Common Adult Injuries Axial Skeleton Pelvis
Prof. Mamoun Kremli
Outline
-
Introduction
- The pelvic ring
- What does a pelvic injury indicate?
-
Emergency assessment & management
- Differentiation between stable & unstable injuries
- Classification and reading x-rays
-
Treatment options
Anatomy
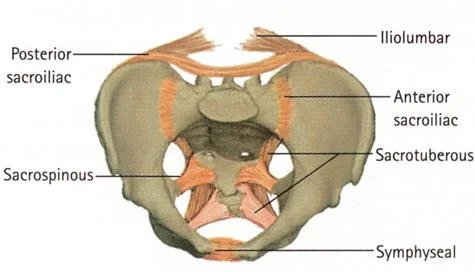
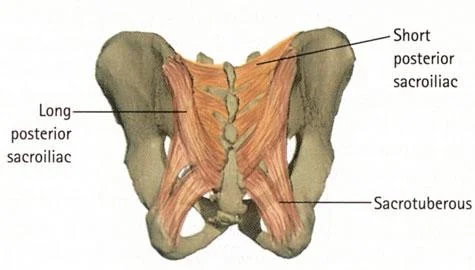
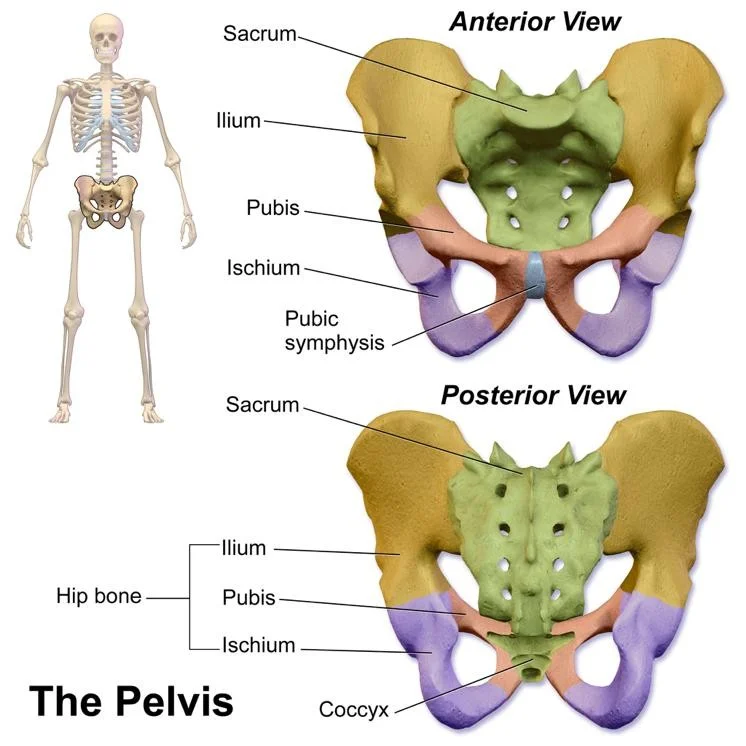
The Pelvic Ring
- Integrity and stability of the pelvic ring is essential

High Energy
- It takes high energy to create such damage



Serious Injury
- Bleeding – up to 3L or more
- Damage to other soft tissues
- Urethra, bladder
- Bowel
- Nerves
- Genitalia
- Rectal sphincter
- Usually with other major fractures / Injuries
Primary Assessment
- Bone is not of primary importance. Life is ! Assessment in suspected pelvic ring fracture is according to ATLS (advanced trauma life support)

Primary Assessment - ATLS

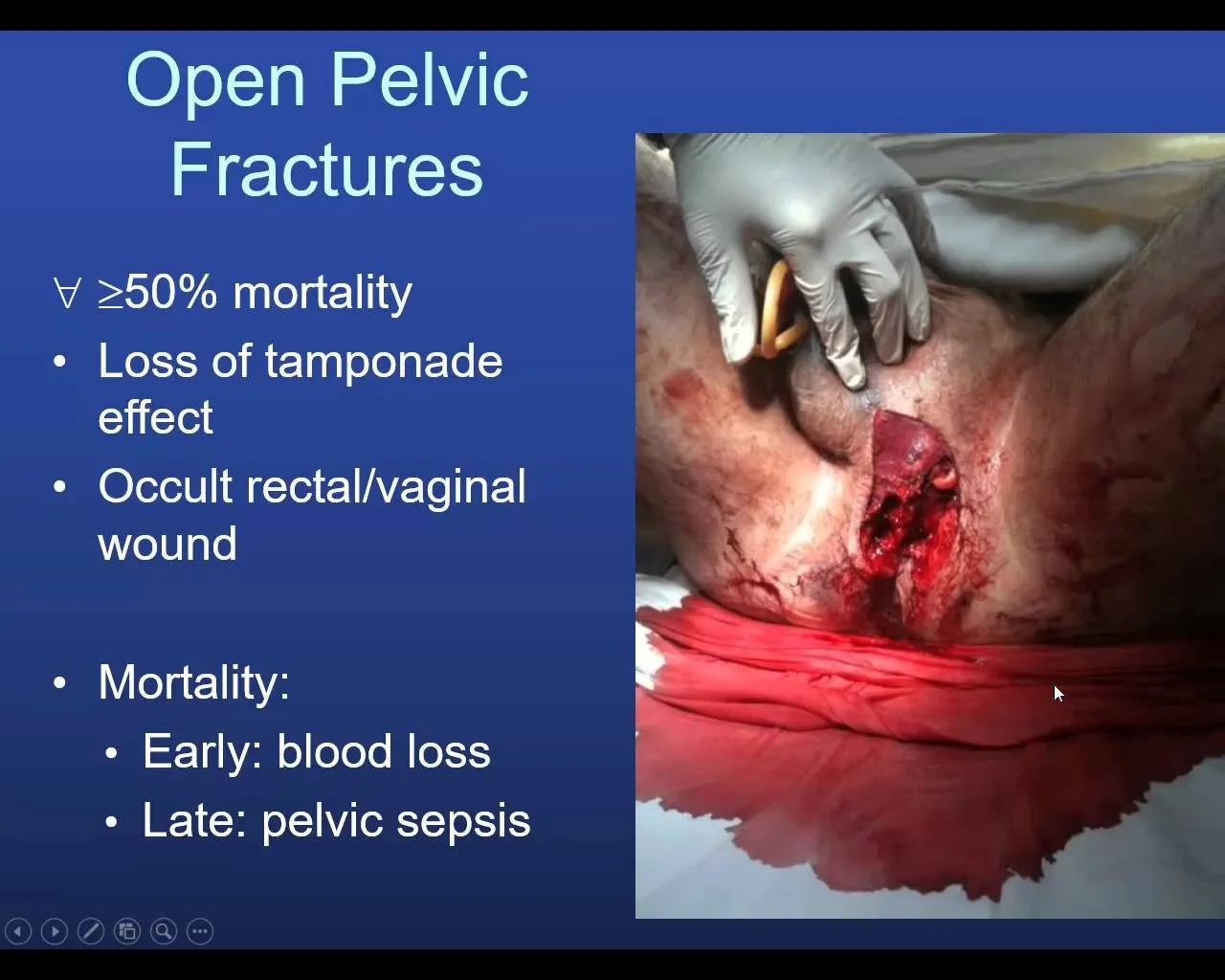
Unstable – Why??
- Exclude other sources
- Open wound — adds risk of sepsis
- Thoracic/abdominal hemorrhage
- Hemothorax
- Hemo-abdomen
- Major fractures
- Long-shaft bone fractures
- Pelvic fracture


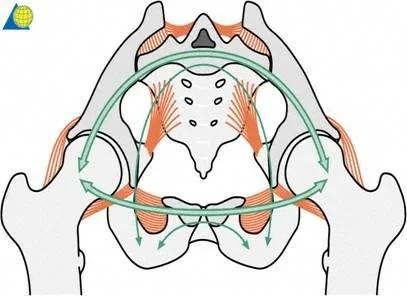
Bleeding from Pelvis
- If the pelvis is the source of bleeding, massive blood loss is:
- Mostly venous 80%,
- Cancellous bone oozing
- posterior disruption
- Supported by enlarged compartment
- Arterial source is rare


Emergency Treatment
- Protect primary blood clot by
- Early pelvic splintage / sheet/ clamp. External fixator and
- Prevention of excessive movement
- Resuscitation
- IV fluids, blood transfusion & fresh frozen plasma, platelets, cryoprecipitate
- For massive transfusions: Ratio of 1:1:1 (PRBC: FFP: Platelets)
- Prevent hypothermia & acidosis
- Stop other bleeding sites(!!)
Bleeding from Pelvis
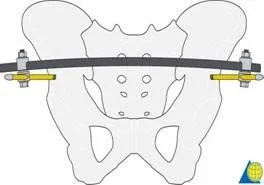
- Emergency treatment: Reduce Compartment
-
Pelvic sheet



-
External fixator


-
Pelvic c- clamp

-
• If the patient still not responding • Think of arterial sources • Either need pelvic packing or embolization by interventional radiologist
Clinical Picture
- Bruising
- Urethral / genital bleeding
- indicates injury to viscera
- Rectal and vaginal examination is mandatory to rule out open fracture
- Do not forget to assess the perineum for wounds




- Tenderness on attempted pressure
- Neurologic exam
- Rule out lumbosacral plexus injuries (L5 and S1 are common)
- Rectal exam to evaluate
- Sphincter tone
- Perirectal sensation

Primary Assessment
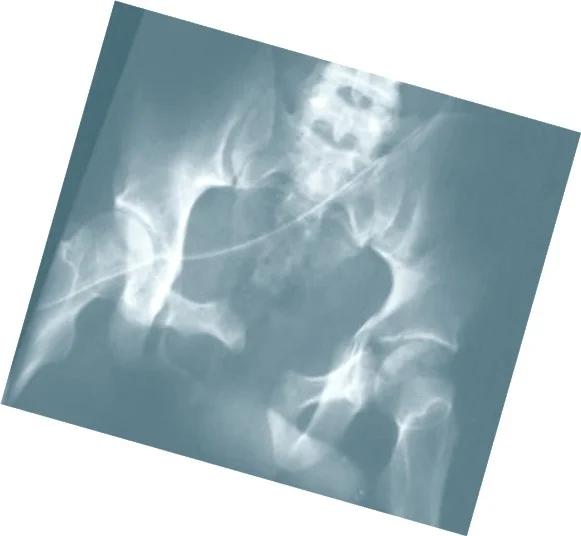
- A standard x-ray reveals up to 90% of fractures

Additional Imaging
- CT scan must be done for pelvis fracture to study condition of posterior ring

Ruptured bladder (urethrogram)

Pelvic Fractures
- Isolated fractures
- Pelvic Ring fractures
Isolated Fractures
- All are Stable
- One bone only
- Or ring on one side
- Avulsion Fractures
- Sudden pull of muscles
- Sartorius: ASIS
- Rectus Femoris: AIIS
- Adductor Longus: Pubis
- Hamstring: Ischium
- Sudden pull of muscles
- Treatment: Rest / analgesics

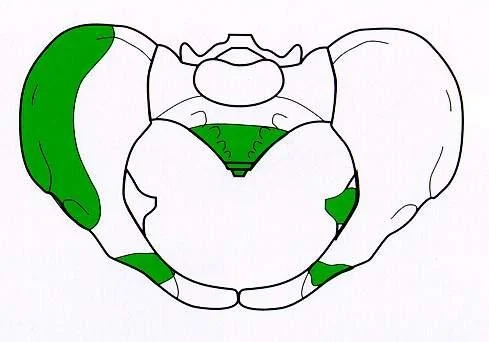

Fractures of Pelvic Ring
In adults, one break in the ring is accompanied by another break in the ring
Three mechanisms:
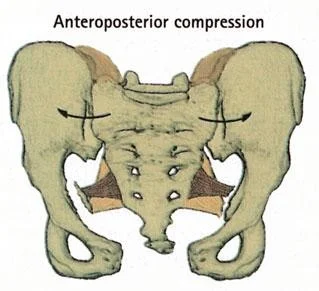
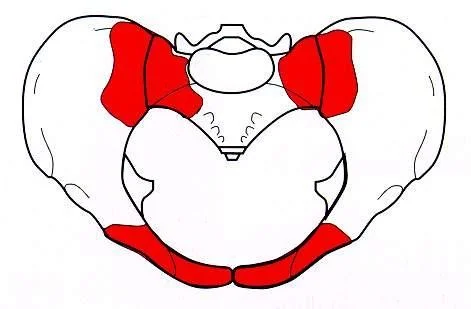
AP compression
- Anteroposterior compression
- Frontal collision of car-pedestrian
- Pubic rami fractured or
- Disruption of symphysis pubis
- Open-book (stable if <2cm)

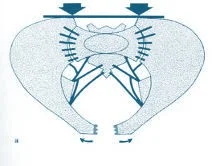

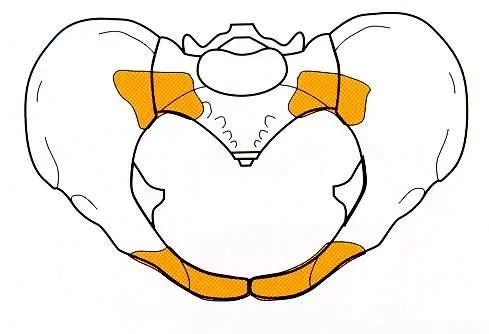
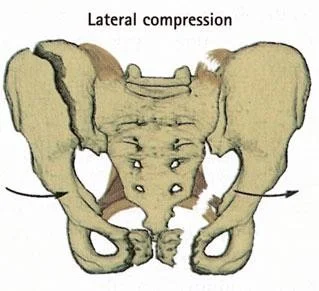
Lateral Compression
- Mechanism:
- Side-on impact in RTA/ fall from height
- Anteriorly:
- Fractured pubic rami
- Posteriorly:
- Sacroiliac strain / fractured ilium & sacrum
- Unstable if severely displaced - needs surgery
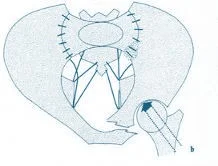
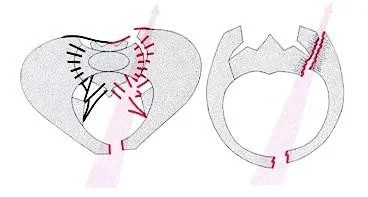
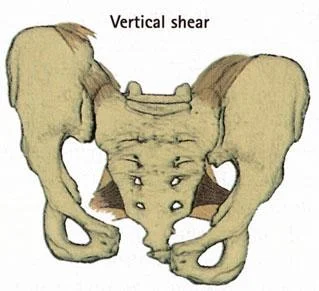
Vertical Shear
- Mechanism:
- Fall from height on one leg
- Innominate bone displaced superiorly on one side
- Fracture of pubic bones
- Disrupted sacroiliac joint on the same side
- Severe, unstable, soft tissue damage, bleeding


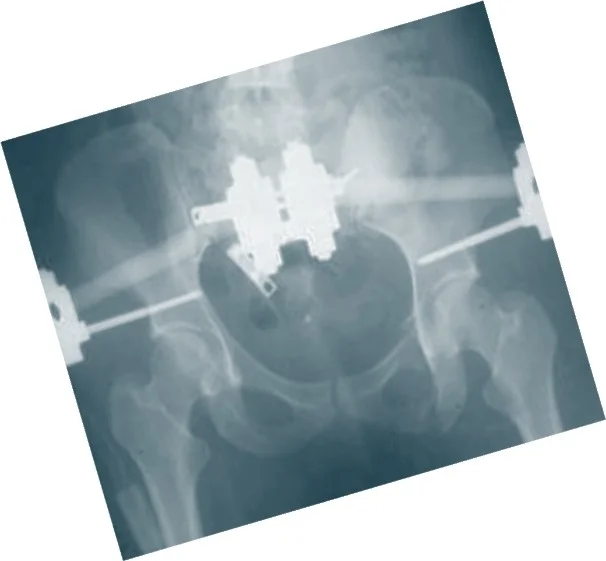
Operative Treatment Options
- External fixation
- Temporary Clamp



-
Internal fixation
- Screws & Plates

- Screws & Plates
-
Combinations
Conclusions
- Pelvic Fractures – Emergency management
- More than just a bony injury
- Suspect high energy trauma
- First, save patient’s life
- If unstable: Stabilization of paramount importance
- Many might be treated nonoperatively