Acute Abdomen
Mohammed Al Sebayel
Essentials
The ‘acute abdomen’ is defined as a sudden onset of severe abdominal pain of less than 24 hours duration.
Structured approach
Initial assessment of acute surgical problem
- Does it need immediate and prompt surgical intervention, or urgent medical therapy.
- critically unwell, give oxygen, start suitable initial steps, and call for help early before going into detail on the history and examination.
Grade of Operative Surgical Urgency in Acute abdomen:
Immediate action: bleeding
- Rupture aortic aneurysm
- Bleeding ulcer (gastric or duodenal)
- Trauma.
- Rupture ectopic. (ask menstrual period, pregnancy, …)
Emergency action: Perforations
- (peptic ulcer, small or large bowel perforation, diverticular disease, Inflammatory bowel disease, Bowel obstruction, Mesenteric Ischemia
Urgent action: Inflammation
- Colic……..Biliary Colic ……Acute Cholecystitis
- Peritonism (localized Peritonitis)…… Acute Appendicitis
Non urgent: Biliary Colic without cholecystitis and renal colic
Colic Colic is an abdominal pain that crescendos to become very severe and then goes away completely. This is most typically seen in either ureteric obstruction or bowel obstruction.
Biliary ‘colic’ is not a true colic as the pain does not go away completely, instead getting periodically better and worse (colloquially termed ‘waxes and wanes’)
Presentations Requiring Immediate /Urgent Surgery
-
The most serious cause of intra-abdominal bleeding is a Ruptured Abdominal Aortic Aneurysm (AAA) which requires swift referral to the vascular team and immediate surgical intervention.
-
Other common causes usually involve a slower rate of bleeding, but with urgent surgery still required, include Ruptured Ectopic Pregnancy, bleeding Peptic Ulcer and Trauma.
-
These patients will typically go into hypovolemic shock. Clinical features include tachycardia and hypotension, pale and clammy on inspection, and cool to touch with a thread pulse.
Indications for Urgent Operation IHOP
- Ischemia - 4 HR until death -
- Hemorrhage
- Obstruction
- Perforation (Perforated Viscus)
| Somatic | Visceral |
|---|---|
| • Nociceptors are involved | • Involves hollow organ and smooth muscle nociceptors that are sensitive to stretching, hypoxia and inflammation |
| • Often well localized | • Pain is usually referred, poorly localized, vague and diffuse |
| • Usually described as throbbing or aching | • May be associated with autonomic symptoms (e.g., pallor, sweating, nausea, blood pressure and heart rate changes) |
| • Can be superficial (skin, muscle) or deep (joints, tendons, bones) |
PAIN:
- Site.
- Onset and progression.
- Character.
- Referred.
Referred Pain:
- Biliary Colic: to right shoulder or scapula
- Renal colic: to groin
- Appendicitis: periumbilical to right lower quadrant (RLQ)
- Pancreatitis: to back
- Ruptured aortic aneurysm: to back or flank
- Perforated ulcer: to RLQ (right paracolic gutter)
- Hip pain: to groin
Most Common Presentations of Surgical Pain
-
Sudden onset with rigid abdomen = perforated viscus
-
Pain out of proportion to physical findings = ischemic bowel (Abdomen soft lax with extreme pain)
-
Vague pain that subsequently localizes = appendicitis or other intra-abdominal process that irritates the parietal peritoneum
-
Waves of colicky pain = bowel obstruction
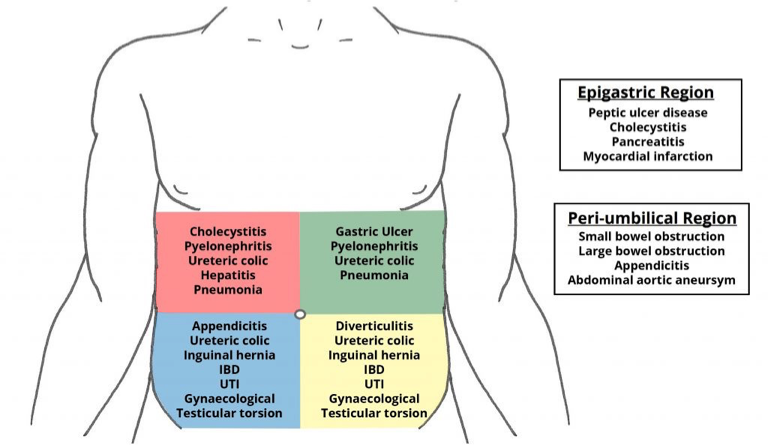
Acute Abdomen by region
In all patients presenting with an acute abdomen, order the following:
KEY TESTS FOR SPECIFIC DIAGNOSIS
- ALP, ALT, AST, bilirubin - liver
- Lipase/ amylase - pancreatic
- Urinalysis - kidney
- β-hCG (in women of childbearing age) - in women
- Troponins - heart
- Lactate - tissue perfusion
KEY TESTS FOR OR PREPARATION
- CBC, electrolytes, creatinine, glucose
- INR/PTT
- CXR (if history of cardiac or pulmonary disease)
- ECG if clinically indicated by history or if >69 years and no risk factors
Laboratory TestsY
The investigations in all cases of the acute abdomen share the same generic outline:
- Urine dipstick – for signs of infection or haematuria ±MC&S. Include a pregnancy test for all women of reproductive age.
- ABG – useful in bleeding or septic patients, especially for the pH, pO2, pCO2, and lactate for signs of tissue hypoperfusion, as well as a rapid hemoglobin.
- Routine bloods – FBC, U&Es, Liver Function, CRP, amylase.
- Consider measuring serum calcium in suspected pancreatitis.
- Do not forget a group & save (G&S) if the patient is likely to need surgery soon.
- Blood cultures – if considering infection as a potential diagnosis
- Note: Any amylase / lipase 3x greater than the upper limit is diagnostic of pancreatitis. Any raised value lower than this may also be due to another pathology, such as perforated bowel, ectopic pregnancy, or diabetic ketoacidosis (DKA)
Investigation:
Imaging In the emergency setting, every patient with abdominal pain should have an ECG to exclude myocardial infarction. Other imaging modalities that may be initially requested include:
Ultrasound:
- Kidneys, ureters and bladder (‘KUB’) – for suspected renal tract pathology
- Biliary tree and liver – for suspected gallstone disease
- Ovaries, fallopian tubes and uterus – for suspected tubo-ovarian pathology
Radiological:
- An erect chest X-ray (eCXR) – for evidence of bowel perforation.
- CT imaging, depending on the suspected underlying diagnosis
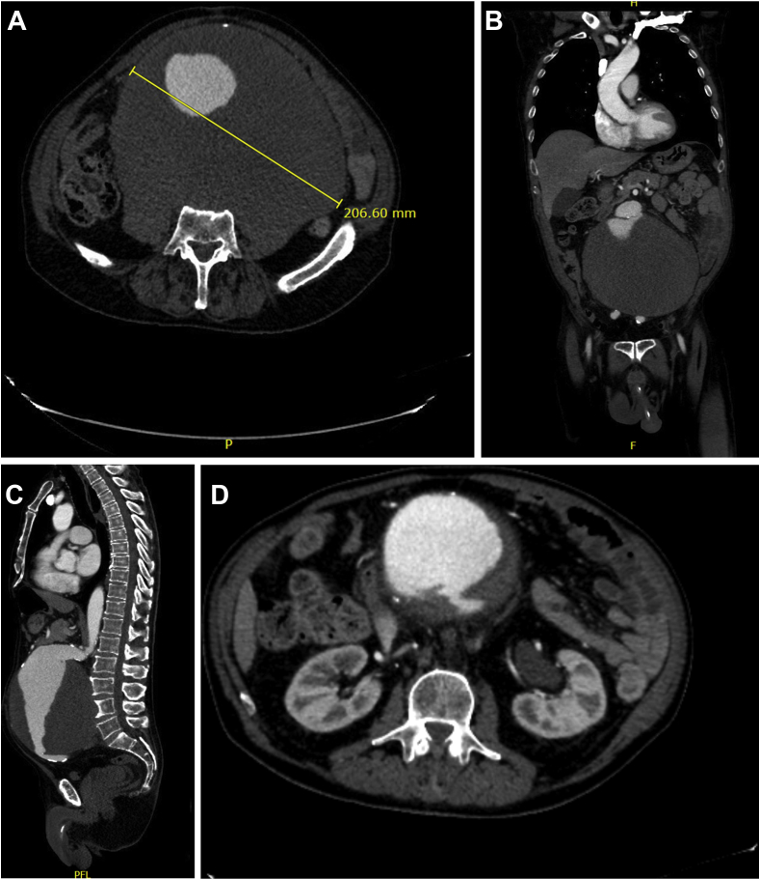 D- Aortic Aneurysm
D- Aortic Aneurysm
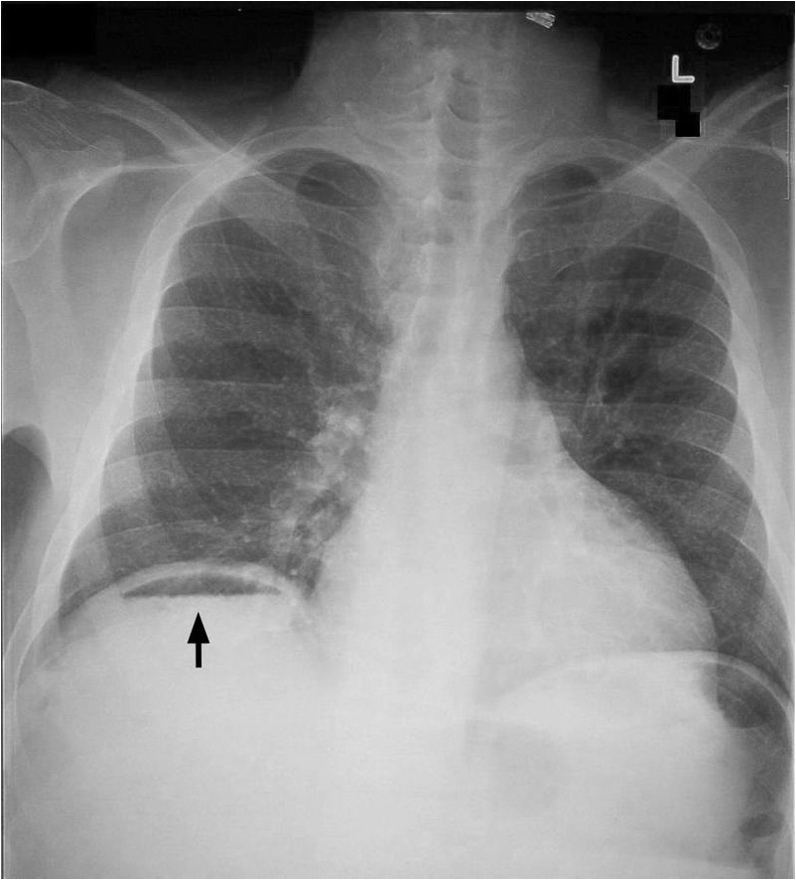 Perforation - air - can be found normally after surgery
Perforation - air - can be found normally after surgery
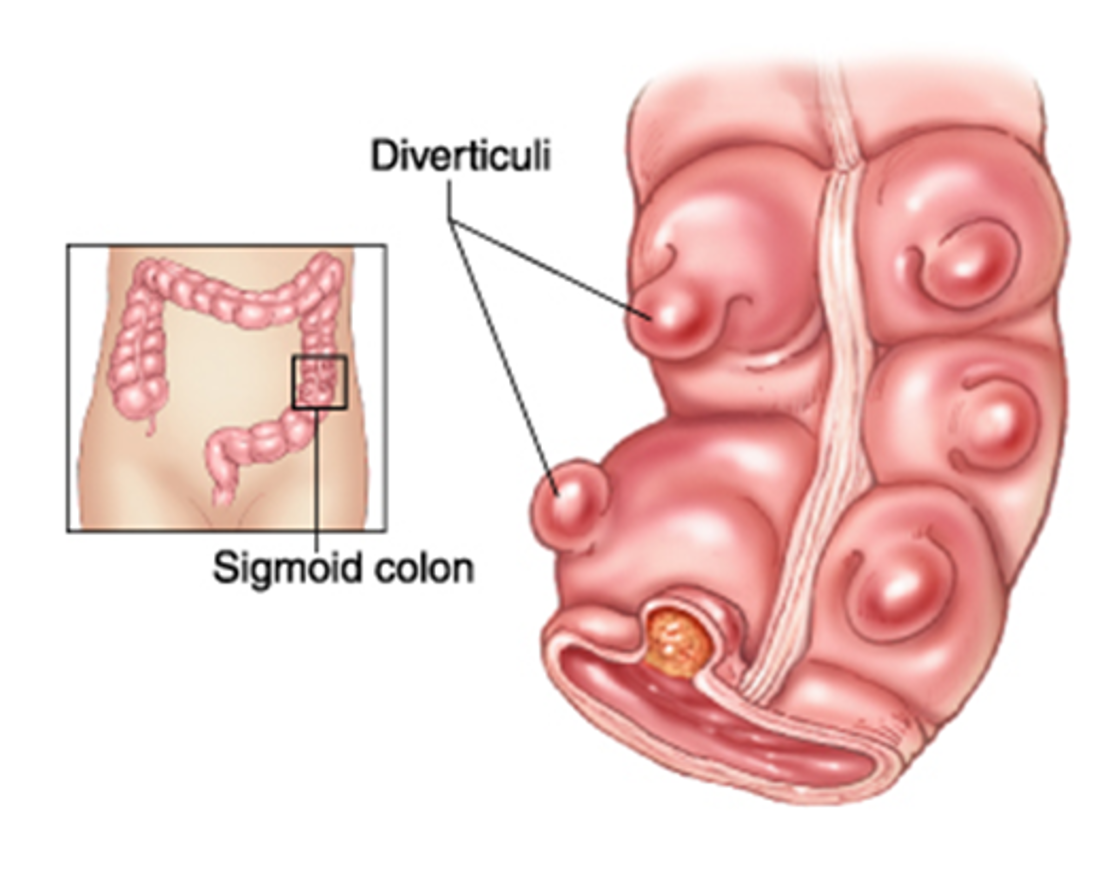
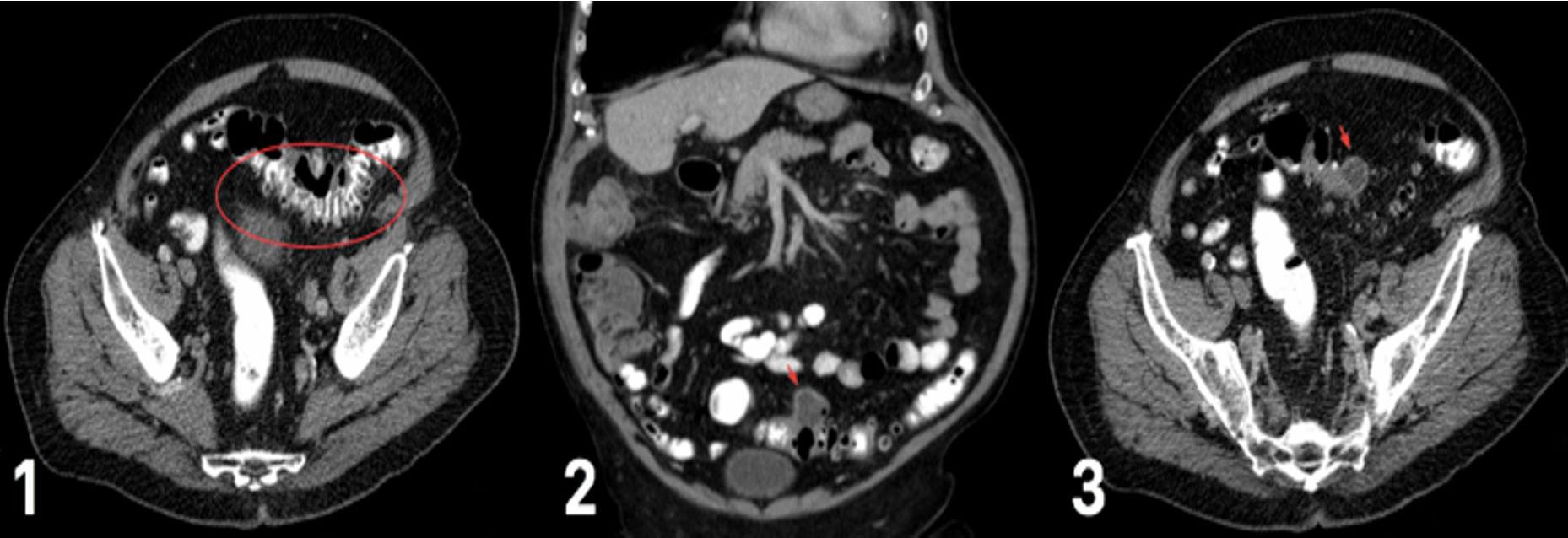 CT scan for varying degrees of diverticular disease (1) diverticulum in the sigmoid colon (2) degree of diverticulitis present (3) abscess formation, secondary to ongoing diverticulitis
CT scan for varying degrees of diverticular disease (1) diverticulum in the sigmoid colon (2) degree of diverticulitis present (3) abscess formation, secondary to ongoing diverticulitis
Left Iliac Fossa Pain;
Male or female ? D/D Diverticular diseases: Presentation ?
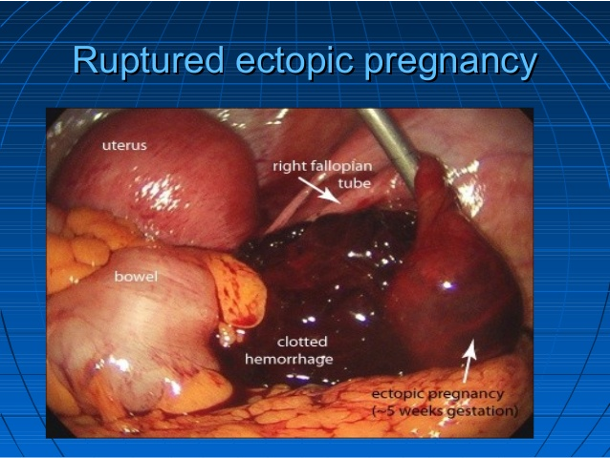 Ruptured Ectopic Pregnancy
Ruptured Ectopic Pregnancy
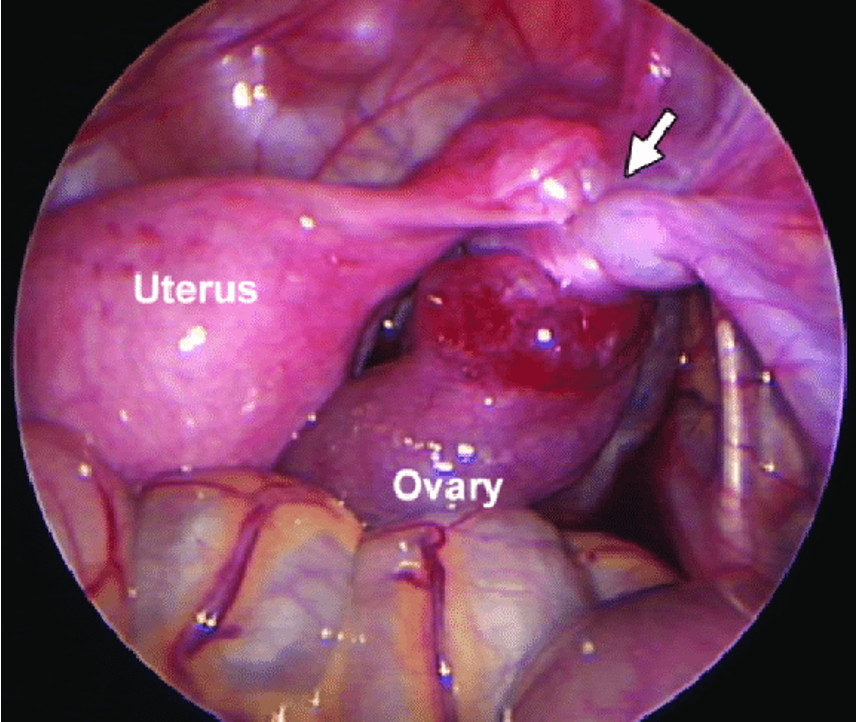 Laproscope
Laproscope
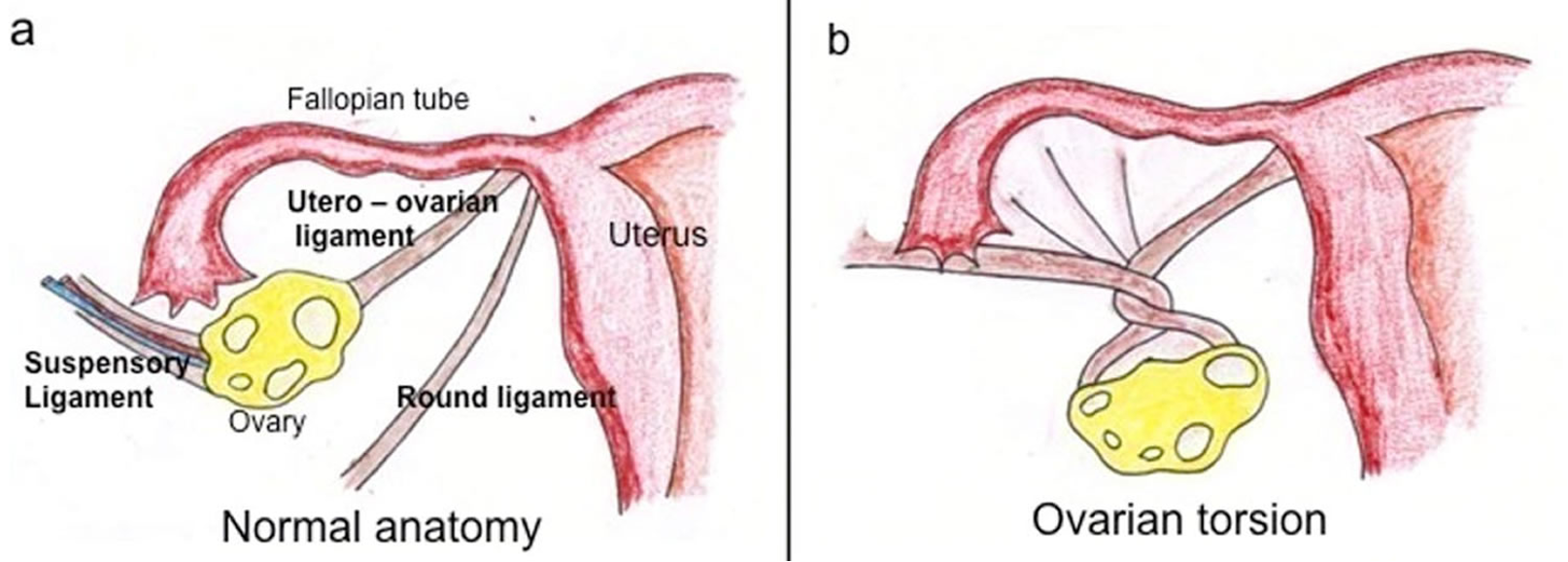 Twiset ovary torsion
Twiset ovary torsion
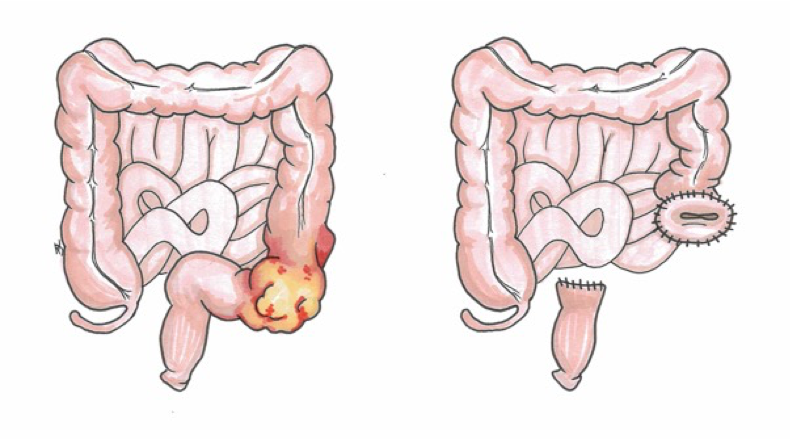
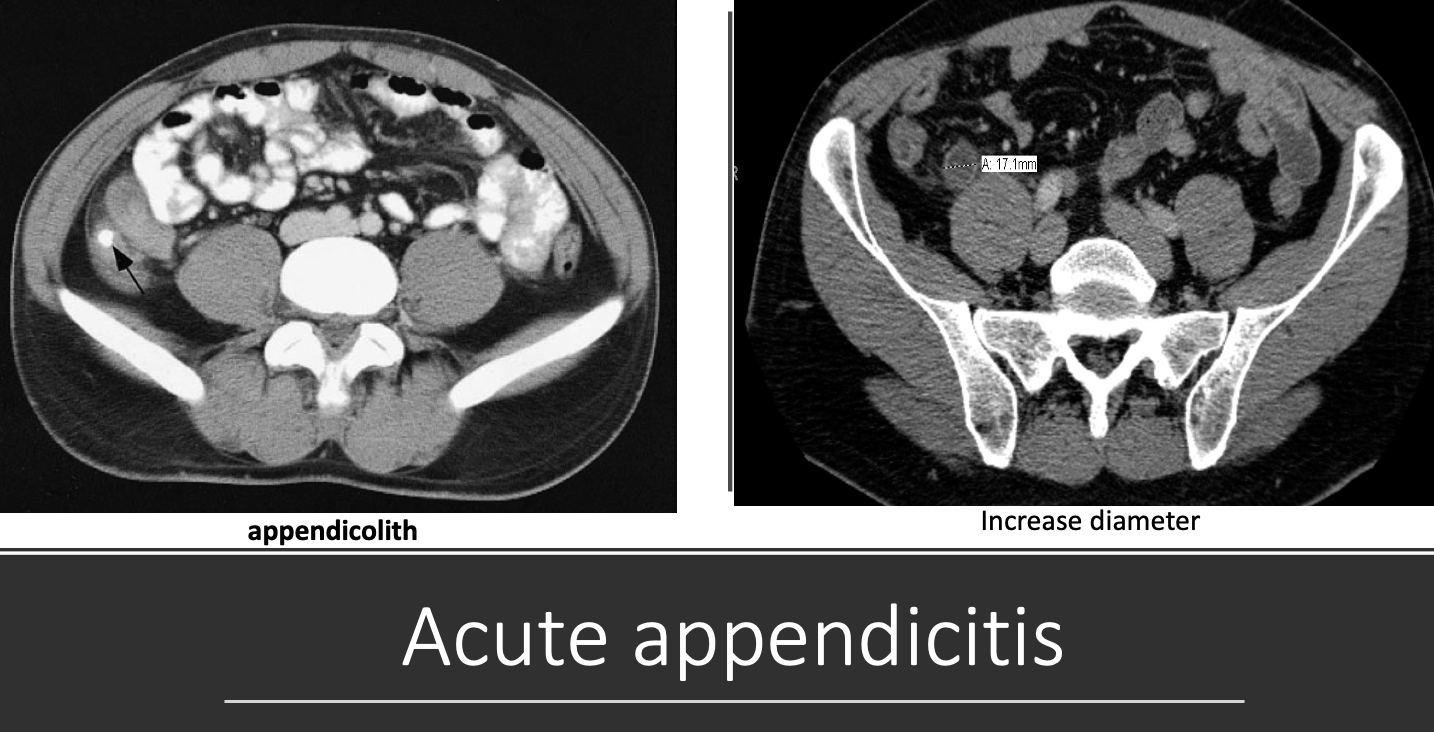 Acute Appendicitis
retrocecal sign obturator??
Acute Appendicitis
retrocecal sign obturator??
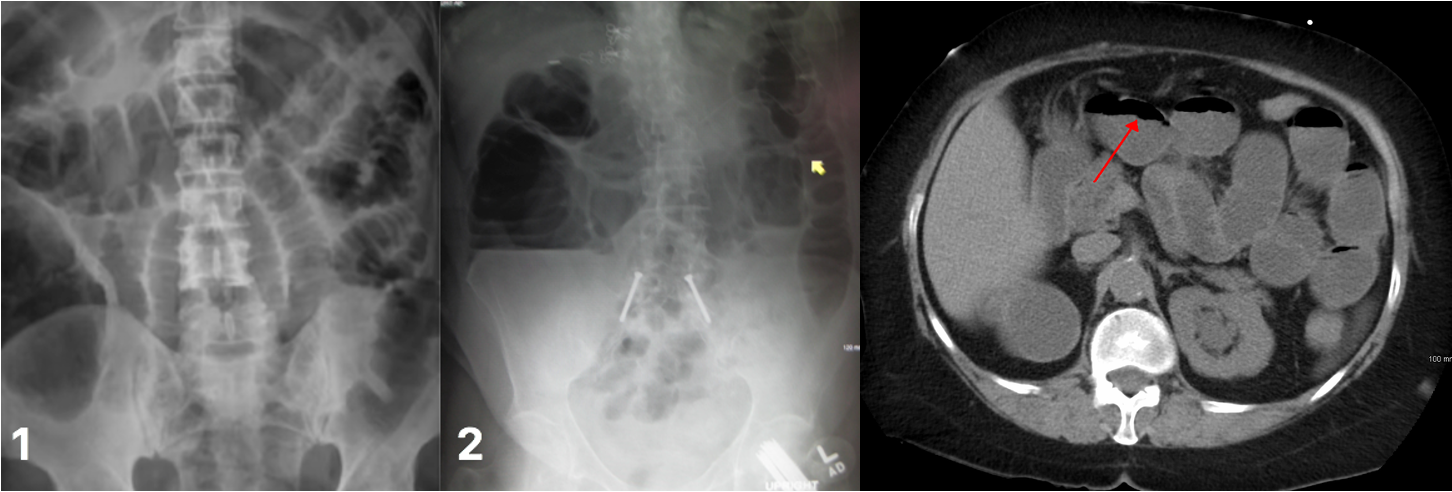 Bowel obstruciton
three view
Bowel obstruciton
three view
 SIgmoid colon tumour
SIgmoid colon tumour