Internal Medicine
Therapeutics
Ischemic heart disease is a condition in which there is imbalance between O2 supply (coronary blood flow) and O2 demand (heart work).
- Angina pectoris: Pain or discomfort in the chest caused by insufficient blood flow to the heart muscle.
- Atherosclerosis
- (Coronary Artery Diseases):…
Myocardial metabolism:
- 60% of the myocardial energy comes from aerobic oxidation of fatty acids (gives more energy but utilizes more O2).
- 35% of the myocardial energy comes from aerobic oxidation of carbohydrates (gives less energy but utilizes less O2).
- 5% of energy comes from oxidation of amino acids, ketone bodies, etc.
Pathophysiology:
- Myocardial ischemia is caused by an imbalance between myocardial oxygen supply and oxygen demand.
- Severe coronary narrowing and myocardial ischemia are frequently accompanied by the development of collateral vessels, especially when narrowing develops gradually.
Effects of ischemia:
It causes transient disturbances of the mechanical, biochemical and electrical function of the myocardium.
-
Mechanical: transient left ventricular failure, mitral regurge if papillary muscles are involved.
-
Biochemical: with severe oxygen deprivation, glucose is broken down to lactate and fatty acids can not be oxidized.
-
Electrical: ventricular tachyarrhythmias.
Risk factors for coronary atherosclerosis:
- Age: men > 45y, women> 55y.
- Family history of premature coronary heart disease (CHO).
- Cigarette smoking.
- Hypertension.
- Diabetes mellitus.
- Dyslipidemia.
- Obesity.
Evaluation and Diagnosis
─In patients presenting with chest pain
- Detailed history
- focused physical examination
- directed risk-factor assessment
─Estimate the probability of significant CAD (i.e., low, intermediate, high)
Symptoms
Pain: usually builds up rapidly within 30 seconds and disappears in decrescendo within 5 to 15 minutes. Fleeting or long-lasting discomfort is rarely angina
Character: variably described but typically presents as tightness, squeezing or constriction. Some patients describe an ache, a feeling of dull discomfort, indigestion, or burning pain. (the clenching of the fist over the sternum while describing the pain is classic)=“grip-like,” “pressure-like,” “suffocating” and “heavy”; or a “discomfort” but not “pain.” Angina is almost NEVER sharp or stabbing, and NOT change with position or respiration.
Site: retrosternal. It can be precordial
Radiation: left shoulder, left arm, back, neck, jaw, teeth, back and rarely epigastrium. If above the mandible, below the epigastrium, or localized to a small area over chest wall is rarely anginal.
Precipitating factors: exertion, emotion, and sexual activity.
Relieving factor: rest, and sublingual nitroglycerin usually within 30 secs to several mins.
Nocturnal angina: occurring during sleep.
Postprandial angina: develops after meals (because of an increased oxygen demand in splanchnic vascular bed)
Angina equivalents: No chest pain, instead dyspnea, dizziness, fatigue or faintness, more in diabetics. When these symptoms occur in response to exercise or stress, patients must be evaluated for possible myocardial ischemia.
Signs: Examination is often normal, there may be signs of risk factors .
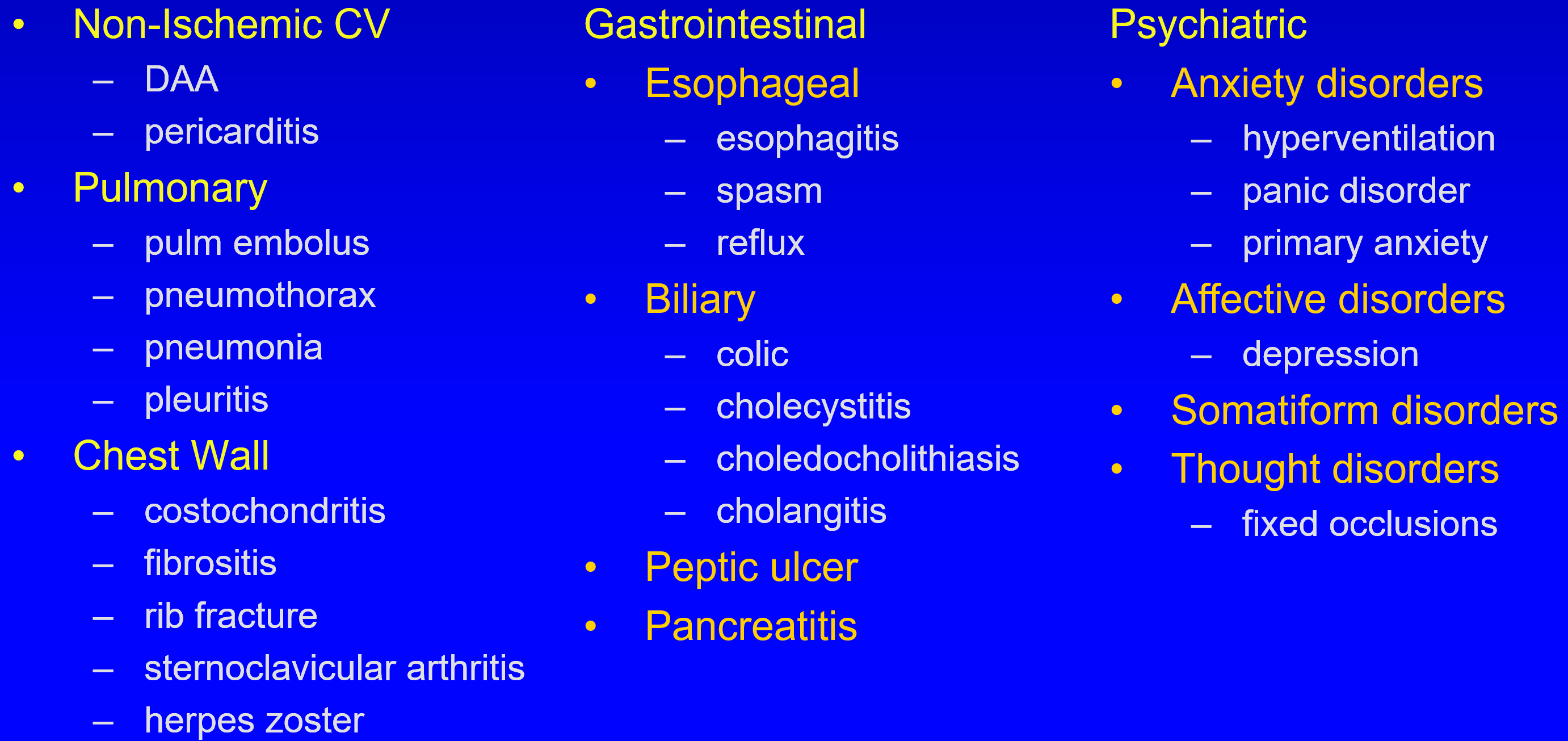
DD of Chest Pain
Conditions Provoking or Exacerbating Ischemia
Increased Oxygen Demand
- Cardiac: HTN, AS / HCM, SVT / VT
- Non-Cardiac: Hyperthermia, Hyperthyroidism, Sympathomimetic toxicity (cocaine use), Anxiety
Decreased Oxygen Supply
- Anemia
- Hypoxemia; COPD, PH,
- Sickle-cell disease
- Hyperviscosity; polycythemia, leukemia, thrombocytosis, hypergammaglobulinemia
Investigations:
1. ECG: Inbetween the attacks: the ECG may be completely free (so we can’t depend on ECG only for diagnosis). It is normal in 50% of cases, but does not exclude the diagnosis. - which is not conclusive
During ischemia: there is ST segment depression and T-wave inversion and may be ventricular tachyarrhythmias. In myocardial infarction: there is deep Q-wave.
*Continuous 24-hour ECG recording (Holter monitoring).
Provocative testing: Angina with normal resting ECG, the provocative testing can confirm the presence of ischemia,
Stress ECG: Treadmill”:
- Recording the 12-lead ECG before, during and after exercise. the physician should be present throughout the test. The test is discontinued upon evidence of:
- Chest discomfort, severe dyspnea, dizziness, fatigue, fall in systolic B.P. > I 0 mmHg., ST segment depression of greater than 0.2 mV, or ventricular tachyarrhythmias
- NB: The normal response to exercise includes a progressive increase in heart rate and blood pressure.
2. Stress echocardiography: After I. V. dobutamine (pharmacological challenge) or exercise shows areas of regional wall motion abnormality (akinesia) in the left ventricle due to persistent ischemia or MI.
-
Multislice CT coronary angiography: is emerging as the most reliable noninvasive method for coronary artery disease assessment, detection of coronary plaques and significant obstructive coronary lesions.
-
Positron emission tomography (PET) (with exercise or pharmacologic stress).
-
Indications: ─for assessing perfusion & ─patients who cannot exercise because of peripheral vascular or musculoskeletal disease ─Intravenous pharmacologic challenge
-
Aim: To create a coronary “steal” by temporarily increasing flow in non-diseased segments of the coronary vasculature at the expense of diseased segments. For example, dipyridamole or adenosine to identify myocardial ischemia and increased risk of coronary events in exertional dyspnea ·The development of a transient perfusion defect with radioactive thallium or 99 mTc to detect myocardial ischemia.
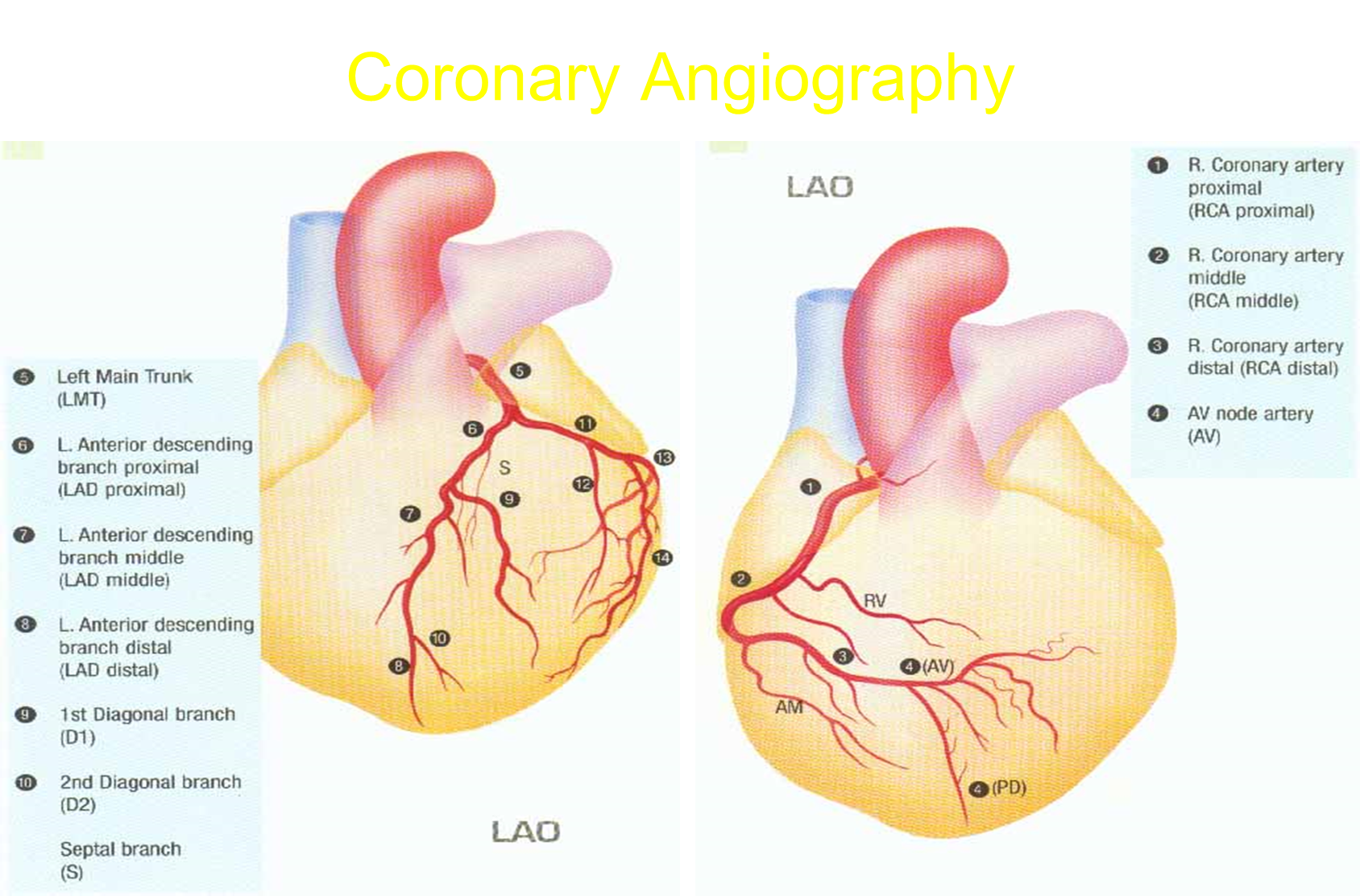
- Coronary angiography: This invasive diagnostic method shows narrowing of coronary artery lumen. It can assess the severity of obstruction. *Indications: *
- Confirm or exclude the diagnosis of ischemia.
- Patients who are severely symptomatic despite medical treatment.
- Severe ischemia as demonstrated in non invasive testing.
- High risk patients, including left ventricular dysfunction.