Alternative Concomitant divergent (Exotropia) 1ry squint angle 40-45 Y


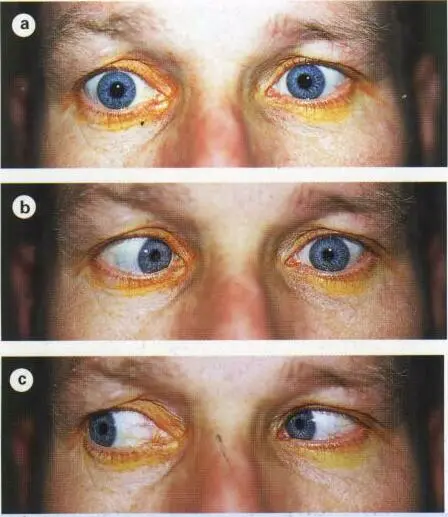
4th nerve palsy
- -Asymptomatic
- -Diplopia (vertical)
- -Head tilt position opposite to the side of the lesion.
- -Hypertropia (the eye is higher )on the affected side.
- -Limitation of depression, most marked in adduction ( SO ms)
Recovery can be achieved within 3-6 months. Neuroimaging if no improvement is noticed within 3-6 months. Z
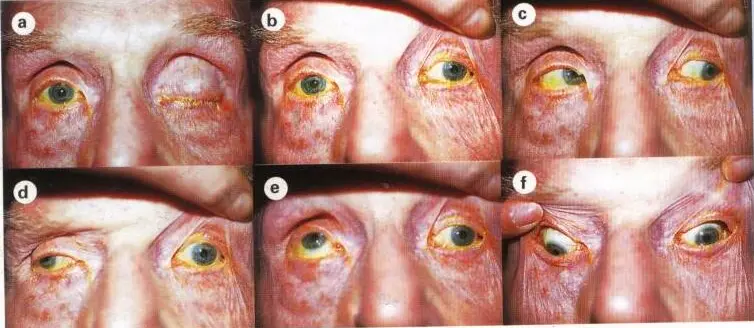

3rd nerve palsy
A) ptosis unilateral B) Exotropia (divergent squint)
Medical Pupil sparing lesions 3rd nerve palsy:
- Diabetes
- Neuropathies
pupil reflexes are not affected
Pupil affected lesions - Surgical 3rd nerve palsy:
- Car Accident
- hemorrhage; hematomas
- Tumours (compression)
Dilation pupil
which statement is correct? A)With involvement of pupil in medical cause B) Needs neuro-radiological

- 2 - divergent extropia
- 5 - ptosis - left 3rd nerve palse

6th nerve palsy
In its primary position eye has convergent squint
Primary position - looking to left side or right the eye which is affected in primary is slight looking Left eye doesnt move behind midline looking right follows
Diagnosis:
- Left Lateral Rectus 6th nerve palsy
Treatment:
- Dont do any surgeries until 6 months after accident
Force: 4 + h hypertropia head titled to opposite side
 Right 6th nerve palsy
Right 6th nerve palsy
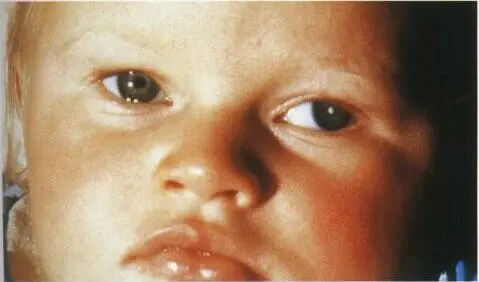
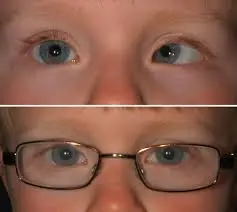
Squint
-
(Strabismus): Eyes are misaligned.
- Esotropia (ET): Eye turns inward. Congenital esotropia is this type, present from early infancy.
- Exotropia (XT): Eye turns outward..
- Hypertropia (HT): Eye turns upward.
- (Pseudoptosis is a false appearance of a droopy lid and not typically associated with simple esotropia).
-
Ptosis (Droopy Eyelid): This is a separate condition where the eyelid itself is low.
- Congenital Ptosis: Present from birth/infancy <2 years. It’s a lid problem, not an eye alignment problem like squint..
- Treatment: Often surgical if the ptosis is significant and affects vision or appearance.

Congenital esotropia
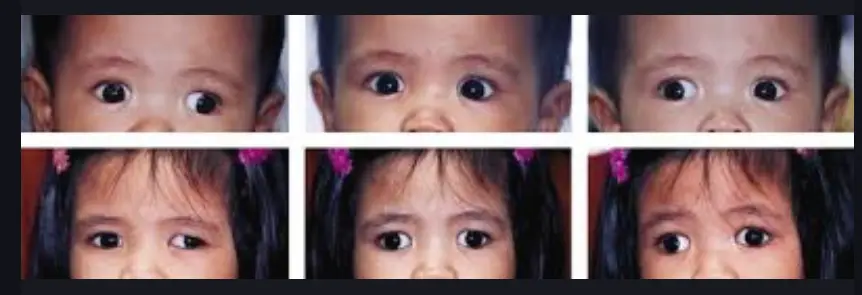

Intermittent exotropia
Which one of these is true regarding intermittent exotropia: It is the most common divergent strabismus
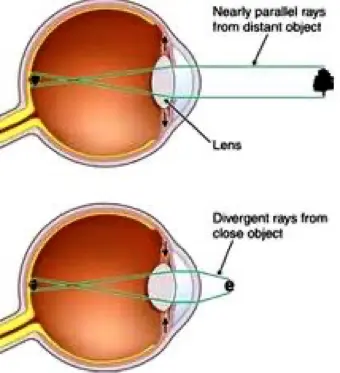
Accommodative Esotropia
Treated by glasses associated with High Hyperopia
One of the following is absent in this case?
- A)Positive family history
- B) High hyperopia
- C) Neurologic impairment and Craniofacial disorder
- D)Comes after 2 y\o
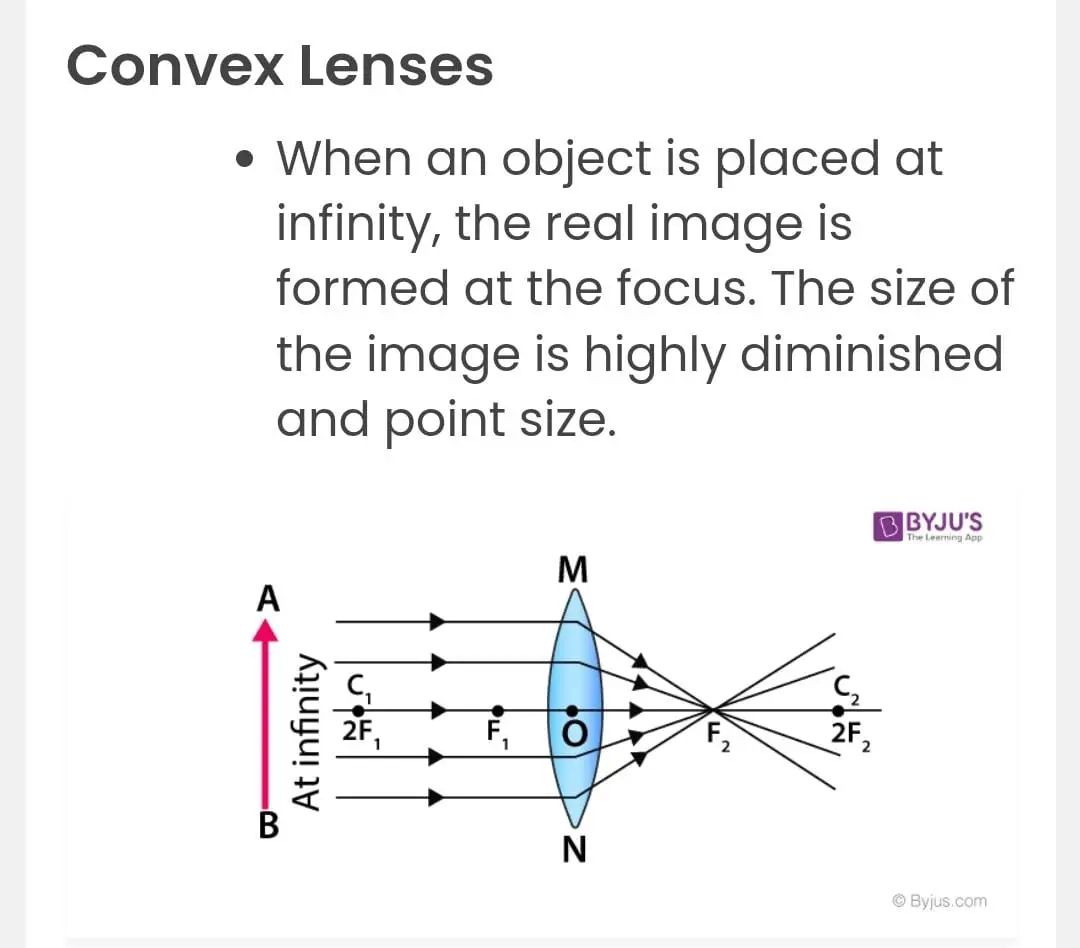
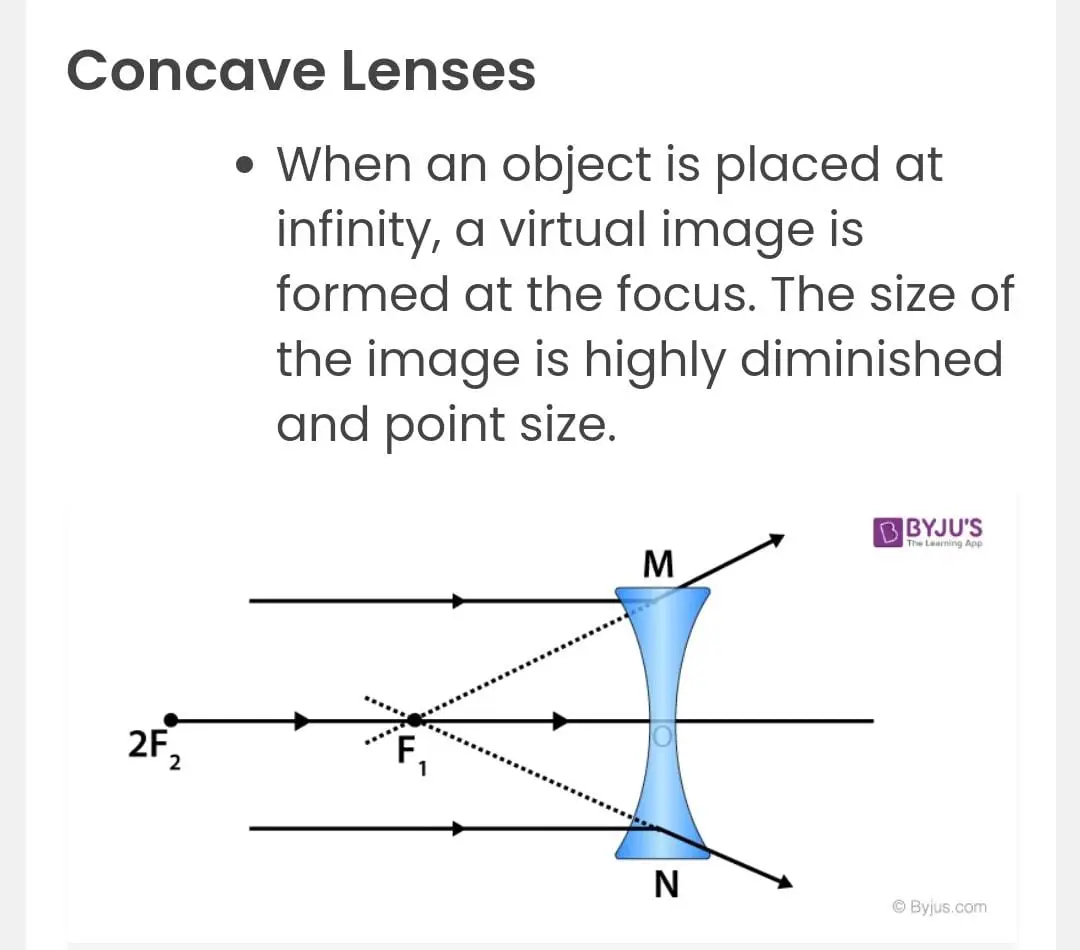
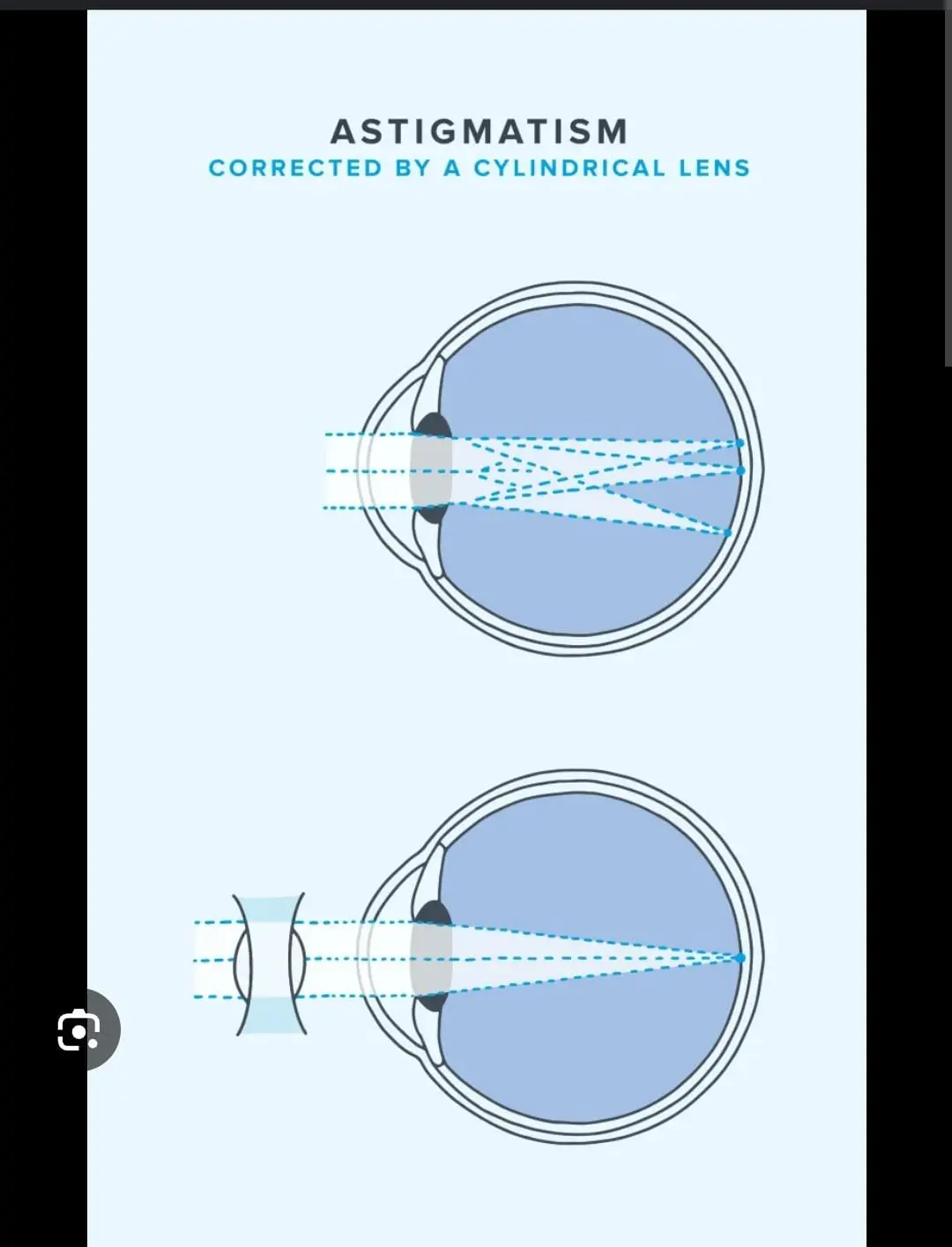
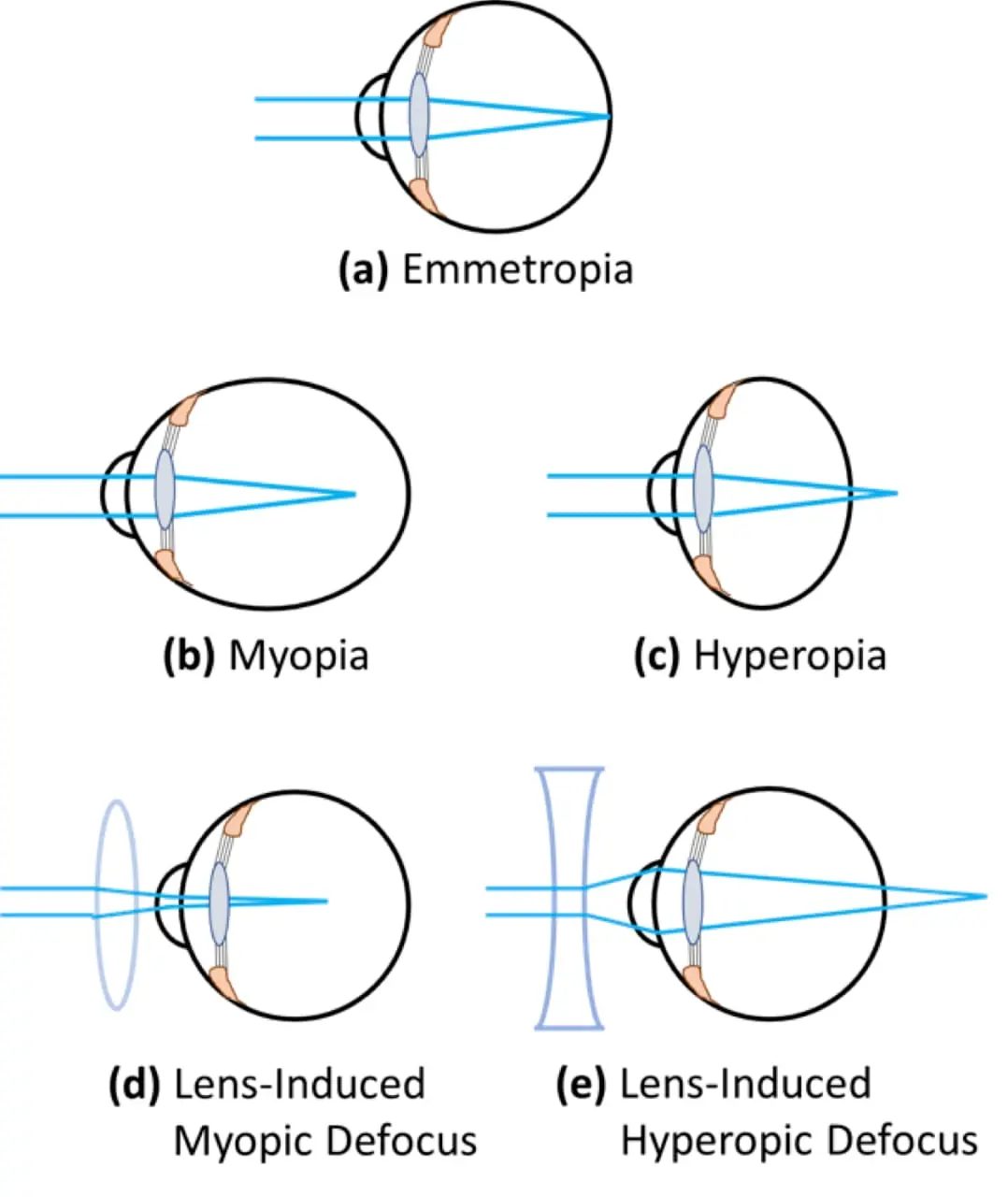
| Type | Cause | Focal Point | Correction |
|---|---|---|---|
| Myopia | Eyeball too long or lens too curved | In front of the retina | Concave (−) lenses |
| Hyperopia | Eyeball too short or lens too flat | Behind the retina | Convex (+) lenses |
| Astigmatism | Cornea/lens unevenly curved (oval shape) | Multiple focal points | Cylindrical (toric) lenses |
| Presbyopia | Age-related lens stiffening, loss of accommodation | Behind the retina for near objects | Convex (+) reading glasses/bifocals |
 PRESBYOPIA.
PRESBYOPIA.

we use this method for? Treatment of amblyopia


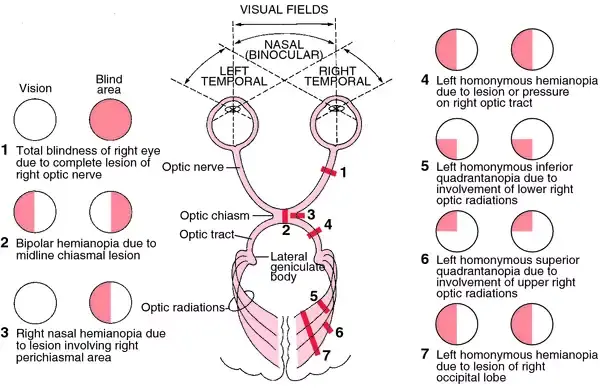
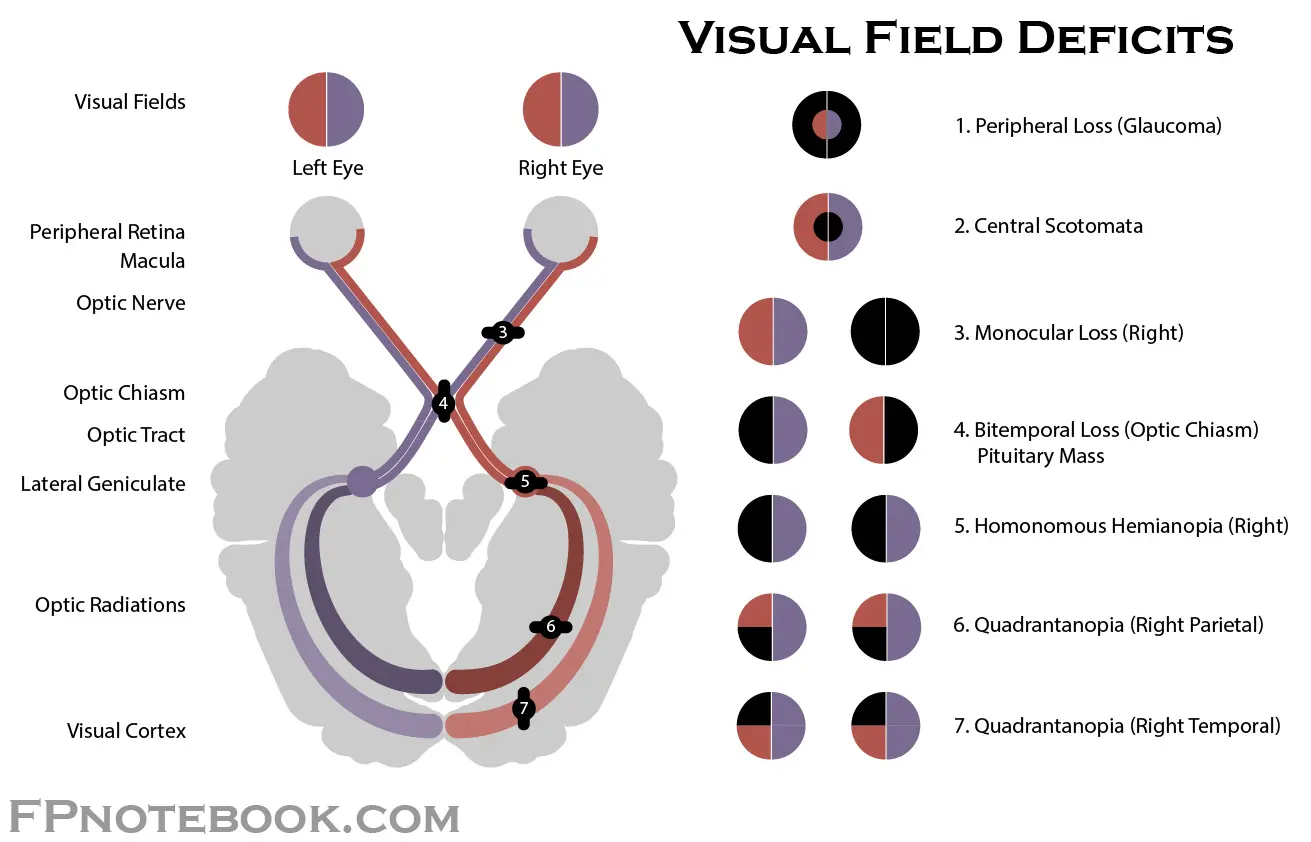
Visual Pathway Disorders
bitemporal hemianopia
pituitary adenoma

Homonymous hemianopia
Homonymous Hemianopia - is loss of vision on one side of both visual fields and may result from occlusion of one of the posterior cerebral arteries with infarction of the occipital lobe.
- Other vascular abnormalities occurring in the middle cerebral artery distribution may produce a hemianopia, but usually, other neurological signs are prominent.
- Any patient with a hemianopia needs a CT or MRI to localize and identify the cause.
Visual Loss
Classification by Time Course
- Acute: sudden onset to days (≤ 2 weeks)
- Subacute: days to weeks (2–6 weeks)
- Chronic: gradual progression over months to years
Acute Visual Loss (≤ 2 Weeks)
| Location | Key Causes | Features / Clues |
|---|---|---|
| Retina | • Central retinal artery occlusion (CRAO) | Painless, “cherry‐red” macula |
| • Central retinal vein occlusion (CRVO) | “Blood and thunder” fundus, sudden blur | |
| • Retinal detachment | Floaters → curtain, photopsia | |
| • Vitreous hemorrhage | Sudden floaters, dark haze | |
| Optic nerve | • Optic neuritis | Pain on eye movement, young adults |
| • Ischemic optic neuropathy (AION) | Painless altitudinal field defect | |
| Media | • Acute angle‐closure glaucoma | Severe eye pain, halos, mid‐dilated pupil |
| • Corneal ulcer / keratitis | Pain, redness, discharge | |
| Vascular / CNS | • Migraine (with aura) | Transient scotoma, then HA |
| • Stroke (occipital cortex) | Homonymous hemianopia, neuro signs | |
| Traumatic | • Globe rupture / orbital hemorrhage | History of trauma, pain, eyelid swelling |
| Inflammatory | • Uveitis | Photophobia, redness, floaters |
Chronic Visual Loss (> 1–2 Months)
| Location | Key Causes | Features / Clues |
|---|---|---|
| Lens / Media | • Cataract | Gradual blur, glare, no pain |
| • Chronic vitreous opacities (e.g. asteroid hyalosis) | Floaters, mild blur | |
| Glaucoma | • Primary open‐angle glaucoma | Peripheral field loss → tunnel vision |
| Retina | • Age‐related macular degeneration (AMD) | Central vision loss, metamorphopsia |
| • Diabetic retinopathy | Microaneurysms, neovascularization | |
| • Retinitis pigmentosa | Night blindness, bone‐spicule pigments | |
| Optic nerve | • Chronic optic atrophy | Pale disc, slow progression |
| • Normal‐tension glaucoma | Optic cupping, field loss | |
| Systemic / CNS | • Neurosyphilis, TB | Progressive, +/- other neurologic signs |
| • Brain tumors | Visual field defects, headache |