Internal Medicine
- Less common than hypothy
- 99% cases are due to problem in the gland ( prim. hyperthyroidism).
- Pituitary causes, like TSH secreting adenoma only 1% (sec. hyperthy)
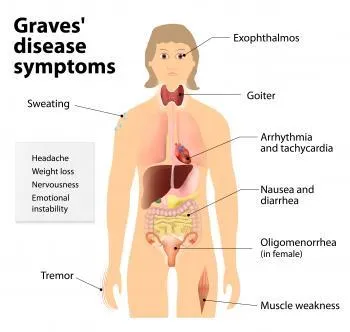
S/S of General HYPERTHY
- Weight loss (inspite of increased appetite)
- Tachycardia or atrial fibrillation ⇒ palpitations
- Excess sweating, warm wet palms
- Continuous low grade fever 37.5-37.8 c
- Heat intolerance
- Feeling warm even in cold weather
- Diarrhea
- Hand tremors
- Polydipsia; drinking alot fluids
- Hyperactive & restless
- Lack of sleep
- Weakness, fatigue
- Menstrual irregularities; hypo + hyper
- Proximal myopathy; shoulders, hips
- Systolic HTN
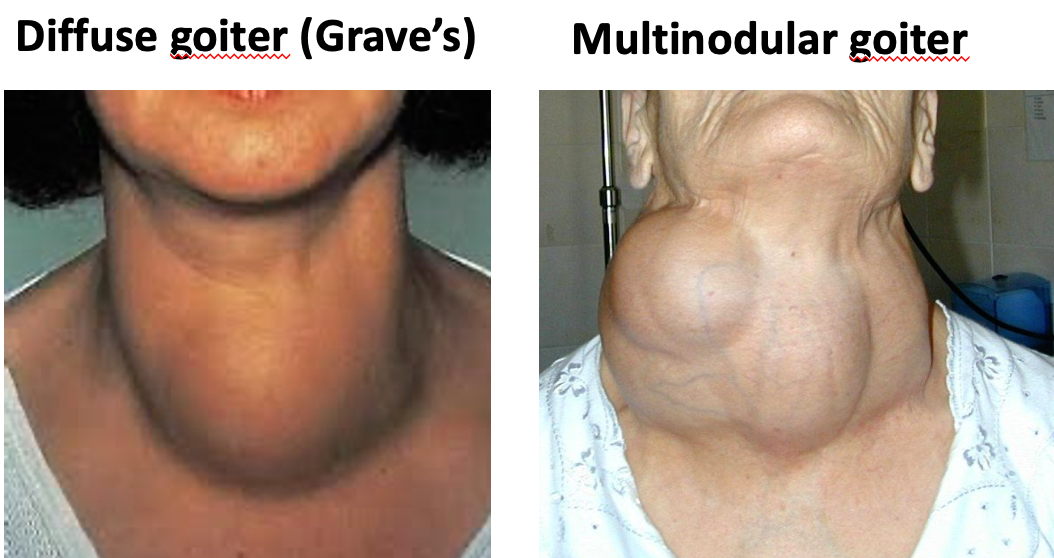
- Goiter (often)
- Hyper reflexia
ETIOLOGIES OF HYPERTHY.
- Grave’s disease (most common cause) - TRSA - TRAB
- Toxic goiter
- Toxic solitary nodule
- Drugs (amiodarone). Can cause hypo also
- Sub acute thyroiditis (viral infection of the gland) (De Quervain’s thyroiditis)
- Overdose of thyroxine tabs.
- Thyrotoxicosis factitia (use of thyroxine for non thyroidal illness)
- Thyroid Storm
Comparison of Thyroid Conditions
| Feature | Grave’s Disease | Solitary Toxic Nodule | Toxic Multinodular Goiter | Subacute Thyroiditis | Amiodarone-Induced | Hyperthyroidism in Pregnancy | Thyroid Storm |
|---|---|---|---|---|---|---|---|
| Cause | Autoimmune (TRAB antibodies) | Single overactive nodule | Multiple overactive nodules | Viral infection | Iodine content of amiodarone | Exacerbation of thyrotoxicosis | |
| Prevalence | Most common cause of hyperthyroidism | Rare | |||||
| Goiter | Diffusely enlarged | Single nodule palpable | Multiple nodules palpable | Mildly enlarged | Variable | ||
| Tenderness | Non-tender | Usually non-tender | Usually non-tender | Tender | Variable | ||
| Other Symptoms | Fever, malaise | Variable | High fever, altered mental status, tachycardia, fluid loss | ||||
| Unique Features | Exophthalmos, pretibial myxedema, clubbing of fingers | Recent history of viral respiratory infection, transient hyperthyroidism | Precipitated by infection, surgery | ||||
| Treatment | Antithyroid drugs, radioactive iodine, surgery | Radioactive iodine, surgery | Radioactive iodine, surgery | NSAIDs, corticosteroids | Discontinue amiodarone (if possible), treat hyper- or hypothyroidism | PTU in first trimester, then carbimazole | ICU admission, supportive care |
Notes:
- TRAB: TSH Receptor Stimulating antibodies
- TFTs: Thyroid Function Tests
- PTU: Propylthiouracil
- Carbimazole: Antithyroid medication
- LAA: Low-dose radioactive iodine ablation
INVESTIGATIONS (in hyperthyr.)
-
TFTs; fT4 : high | fT3 : High | TSH: Low
-
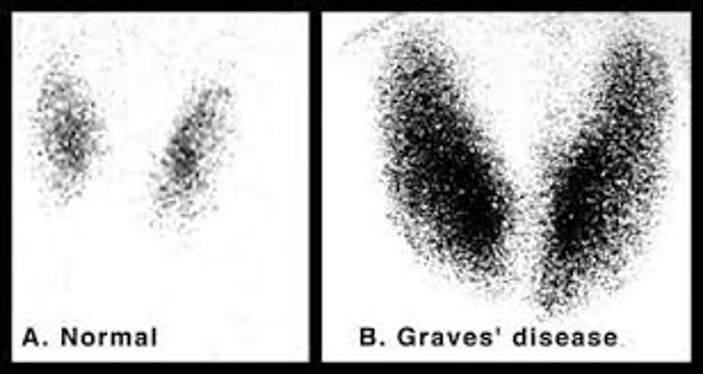
RAIU scan (not done in every case)
- Radio iodine given orally or i.v.
- Taken up by the active areas of the gland
- Grave’s : Increased uptake diffusely
- Toxic multinodular goiter: Increased uptake by the nodules
- Toxic adenoma : increased uptake by the single nodule only
- De quervain’s & post partum thyroiditis: Low uptake
- Serum antibodies (not done in every case) Present in hyperthyroidism due to Grave’s disease
- TSH receptor stimulating ab. (specific) (also called TRAB)
- Anti TPO antibodies (in some Grave’s patients)
(anti TPO are present mainly in Hashimoto’s thyroiditis which causes hypothyroidism)
Treatments
Hyperthyroidism in a preg. lady
- PTU in the first trimester, then switch to Carbimazole
- LAA radio iodine
TREATMENT In Hyper
(Grave’s, toxic multinodular, toxic adenoma)
| Symptomatic Rx | Definitive Rx |
|---|---|
| Beta blockers (control palpitations, sweating, restlessness) | Antithyroid drugs |
| Radioiodine | |
| Surgery (effective treatment) |
(definitive Rx does not have a quick effect)
STEP WISE TREATMENT OF GRAVE’S
- First, beta blockers (symptomatic control)
- Carbimazole (for about 2 months), to lower the hormone levels
- Finally, once hormones normalise, Radio iodine treatment (in the U.S.)
If you give Iodine treatment without giving prior carbimazole, it can be a problem
A- Antithyroid drugs
- Carbimazole/methimazole, Propylthiouracil (PTU)
- Not a permanent cure ⇒ disease relapses in many cases after stopping, specially Grave’s
- First choice drug is always Carbimazole (in preg., 1st choice is PTU)
- After starting or changing the dose, check TFTs after at least 6 wks. ( hormones take some time to normalise)
S/E:
- Hepatitis: Report to the doctor if jaundice develops
- Rash
- Agranulocytosis (low neutros); may cause fever, sore throat. Report immediately to the doc.
B- Radio iodine Rx
- First choice Rx in the U.S.
- LAA in pregnancy (do preg. test before giving)
- Radio active Iodine given orally ⇒ suppresses thyroid hormone synthesis
- A single dose permanently controls hyperthy. in 90% patients.
- Normalisation of S/S & labs takes few months (so continue beta blockers till then)
Side effects of radio iodine Rx:
- Hypothyroidism ⇒ very common (have to start thyroxine then)
- No risk of malignancy
- No risk of congenital abnormalities in babies born to mothers who got this Rx - but LAA in pregnancy - one time dose can be repeated after 6 months
C-SURGICAL TREATMENT
- Subtotal thyroidectomy provides long term control of the disease
- Done if drugs fail, or if patient refuses radio iodine
D- DeQuervain’s thyroiditis
Rx:
- Beta blockers (symptom control)
- NSAIDs (for inflammation)
- Prednisone (for inflammation)
What will the radio-iodine scan show in De Quervain’s thyroiditis? decreased uptake
E- Treatment of storm Z
- PTU
- SSKI (saturated solution of potassium iodide)
- Cooling blanket
- i.v. fluids
- Beta blockers
- Prednisone
SURGERY
Grave’s Disease
- Most common form of thyrotoxicosis (60-80 %)
- Any age, common in 20-40 age group
- 5 times > in females
- Autoimmune disease
- 15% relatives with same disorder
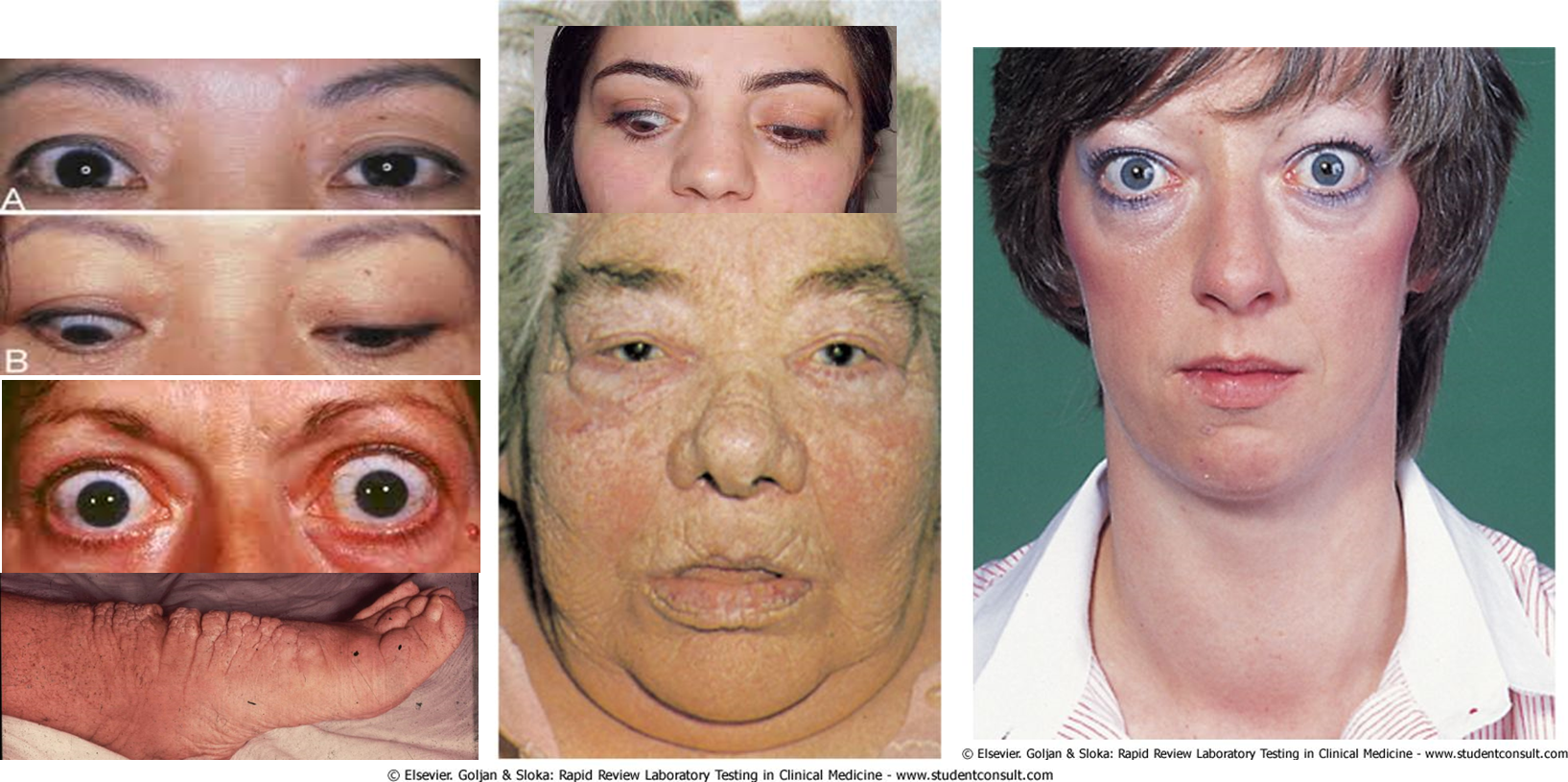
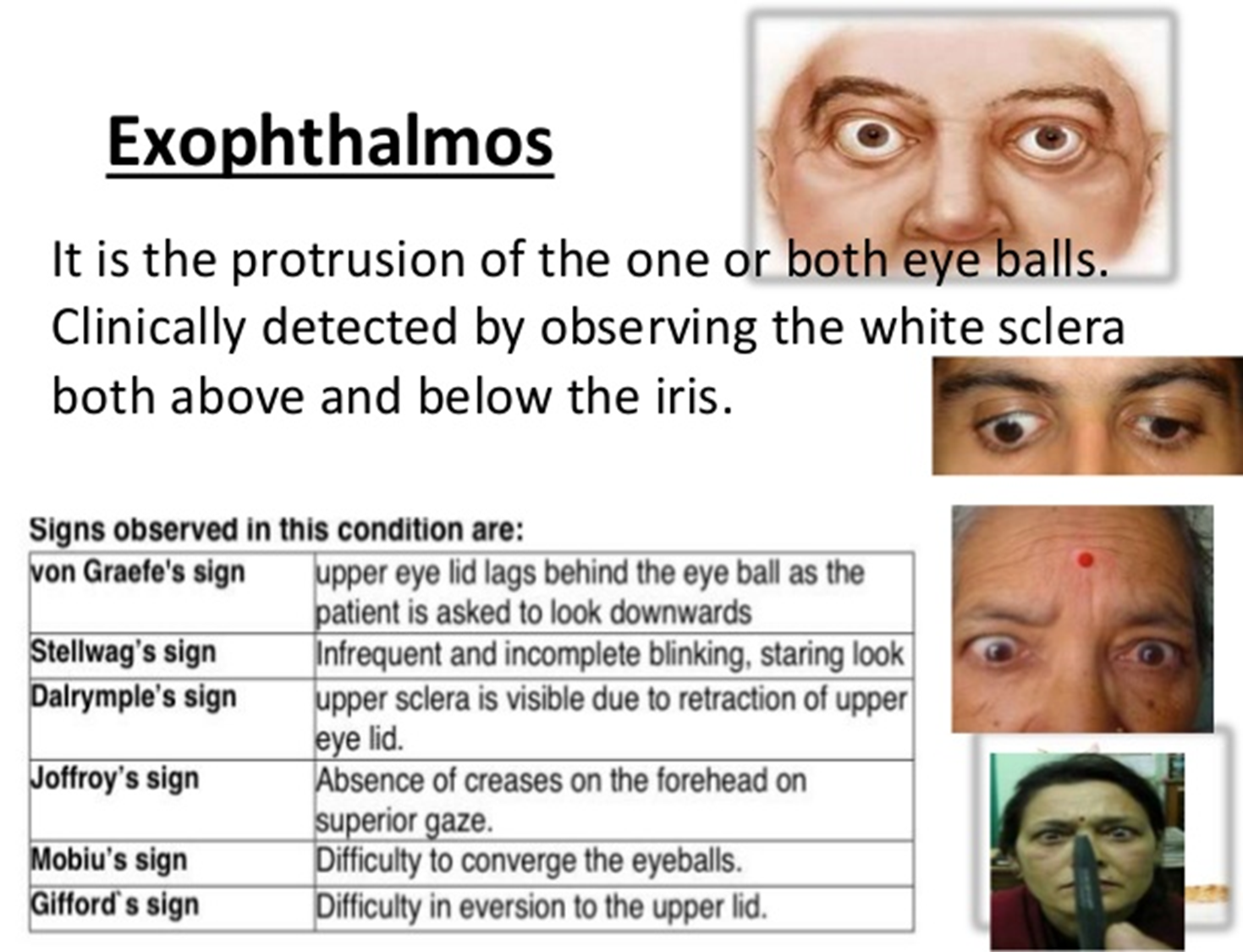
- Disease consists of one or more of the following:
- Thyrotoxicosis
- Goitre (diffuse enlargement, ± bruit)
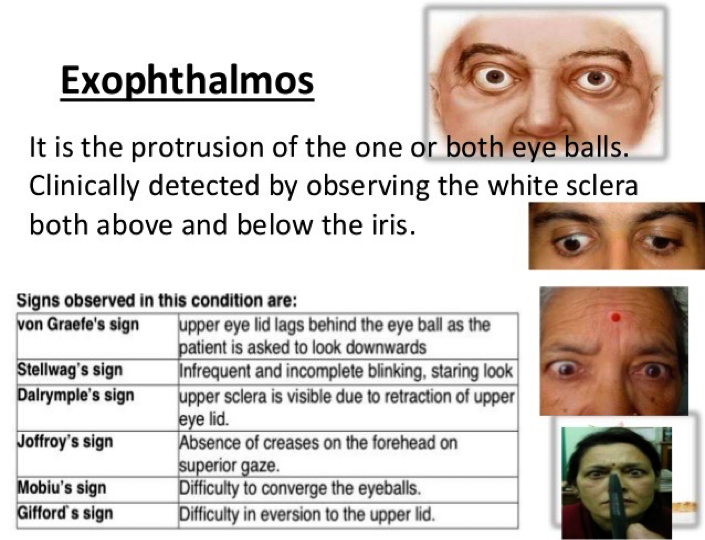
- Ophthalmopathy (exophthalmos, lid-lag, lid retraction, chemosis ophthalmoplegia)
- Dermopathy (pretibial myxedema – only 2%)

Features of thyrotoxicosis (Grave’s Disease)
- Heat intolerance, excessive sweating
- CVS: tachycardia, palpitation, atrial fibrillation, CHF
- GI: Wt. loss, increased appetite, diarrhoea
- Neuromuscular: anxiety, nervousness, tremor, proximal myopathy
- Reproductive: amenorrhea, infertility

Diagnosis of Grave’s Disease
- Low TSH, high FT4, &/or T3
- Detection of TSH-R Ab: TSI-thyroid stimulating immunoglobulin
- Isotope scan- diffuse high uptake
- Ultrasound- rarely needed
Treatment of Grave’s Disease
-
Antithyroid drugs:
- Blocks coupling of iodine with tyrosine
- Supress synthesis of thyroxine
- Carbimazole- 30-60 mg daily, divided dose-4-6 weeks
- Other drugs- Propylthiouracil, β- blocker- propranolol
- Skin rash, agranulocytosis,
- Long term remission- only 20-30%
-
Radioactive iodine ablation:
- RAI treatment of choice for most.
- 1-2 dose- oral,
- 90% cure at 1 year
- Contraindications: pregnancy, lactation, suspicion of carcinoma, low iodine (<20%) uptake
-
Surgery:
- RAI ablation contraindicated.
- Preoperatively- euothyroid with antithyroid medication.
- Total thyroidectomy- recommended

FM
Hyperthyroidism is an excessive concentration of thyroid hormones in tissues caused by:
- Increased synthesis of thyroid hormones,
- Excessive release of preformed thyroid hormones, or
- An endogenous or exogenous extrathyroidal source.
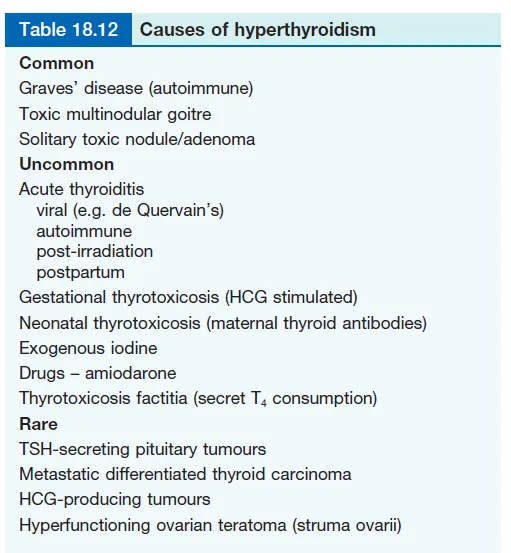
Table 18.12 Causes of Hyperthyroidism
-
Common
- Graves’ disease (autoimmune)
- Toxic multinodular goitre
- Solitary toxic nodule/adenoma
-
Uncommon
- Acute thyroiditis
- viral (e.g. de Quervain’s)
- autoimmune
- post-irradiation
- postpartum
- Gestational thyrotoxicosis (HCG stimulated)
- Neonatal thyrotoxicosis (maternal thyroid antibodies)
- Exogenous iodine
- Drugs – amiodarone
- Thyrotoxicosis factitia (secret T₄ consumption)
- Acute thyroiditis
-
Rare
- TSH-secreting pituitary tumours
- Metastatic differentiated thyroid carcinoma
- HCG-producing tumours
- Hyperfunctioning ovarian teratoma (struma ovarii)
Causes of Hyperthyroidism
Graves’ disease:
- This is the most common cause of hyperthyroidism and is due to an autoimmune process.
- Serum IgG antibodies bind to TSH receptors in the thyroid, stimulating thyroid hormone production.
Other Causes of Hyperthyroidism/Thyrotoxicosis
- Solitary toxic adenoma/nodule
- Toxic multinodular goitre
- de Quervain’s thyroiditis
- Transient hyperthyroidism from an acute inflammatory process, probably viral in origin.
- Postpartum thyroiditis
- Amiodarone-induced thyrotoxicosis


Diagnosis Of Hyperthyroidism
Hyperthyroidism is diagnosed based on symptoms, physical exam, and blood tests to measure levels of thyroid stimulating hormone (TSH) and thyroid hormones T₃ and T₄.
Investigations
- Serum TSH is suppressed in hyperthyroidism (< 0.05 mU/L)
- A raised free T4 or T3 confirms the diagnosis
- TPO and thyroglobulin antibodies are present in most cases of Graves’ disease.
- Radioactive Iodine Uptake
- Ultrasound scan
Diagnostic Workup of Hyperthyroidism

Treatment
Three possibilities are available:
- Antithyroid drugs
- Radioactive iodine
- Surgery: subtotal thyroidectomy
Long-term Consequences Of Hyperthyroidism
- Increased risk of osteoporosis.
- Increased the risk of atrial fibrillation which may predispose to thromboembolic disease.
- Cardiac Failure
- Nodular abnormalities – Goitre:
- Goitre is a lump in the neck caused by the thyroid gland becoming swollen.
Table 18.14 Z
Goitre – causes and types
-
Diffuse
- Simple
- Physiological (puberty, pregnancy)
- Autoimmune
- Graves’ disease
- Hashimoto’s disease
- Thyroiditis
- Acute (de Quervain’s thyroiditis)
- Iodine deficiency (endemic goitre)
- Dyshormonogenesis
- Goitrogens (e.g. sulfonylureas)
- Simple
-
Nodular
- Multinodular goitre
- Solitary nodular
- Fibrotic (Reidel’s thyroiditis)
- Cysts
-
Tumours
- Adenomas
- Carcinoma
- Lymphomas
-
Miscellaneous
- Sarcoidosis
- Tuberculosis

Investigations:
- Thyroid function tests
- Thyroid antibodies
- Ultrasound
- Chest and thoracic X-rays
- Fine-needle aspiration (FNA)
- Thyroid scan
Drugs known to affect thyroid function
-
Inhibition of T4/T3 synthesis
- Propylthiouracil
- Methimazole
-
Inhibition of T4/T3 secretion
- Lithium
- Iodide
- Amiodarone
-
TSH suppression
- Glucocorticoids
- Dopamine agonists
Therapeutics BIO
Primary Hyperthyroidism (decreased TSH increased FT4 & FT3)
- Grave’s disease
- Multi-nodular Toxic Goiter
- Autonomous Toxic Adenoma
- Iodine Overload, Procor
Secondary Hyperthyroidism (Increased TSH, FT4, FT3)
- TSH-Producing pituitary adenoma
- Thyroid Hormone Resistance
- Gestational Thyrotoxicosis
Thyrotoxicosis without hyperthyroidism
- Sub-acute thyroiditis
- Silent Thyroiditis
- Thyrotoxicosis Facticia
Administration of T3 or T4 (Facitious or iatrogenic Hyperthyroidism)
MEDICAL Examination
Grave’s Disease
- Most common form of thyrotoxicosis (60-80 %)
- Any age, common in 20-40 age group
- 5 times > in females
- Autoimmune disease
Disease consists of one or more of the following: - Thyrotoxicosis - Goitre (diffuse enlargement, ± bruit) - Ophthalmopathy (exophthalmos, lid-lag, lid retraction, chemosis ophthalmoplegia) - Dermopathy (pretibial myxedema – only 2%)
Features of thyrotoxicosis (Grave’s Disease)
- Heat intolerance, excessive sweating
- CVS: tachycardia, palpitation, atrial fibrillation, CHF
- GI: Wt. loss, increased appetite, diarrhoea
- Neuromuscular: anxiety, nervousness, tremor, proximal myopathy
- Reproductive: amenorrhea, infertility
MIMG
Thyroid scintigraphy Shows a *diffuse uptake of radioactive iodine *
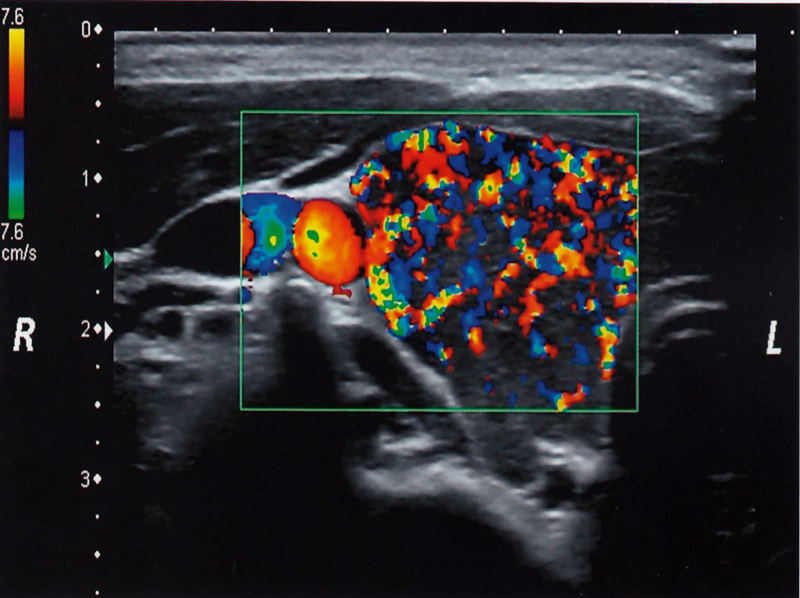
Thyroid ultrasound (with color Doppler) Shows an enlarged, hypervascular thyroid
Thyroid ultrasound of the right thyroid lobe (color Doppler) Numerous red and blue areas consistent with increased vascularization are visible within the color Doppler image window (green rectangle).
This finding is typical in Graves disease.