IM
- Diagnosis is mainly clinical based on history and examination
- Supportive evidence is provided by
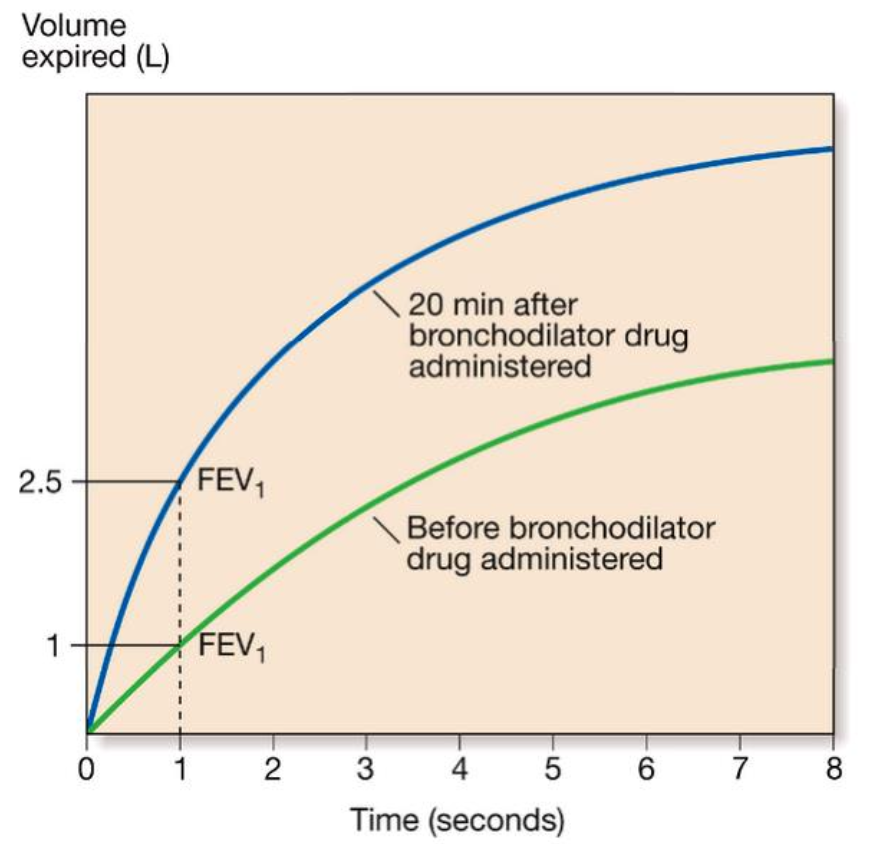
- Spirometry - FEV₁ is reduced than normal and there is > 15% increase in FEV1 following administration of broncho dilator
Reversibility Test
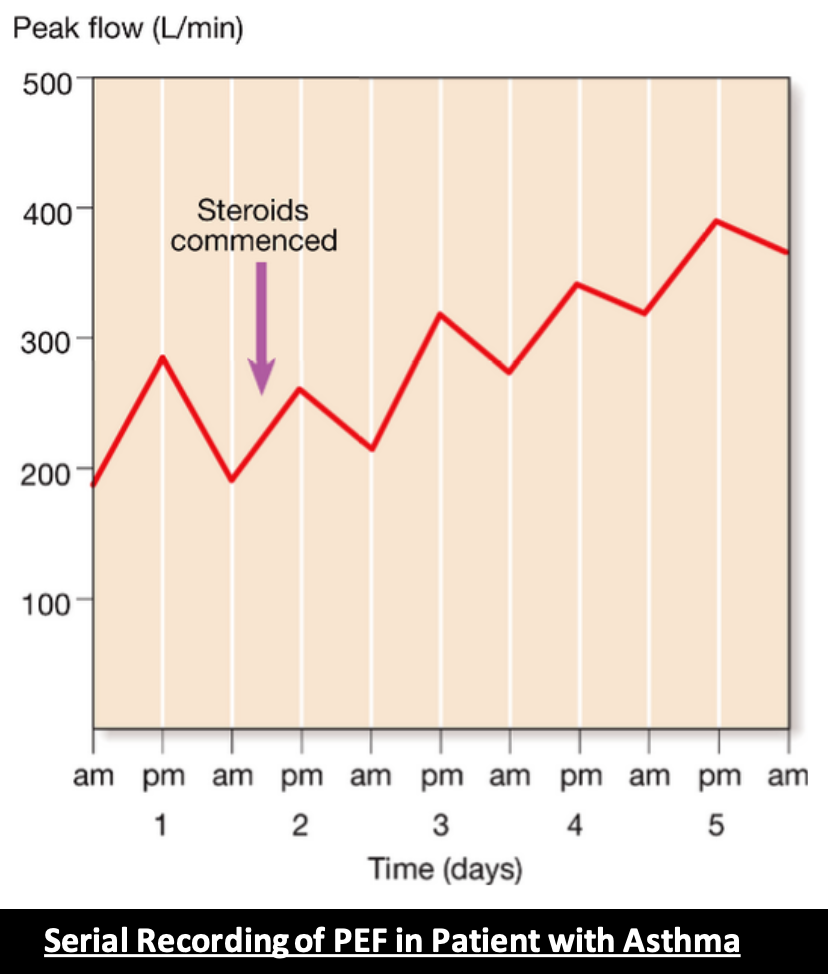
2- Peak Flow Meter at Home
- Patients are advised to record peak flow reading after arising in the morning and before retiring in the evening
- PEF (Peak Expiratory Flow) if reduced more than 20% in the morning is considered diagnostic of bronchial asthma
Peak Flow Meter
Other useful test
- Allergic status - skin prick test
- IgE measurement
- Blood CBC - may show increase Eosinophil count,
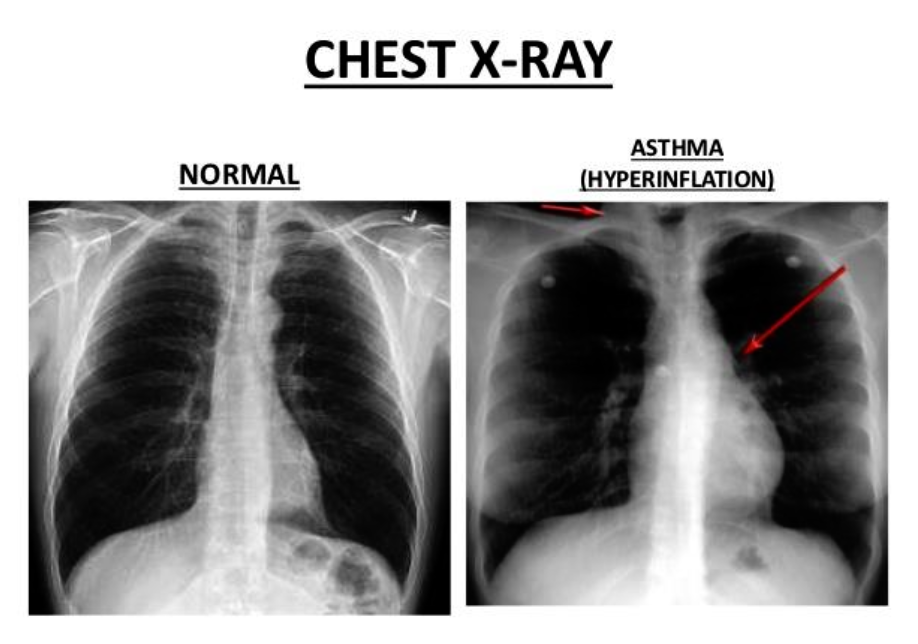
- Radiological examination - normal or hyperinflation of lung fields
Chest X-Ray
FM
Diagnosis of Asthma in Adults and Adolescents
Signs and Symptoms
- Cough
- Wheezing
- Chest tightness
- Shortness of breath
History
- Family history of asthma or other atopic conditions?
- Any recurrent attacks of wheezing?
- Does the patient have a troublesome cough at night?
- Does the patient wheeze or cough after exercise?
- Does the patient experience symptoms after exposure to any of the triggers?
- Is there worsening of symptoms after taking the causative medications?
- Does the patient’s cold “go to the chest” or take more than 10 days to clear up?
- Are symptoms improved by appropriate asthma treatment?
- Are there any features suggestive of occupational asthma?
Physical Examination
- May be normal in stable and controlled asthma
- Bilateral expiratory wheezing
- Examination of the upper airways
- Other allergic manifestations: e.g., atopic dermatitis/eczema
- Consider alternative diagnosis when there is localized wheeze, crackles, stridor, clubbing or heart murmurs.
Classification of Asthma Severity Y
Clinical Features Before Treatment
| Symptoms | Nocturnal Symptoms | FEV₁ or PEF |
|---|---|---|
| STEP 4 Severe Persistent | Frequent | < 60% predicted Variability > 30% |
| STEP 3 Moderate Persistent | > 1 time a week | 60 to 80% predicted Variability > 30% |
| STEP 2 Mild Persistent | > 2 times a month | > 80% predicted Variability 20 to 30% |
| STEP 1 Intermittent | < 2 times a month | > 80% predicted Variability < 20% |
Thera
Asthma Diagnosis
- History and patterns of symptoms
- Measurements of lung function
- Spirometry
- Peak expiratory flow
- Measurement of airway responsiveness
- Measurements of allergic status to identify risk factors
- Extra measures may be required to diagnose asthma in children 5 years and younger and the elderly
Classification of bronchial asthma: T
A. According to aetiology:
-
Extrinsic asthma (allergic): It is due to allergy to antigenic substances in the inspired air e.g. pollens, animal feather, drugs, or home dust mite.
-
Intrinsic asthma (non-allergic): bronchospasm can be evoked by internal causes. It is common above 40 years and have bad prognosis. B. According to clinical severity:
-
Mild asthma: patient has bronchoconstrictive episodes <2 times/week and is asymptomatic between attacks.
-
Moderate asthma: patient has bronchoconstrictive episodes >2 times/week and symptoms requiring inhaled beta agonists daily.
-
Severe asthma: patient has continuous symptoms, Hospitalization may be required. C. According to clinical presentation:
-
Acute asthma.
-
Chronic asthma.
-
Acute Severe Asthma (status asthmaticus): is a condition in which bronchodilators are ineffective in relieving the attack after 24 hrs.
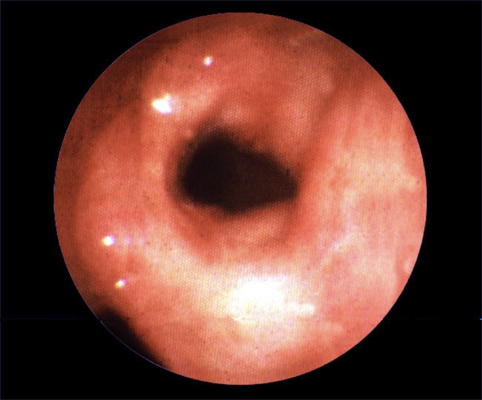
Bronchoconstriction -
provacitive test - methacholine stimulation to assess if patient is Asthmatic - usually 10 minutes after exposure there would be complete obstruction
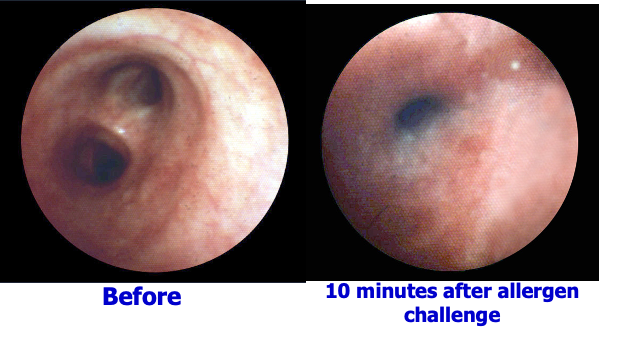
Airway mucosal oedema