral Horn; Temprature/Pain
UML vs LML ↑ ↓
- Fasciculation ↓ = LMN
- Bulk; ↓ = LMN
- Tone - ↓ = LMN
- Reflexes - ↓ = LMN
- Babinski; Positive = UML
- Power - ↓ UML & LML
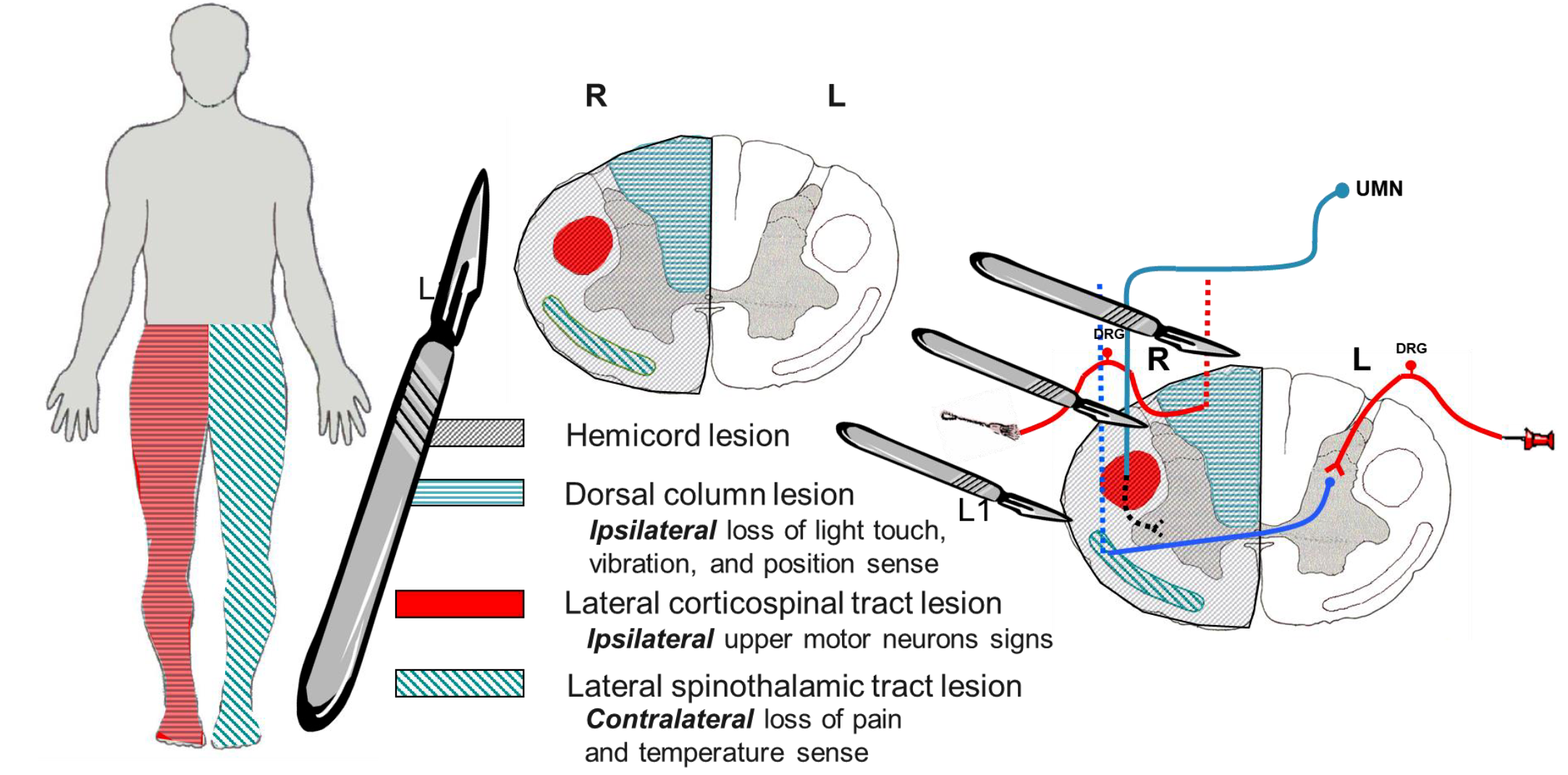
Brown squart syndrome
Lesion results in:
Dorsal column lesion – Ipsilateral loss of light touch, vibration, and position sense Lateral corticospinal tract lesion – Ipsilateral upper motor neurons signs Lateral spinothalamic tract lesion – Contralateral loss of pain and temperature sense
DM neuropathy
- staking pattern test on both legs
Physiotherapy neuro-plasticity to return the baseline
Cases
C1
Male 53 year old pakistani with known case of DM, HTN, occasional smoker for last 10 years, and sedentary lifestyle taking medication of aspirin, insulin, metformin, glavix with no known allergies
Patient previously admitted with chest pain, no hx of surgeries, family hx strongly positive cardiovascular comorbidity.
Presented to Clinic with 3d hx of numbness on right side of face and lt lower limb side of body, slurred speech which have improved
- no dizziness
- no vomiting
- no chestpain
- no joint pain
- no fasiculation
- no headache
- no visual loss
- no hearing loss
- no muscle bulk even on induction
- no fasciculation
- no gastrointestinal, respiratory, or urinary abnormality
O/E; on examination
- Patient is concious and orientated - GCS 15/15
- slurred speech but improved
- focal neurological loss
- rinne’s test normal
- power grade 5
- normal reflexes (biceps, triceps, supinator, plantar, heel, knee)
- no sensory loss at time of examination
in vibration you dont have to go in continuem from the toe exception of pain
Assessment
- Stroke - focal neurological loss - Sudden onset, Progressive, slurred speech, cant move any leg - UML
- SOL - visual loss/ headache; already ruled out from history
- MS - usually female 40s with numbness, fatigue, eye pain, visual disturbance - with multisystem appearance - Convergence. - LML; already ruled out from history
Investigation
- Check Vital signs; Make patient stable
- basic investigation - cbc
- CT - hemorrhage
- MRI - for infarction; mri is not recommended in case of stroke, as it takes long time to take.
- D dimer
- Echocardiogram, cerebral angiogram, carotid US
Initial Treatment with stroke???
- less than 4h- with thrombolysis
-
4h - targeted thrombolytics - interventinal radiology thr
-
6-7h - aspirin
C2
34 yrs male with known case of DM; possibly MODI, DM1 & HTN, hx of seizure 4D ago, right side weakness, headache, diplopia
o/e
- RT upper/lower limb hypertonia
- RT upper/lower limbs decreased power
- No knee reflex
- shock stasis
- Equivocal RT
Investigations
CT: no abnormal findings finding
Differential
C3
headache for 3 days - - associated with photophobia constant for 3 hours before presentation - also theres hx of numbness with no seizure, no neck stiffness
C4
History
Make sure to include past Hx of travel; mecca & Surgery; cranial surgery
S/S/ | HOP
- Altered mental status; most likely TB protein deposition
- Vomitting
- Neusea
- Fever
- Neck stiffness
- Headache increases with neck movement
Examination:
- B sign
- Ta sign
Investigations:
- LP - make sure to do CT, Fundoscopy to rule out sign of intracranial pressure
- CT
- Fundoscopy; Papilledema
- Basic Investigations
- Geimsa, indian ink, PCR
CSF Characteristics
Bacterial vs TB vs Viral Cell count differentials
Effective treatment for meningitis
treat as early possible with empiric antibiotics depending on age group
Q&A
Partially treated meningitis? Menningo encephalitis> Staph - vancomycin viral - acyclovir tb - anti tb rifa