Pediatrics
Acute Otitis Media
Acute ear infection occurs with up to 30 percent of URIs.
Infants and young children are prone to acute otitis media, most common at 6-12 months of age (horizontal and short tube)
Etiology:
-
Bacteria are the most common pathogens in OM, most frequently as a co-infection with viruses.
-
Viruses can be the sole pathogen in OM, but this is less common (<20%).
-
Bacteria including Streptococcus pneumoniae, non-typeable Haemophilus influenzae, and Moraxella catarrhalis.
Clinical Picture
In infants: fever, irritability, and poor feeding.
In older children and adolescents:
- AOM usually is associated with fever and otalgia (acute ear pain).
- AOM also may present with otorrhea (ear drainage) after spontaneous rupture of the tympanic membrane.
- Signs of a common cold, which predisposes to AOM, are often present.
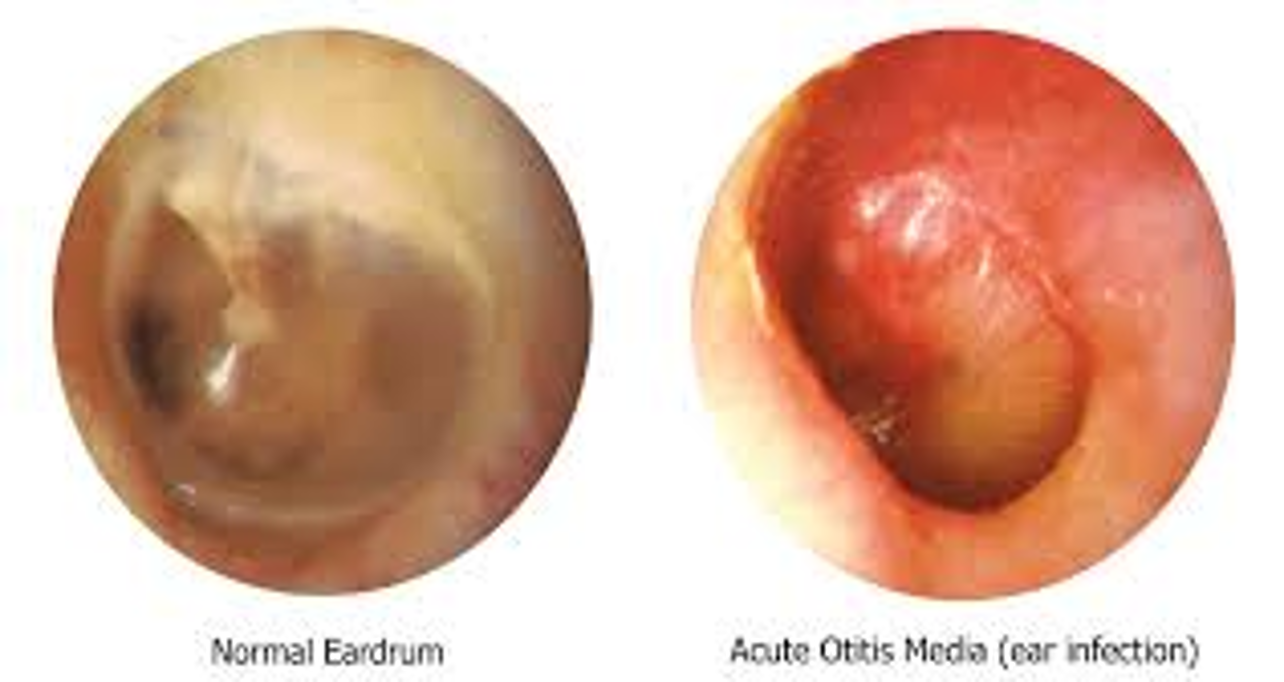
- A bulging tympanic membrane, air fluid level, or visualization of purulent material by otoscopy are reliable signs of infection.
- Examination of the ears is essential for diagnosis.
- The hallmark of OM is the presence of effusion in the middle ear.
Diagnosis
Diagnostic action statements from the AAP guidelines include the following:
-
AOM should be diagnosed when there is moderate to severe tympanic membrane bulging or new-onset otorrhea not caused by acute otitis externa.
-
AOM may be diagnosed from mild tympanic membrane bulging and ear pain for less than 48 hours or from intense tympanic membrane erythema; in a nonverbal child, ear holding, tugging, or rubbing suggests ear pain.
-
AOM should not be diagnosed when pneumatic otoscopy and/or tympanometry do not show middle ear effusion.
Tympanic Membrane Examination:
- Bright red, bulging, loss of light reflection.
Complications:
-
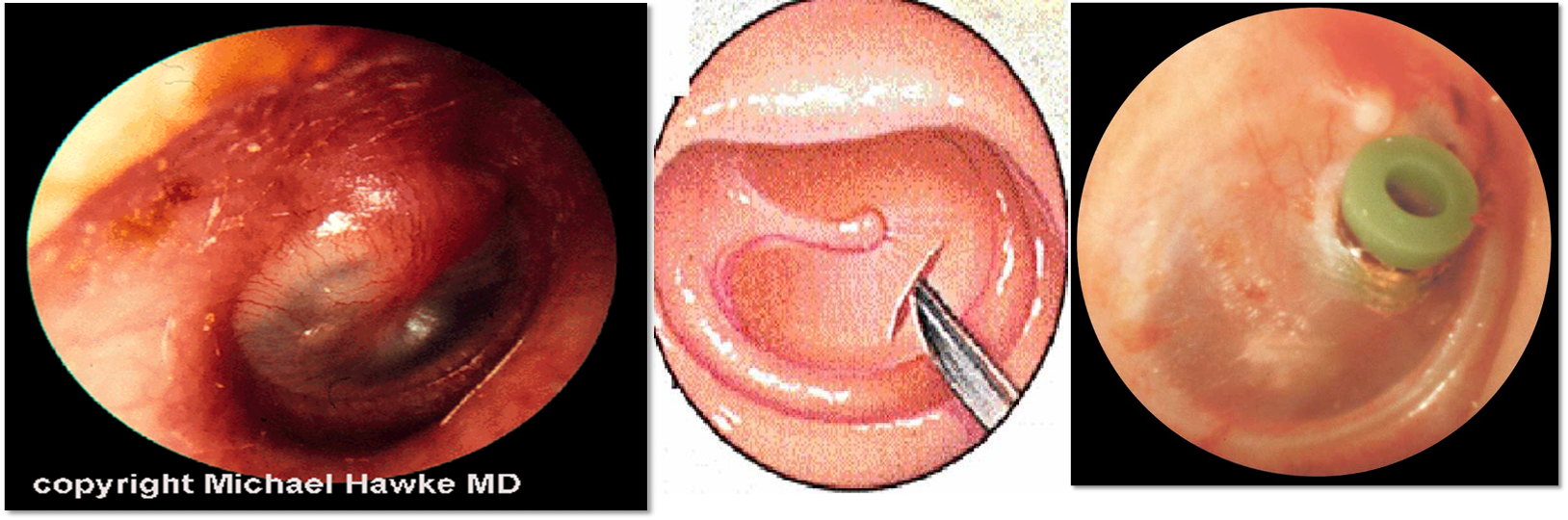
It may lead to perforated eardrums and chronic ear discharge in later childhood and ultimately to hearing impairment or deafness.
-
Mastoiditis and meningitis (STAT admission & surgery), but uncommon.
-
Chronic ear infection following repeated episodes of acute ear infection is common in developing countries, affecting 2 to 6 percent of school-age children.
-
The associated hearing loss may be disabling and may affect learning.
-
Recurrent ear infections can lead to otitis media with effusion (OME or glue ear or serous otitis media).
Treatment:
-
Regular analgesic e.g. Paracetamol, ibuprofen. (every hour to reduce inflammation)
-
The recommended first-line therapy for most children meeting the criteria for antibiotic therapy is amoxicillin (80–90 mg/kg/day in two divided doses).
-
Some children with mild illness or uncertain diagnosis may be observed if appropriate follow-up within 48–72 hours can be arranged with the initiation of antibiotic therapy if symptoms do not self-resolve.
-
Treatment of complications e.g. grommets insertion.


ENT
Acute Otitis Media
Definition:
- Acute infection (<3 weeks) of the middle ear space.
Pathophysiology:
- Eustachian tube dysfunction.
Pathogens:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis
Presentation of Acute Otitis Media
- Symptoms: Fever, earache, ear fullness, hearing loss.
- In Children: Ear itching and pulling.
- Otoscopy Examination (OE): Hyperemic tympanic membrane (TM), fluid in the middle ear (bulging TM, air-fluid levels or bubbles).
- Tests: Pure Tone Audiometry (PTA), Tympanometry.
Management of Acute Otitis Media
- Medications: Antibiotics, analgesia, nasal decongestants.
- Surgical Intervention: Myringotomy with or without ventilation tube insertion.
Management Based on Age and Severity:
| Age | Mild: fever < 102, Pain < 48 hrs | Severe: fever > 102, pain > 48 hrs |
|---|---|---|
| < 6 mos | Antibiotics and analgesics | Antibiotics and analgesics |
| 6-23 mos | Analgesia and Recheck 24-48hrs Unilateral | Antibiotics and analgesics Bilateral or Severe |
| > 2 yrs | Analgesia and Recheck 24-72hrs | Antibiotics and analgesics |