Esophageal varices may be:
- -silent
- -repeated insidious hemorrhage leading to iron deficiency anaemia.
- -sudden rupture either : (From within due to sudden increase in portal venous pressure by cough, exercise, or straining) OR erosion from esophegitis due to ( NSAID-hard food or peptic ulcer).
Here patient manifested by bright red blood not stopped spontaneously because of negative intrathoracic pressure which keep veins patent It can be diagnosed by endoscopy and barium swallow.
Other Varices
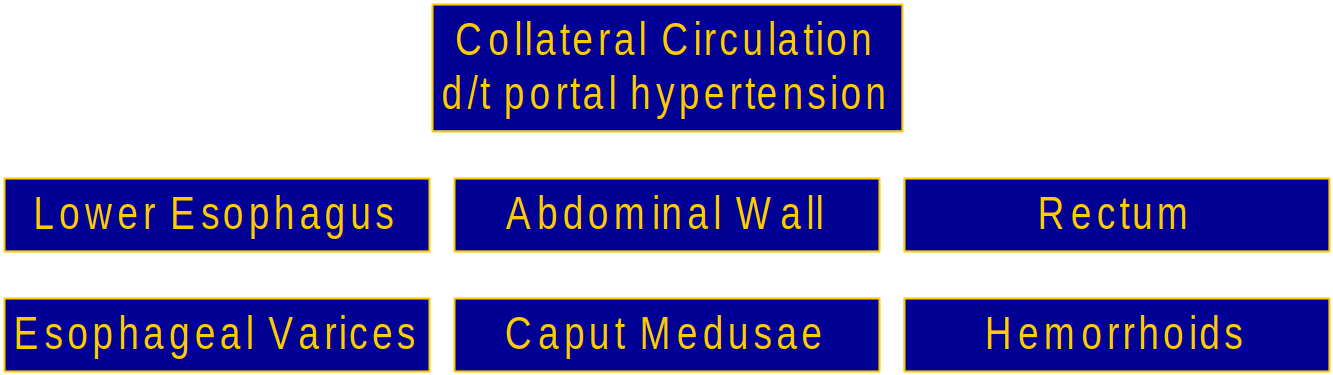
Complications: Esophageal & Gastric Varices:
Esophageal: Complex of twisting veins at lower end of esophagus and upper portion of stomach
Most life threatening complication!! The varices can rupture in 1/3 cases and can lead to death in 50% cases.
Clinical Feature :
- Melena (black color stools)
- Hematemesis
- Hypovolemic shock
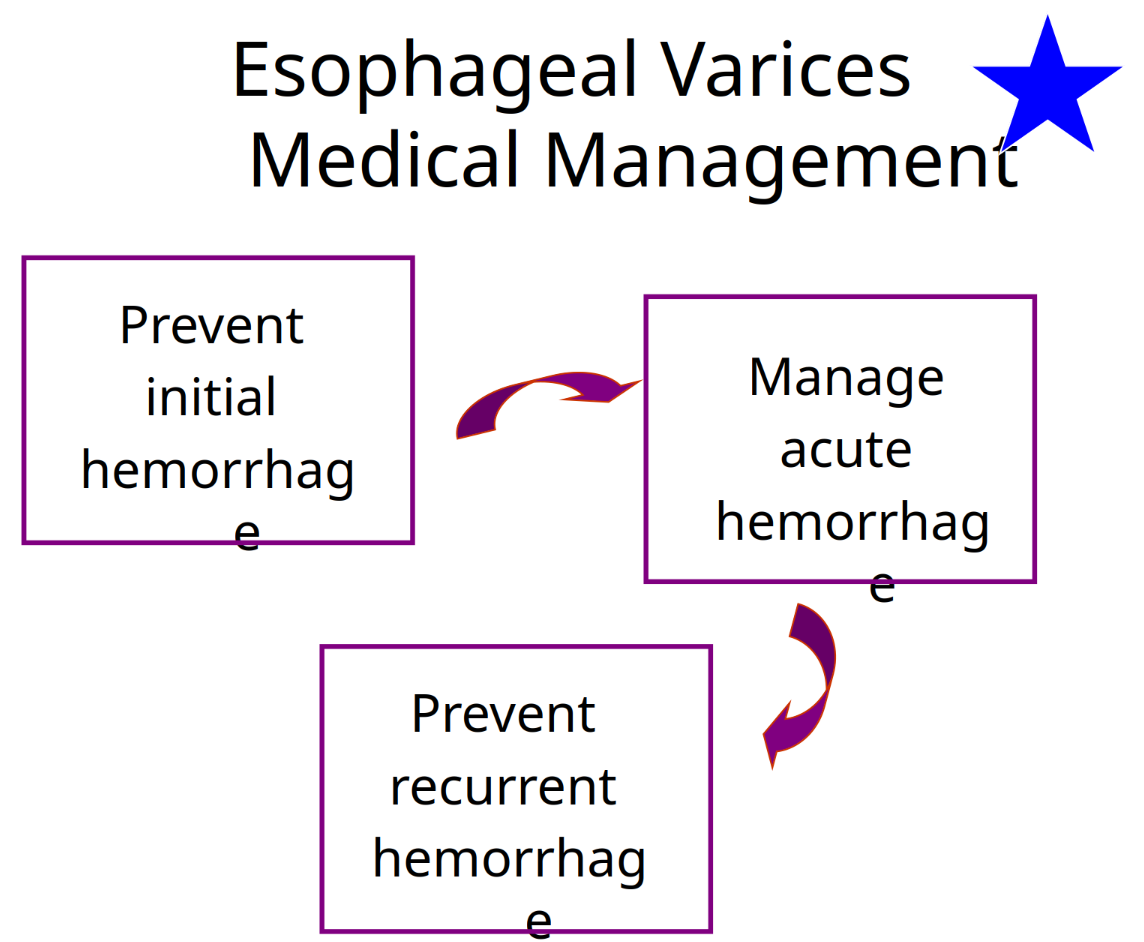
Treatment
of general hemastesis treatment is done till point C for emergency - rest continued for esophageal varices
A)- Stop drugs.
B)- treatment of upper GIT bleeding:
Definition: bleeding occur from upper portion of GIT usually (esophagus, stomach, duodenum ) due to: ( rupture esophageal varices, peptic ulcer (gastroduodenal ), systemic cause as NSAID). Clinical picture: *Overt bleeding in the form of hematemesis and melena.
C)- Stop acute bleeding:
- Urgent hospitalization, complete bed rest with head lower down with warmth.
- Monitor the vitals signs and Pass I/V line.
- Fresh blood transfusion to supply deficient clotting factors and avoid stored blood which contain ammonia (may be packed RBCs to maximize O2 delivery)
(don’t give plasma expander which produce dilution of blood coagulation constituents so, increasing bleeding tendency).
-
FFP (Fresh Frozen Plasma) can be given in case of thrombocytopenia.
-
After restoring blood volume , take blood sample for (clotting and bleeding time and for level of creatinine for acute renal failure).
-
Vitamin K (IM) to correct hypoprothrombinemia) , recombinant activated factor 8 to augment initiation of coagulation.
-
Suction of blood from the stomach then gastric lavage with cold saline. ((avoid destruction of rbc by git which result in increased ammonia = encephalopathy))
-
Sedative (if needed give oxazepam not diazepam “due liver dysfunction, = major depression of brain”), never morphine.
-
Ranitidine I.V. or Proton Pump Inhibitors : aim is decrease stomach PH to reduce gastric irritation and so, decrease frequency of stress induced mucosal lesions ( surgery , trauma, burn , hemorrhage…_)
-
Emergency endoscopy: its aim to detect blood origin , exclude bleeding peptic ulcer from other causes.
D)- Drug treatment:
Only used to control acute bleeding from rupture esophageal varices due to portal hypertension e.g :
- 1- Vasopressin: (via V1 receptors):
- 2- Glypressin (given bolus):
- 3- Terlipressin
- 4- Somatostatin:
E)- Non drug therapy for ROV:
Non drug therapy for ROV:
- Sclerotherapy by injecting varices with sclerosant
- Banding - can be performed by putting rings at basis of varices Endoscopic Band Ligation (EBL) .
- Ballon tamponade.
Prophylaxis:
- Once the initial episode of bleeding is controlled, the risk of rebleeding is 50-80% without further therapy.
(1) Long term injection sclerotherapy usually 4-6 treatment one required to prevent rebleeding, but every year endoscopy should be done to see the condition of varices. *Endoscopy for every cirrhotic patient at diagnosis and periodically
(2)-Beta blockers (propranolol, timolol…): Y It decrease portal pressure by
- B1 blockade in the heart will decrease COP with decrease hepatic flow.
- Block V.D effect of splanchnic blood vessels B2 leading to unopposed alpha1 action leading to splanchnic V.C.
(3) H2 blockers (ranitidine to prevent gastroduodenal erosion)or PPIs.
(4)-Diuretics Y (spironolcatne with low Na in diet to decrease blood volume).
(5)-New treatment to decrease portal pressure by manipulating intrahepatic circulation instead of beta blockers nitrates & nitrites Y……… *Carvedilol………… *Losartan……………. *Ritanserin…………….. *Verapamil…………….. *Metoclopramide……………… *Pentoxiphylline………………………………etc
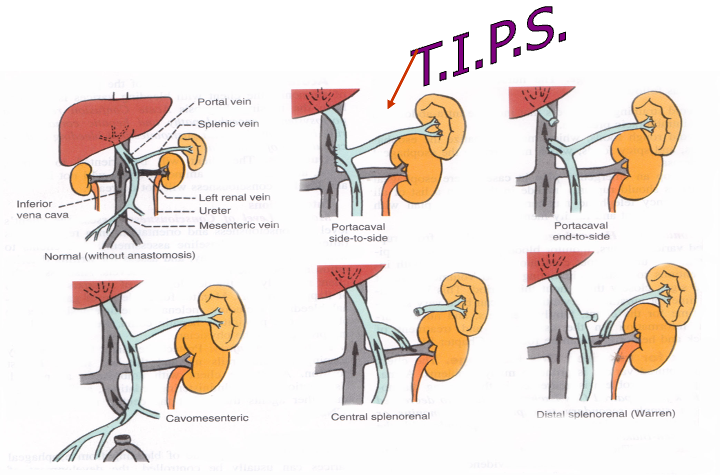
(F)- Shunting Procedures:
Used more after 2nd major bleeding episode TIPS
- shunt is placed between systemic and portal venous systems
- redirect’s portal blood flow
- reduces portal venous pressure
- decompresses varices
ShuntsTransjugular intrahepatic portosystemic shunt
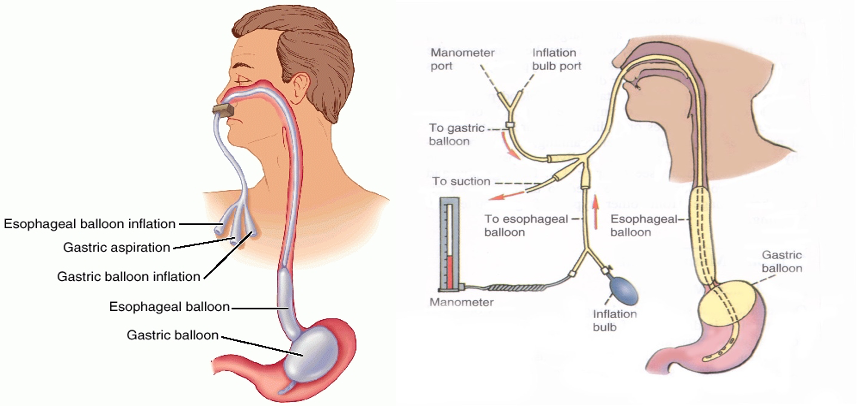
Sengstaken-Blakemore Tube
Three Lumens:
- Esophageal balloon inflation
- Gastric balloon inflation
- Gastric aspiration