By Dr. Israa
Important Terms:Z
- Relapse: (P. ovale and P. vivax) Recurrence of disease after it has been apparently cured.
- Reinfection: By different species.
- Recrudescence; recruitment: Insufficient treatment with malarial medication.
Types:Z
| Plasmodium Species | Type / Fever Cycle | Fever Pattern | Additional Notes | RBCs |
|---|---|---|---|---|
| Plasmodium falciparum | Malignant Tertian Malaria 24-48 hours | Irregular, often continuous or remittent fever | Most severe form, can cause cerebral malaria, multi-organ failure. | All stages of RBCs |
| Plasmodium vivax Relapse | Benign Tertian Malaria 48 hours Recurrent | Fever spikes every 48 hours (every third day) | Can cause relapses due to dormant liver stages (hypnozoites). | Reticulocytes (young RBCs) |
| Plasmodium ovale Relapse | Benign Tertian Malaria 48 hours Recurrent | Fever spikes every 48 hours (every third day) | Similar to P. vivax, can also cause relapses due to hypnozoites. | Reticulocytes (young RBCs) |
| Plasmodium malariae | Membranous milaria - Membranous glomerulonephritis = nephrotic Quartan Malaria 72 hours | Fever spikes every 72 hours (every fourth day) | Chronic infection can persist for years, often with low-grade symptoms. | Older RBCs (mature RBCs) |
| Plasmodium knowlesi | Simian malaria Quotidian Malaria 24 hours | Daily fever spikes | Zoonotic malaria, primarily found in Southeast Asia, can be severe. | All stages of RBCs |
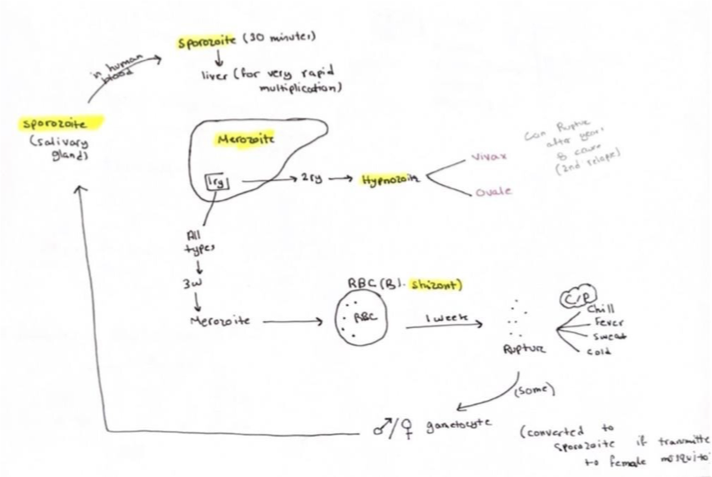
Life Cycle:
There are two stages:
- Sexual (anopheles mosquito; Plasmodium Sporozite ⇒ Hepatocytes)
- Asexual (Liver Hepatocytes; Schizonts ⇒ RBCs; Merozoites (cycled))
Merozoites matures to trophozoites then forming Schizonts
Pathophysiology of Malaria:
Blood film is done to know which type of malaria and choose the proper treatment.
- Anopheles mosquito (carries the plasmodium in her salivary gland)
- Mosquito bite transmits the plasmodium sporozoite (infective stage) into your blood and circulates for 30 minutes to 3 Hours, then enters the liver.
- In the liver:
- The sporozoite enters the hepatocyte to multiply, forming schizonts.
- Schizonts multiply asexually, forming merozoites.
- Within 2 weeks, thousands of merozoites will be formed and rupture the hepatocytes, releasing merozoites into the blood.
- In the blood:
- Merozoites enter erythrocytes and mature into trophozoites.
- Trophozoites develop into schizonts, which multiply asexually, forming thousands of merozoites in RBCs.
- Rupture of RBCs (clinical features begin here); fever rigors sweating
- Released merozoites into the blood:
- Infect other RBCs.
- Stay in blood to become gametocytes.
- Fate of gametocytes:
- Anopheles mosquito sucks your blood again and takes the gametocytes into her intestine.
- Gametocytes multiply sexually, forming sporozoites.
- Mosquito then infects you again with the sporozoite.
hypnozoites? cc
Early and Late Malaria Trophozoite:Z
- Tertian malaria: Periodic fever and spikes every 48 hours / cont 1D (all except . malariae)
- Quartan malaria: Periodic fever spikes every 72 hours / cont 1D (. malariae).
- Malignant tertian malaria: (associated with falciparum malaria): irregular fever spikes without a noticeable rhythm.
Severe Malaria
Definition: Potentially fatal manifestation or complications of malaria.
Most commonly a result of falciparum malaria (higher risk in pregnant women and children).
Infected erythrocytes occlude capillaries, leading to severe organ dysfunction.
Criteria:Z
- CNS: P. Falciparum; Cerebral malaria - cerebral edema - seizures - swollen brain - hallucinations - confusion - loss of consciousness. Cerebral malaria is caused either due to hypoglycemia or occlusion of arteries or capillaries as a result of sticky RBCs. spleen breakdown RBCs, release sticky rbcs ⇒ P>F adherent protien resulting occlusion microcirculation of spleen
- CVS: Heart failure / hb <7 / hemolytic anemia = bilirubin = jaundice
- Pulmonary: Adult Respiratory Distress Syndrome (ARDS).= Acidosis
- Kidney: plasmodium malaria; Acute kidney injury- proteinuria and glomerulonephritis + black water fever (hemoglobinuria).
- GIT: bilious malaria; Jaundice - diarrhea - increased liver enzymes - hepatitis - splenomegaly.
- Others: Severe anemia - acidosis - high fever. circulatory collapse
Diagnosis:
- Blood smear:
- Thin: For the type of parasites.
- Thick: To see the parasites.
- PCR
Treatment:
Uncomplicated:
- Chloroquine persistent: any one of these drugs for prophylaxis
- Artemether + lumefantrine
- OR atovaquone + proguanil
- OR Quinine; synchonism; Prolong Qt interval; + doxycycline; no milk drinker; yellow teeth; no pregnancy; staining bone;
- For vivax or ovale: give PART regimen:
-
- Tafenoquine
- Chloroquine sensitive: Chloroquine *(retinal deposition); visual disturbances *
Complicated:
- IV n
Prophylaxis?:
- Some medications are available but do not use the same medication if infected.
- Chloroquine and Mefloquine are safer in pregnancy.
Vaccine?:
- Mosquirix
Prevention?:
- Avoid exposure to mosquitoes.
- Mosquito control.
| Feature | P. falciparum | P. vivax | P. ovale | P. malariae | P. knowlesi |
|---|---|---|---|---|---|
| Severity | Severe | Moderate | Moderate | Mild | Severe |
| RBC Type Affected | All types of RBCs | Younger RBCs (reticulocytes) | Old RBCs | Old RBCs | Old RBCs |
| Fever Cycle | 48 hours (Malignant tertian malaria) | 48 hours (Tertian malaria) | 48 hours (Tertian malaria) | 72 hours (Quartan malaria) | 24 hours (Quotidian malaria) |
| Relapse | No | Yes (due to hypnozoites) | Yes (due to hypnozoites) | No | No |
| Recrudescence | Yes | Yes | Yes | Yes | Yes |
| Reinfection | Yes | Yes | Yes | Yes | Yes |
| Complications | Cerebral malaria, severe anemia, ARDS, AKI | Splenomegaly, mild anemia | Splenomegaly, mild anemia | Nephrotic syndrome, membranous glomerulonephritis | Severe malaria, similar to P. falciparum |
| Geographical Distribution | Worldwide, especially in Africa | Asia, Latin America | Africa, Asia | Worldwide, especially in Africa | Southeast Asia |
| Treatment | Artemether-lumefantrine, quinine, etc. | Chloroquine, Primaquine (for relapse) | Chloroquine, Primaquine (for relapse) | Chloroquine | Artemether-lumefantrine, quinine, etc. |
| Prophylaxis | Chloroquine, Mefloquine | Chloroquine, Mefloquine | Chloroquine, Mefloquine | Chloroquine, Mefloquine | Chloroquine, Mefloquine |
Differentiating Malaria, Typhoid Fever, and Dengue Fever Clinically
| Feature | Malaria | Typhoid Fever | Dengue Fever |
|---|---|---|---|
| Causative Agent | Plasmodium parasites (P. falciparum, P. vivax, P. ovale, P. malariae) | Salmonella Typhi bacteria | Dengue virus (DENV 1-4) |
| Transmission | Bite of infected Anopheles mosquito | Fecal-oral route (contaminated food/water) | Bite of infected Aedes mosquito |
| Incubation Period | 7-30 days (depending on species) | 6-30 days | 4-10 days |
| Fever Pattern | Classic cyclical pattern (cold, hot, sweating stages) – may not be present in all cases | Sustained high fever (step-ladder pattern) | High fever (biphasic pattern possible) |
| Headache | Common and severe | Present, but usually not severe | Severe frontal headache (retro-orbital pain) |
| Muscle/Joint Pain | Myalgia common | Myalgia possible | Severe myalgia and arthralgia (“breakbone fever”) |
| Gastrointestinal Symptoms | Nausea, vomiting, diarrhea possible | Abdominal pain, constipation or diarrhea, rose spots on abdomen (in some cases) | Nausea, vomiting, abdominal pain possible |
| Other Symptoms | Splenomegaly, hepatomegaly, anemia, jaundice (in severe cases) | Hepatosplenomegaly, relative bradycardia, cough | Rash (maculopapular or petechial), bleeding manifestations (severe cases), lymphadenopathy |
| Lab Findings | Parasites seen on blood smear, positive rapid diagnostic tests | Blood, stool, or urine culture positive for S. Typhi, Widal test (limited value) | Positive dengue IgM/IgG antibodies, NS1 antigen detection, thrombocytopenia, leukopenia |
Lab Findings for Malaria, Typhoid Fever, and Dengue Fever:
KFT (Kidney Function Test)
| Parameter | Malaria | Typhoid Fever | Dengue Fever |
|---|---|---|---|
| Creatinine | May be elevated in severe cases with complications like acute kidney injury | Usually normal, but may be elevated in severe cases with dehydration or kidney involvement | Usually normal, but may be elevated in severe cases with dehydration or kidney involvement |
| BUN (Blood Urea Nitrogen) | May be elevated in severe cases with dehydration or kidney involvement | Usually normal, but may be elevated in severe cases with dehydration or kidney involvement | Usually normal, but may be elevated in severe cases with dehydration or kidney involvement |
LFT (Liver Function Test)
| Parameter | Malaria | Typhoid Fever | Dengue Fever |
|---|---|---|---|
| AST (Aspartate Aminotransferase) | Elevated | Elevated | Elevated, especially in severe cases |
| ALT (Alanine Aminotransferase) | Elevated | Elevated | Elevated, especially in severe cases |
| Bilirubin | Elevated (especially unconjugated) in cases with jaundice | Usually normal or mildly elevated | May be elevated in severe cases |
| Alkaline Phosphatase | May be elevated | May be elevated | May be elevated |
CBC (Complete Blood Count)
| Parameter | Malaria | Typhoid Fever | Dengue Fever |
|---|---|---|---|
| Hemoglobin | Decreased (anemia) | Usually normal or slightly decreased | Usually normal or slightly decreased, but can be significantly lowered in severe cases with bleeding |
| WBC (White Blood Cell Count) | Normal or decreased (may be elevated in early stages) | Normal or decreased (leukopenia) | Decreased (leukopenia), especially in later stages |
| Platelets | Decreased (thrombocytopenia) | Usually normal or slightly decreased | Decreased (thrombocytopenia), often significantly lowered |