Preoperative Preparation & Postoperative Care
Omar Alaidaroos
Patient History:
- Explore the patient’s understanding of the need for surgery to be performed.
- Ask about any previous surgeries and anaesthetics that the patient may have and how those procedures were tolerated.
- Ask about the patient’s family health history. Include any adverse reactions to anaesthesia, such as malignant hyperthermia.
- Ask about Co-morbidities:
A. Diabetics Patients:
- Patients whose diabetes is controlled by diet alone, nothing is needed other than preoperative serum glucose monitoring.
- Patients taking long-acting Oral Hypoglycaemic drugs such as Metformin should discontinue 2-3 days to avoid intraoperative hypoglycaemia.
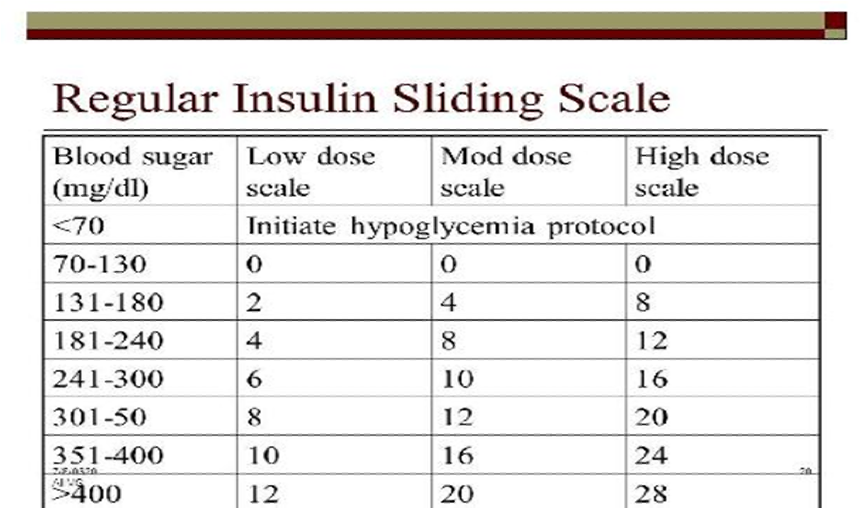
- Patients taking Insulin should receive one half or 2/3 of their usual AM insulin dose, and then soluble insulin should be given on a Sliding Scale based on finger stick monitoring.
B. Cardiovascular System
A. Ask about a history of dysrhythmias, chest pain, or myocardial infarction (heart attack, MI) because of the potential for re-infarction with surgery.
- If the patient had a heart attack more than 6 months ago, the risk of reinfarction is about 6%.
- If the MI was between 3 and 6 months before a procedure, the risk increases to 15%.
- If the surgery is within 3 months, the risk increases to 30% with a 50% mortality!
B. Assess breath sounds and the lower extremities for signs of fluid retention.
- Listen for rales that do not clear with coughing, and for pitting oedema.
- Both are a sign of symptomatic congestive heart failure, and surgery should be postponed until the patient’s symptoms have been controlled.
C. Ask about hypertension, and if blood pressure is well controlled by medications.
- Patients are generally encouraged to take their blood pressure medications on the morning of surgery with a sip of water to keep pressures under control.
- Hypertension increases the risk for coronary artery disease, stroke, congestive heart failure, and renal failure.
- If the hypertension is mild and controlled, the evaluation can take place up to 2 months before surgery.
- If moderate, evaluation and clearance should be within 2 weeks.
- If severe, surgery should be postponed with immediate evaluation and intervention.
D. Respiratory diseases:
A. Ask about dyspnea both at rest and with exertion.
B. Ask about the presence of a cough. If productive, it is a clue to an upper respiratory infection, which leads to cancellation of surgery.
- A dry cough may be a side effect of the use of an angiotensin-converting enzyme (ACE) inhibitor medication used to treat hypertension.
C. Ask about a history of chronic obstructive pulmonary disease (COPD), and any current treatment, including antibiotics, bronchodilators or nebulizer treatments, or use of home oxygen therapy.
- The anaesthesia provider may give the patient a nebulizer treatment before induction.
D. Educate the patient about postoperative lung expansion manoeuvres such as Incentive spirometry.

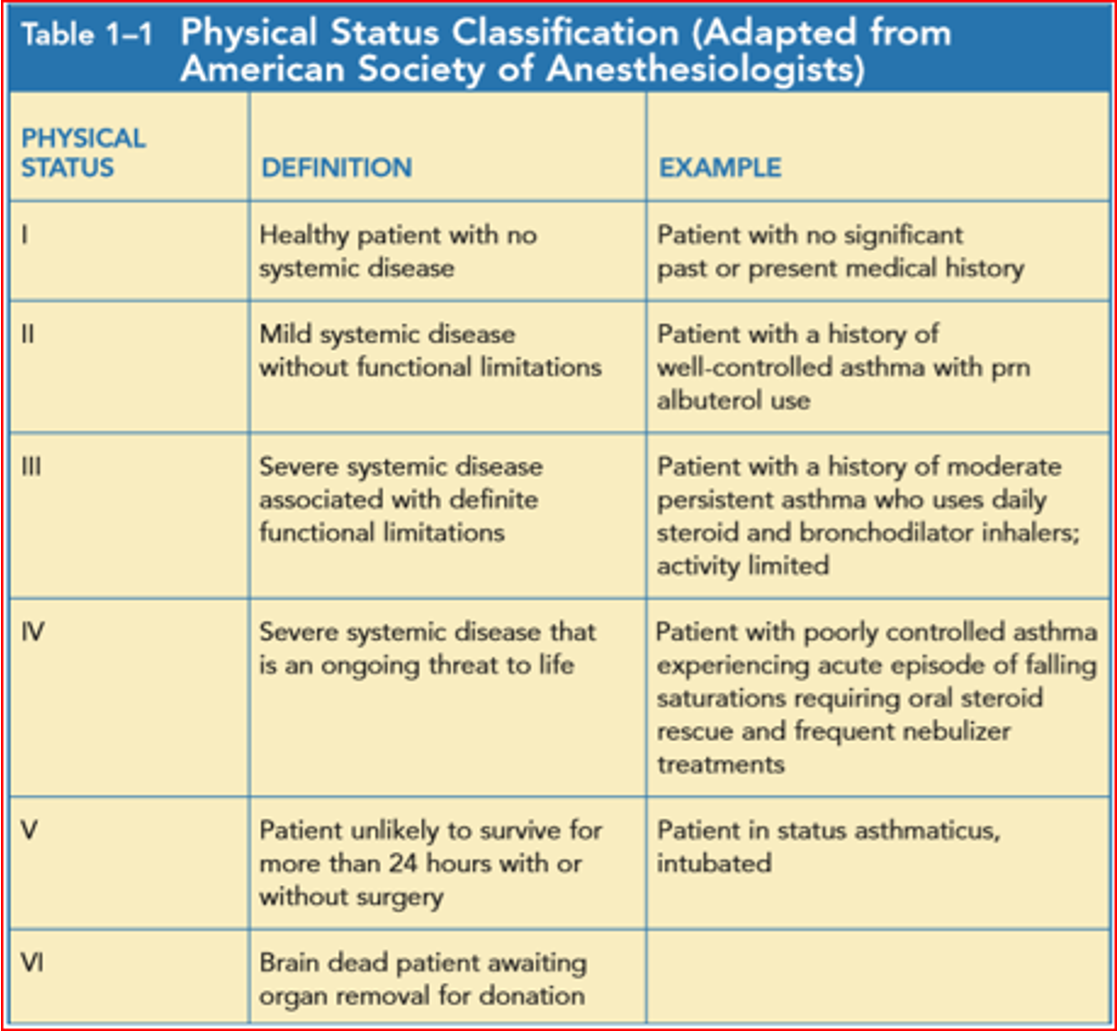
- An E is added to the status number to designate an emergency operation.
- Ask about current medication use.
- A patient who takes aspirin, Coumadin, or ibuprofen is at an increased risk for bleeding.
- Those who need Aspirin (antiplatelets) continuously, as in mechanical heart valves, can be given heparin preoperatively.
- Discontinue Coumadin 5 days preoperatively, start LMWH and check PT or INR on the day of surgery to make sure clotting studies are within normal limits before surgery.
- The normal range for your PT results is: 11 to 13.5 seconds, INR of 0.8 to 1.1. PTT: 30 to 45 seconds.
- Stop IV heparin 6 hours prior to surgery.
- LMWH – should be stopped 12 hours before surgery.
Drugs to hold for at least 2 weeks preoperatively:
- Aspirin
- MAO inhibitors (for Parkinson’s disease)
- Oral central alpha agonists (e.g., methyldopa)
- Oral contraceptive pills
- Antirheumatic agents
Drugs to hold for 4–5 days preoperatively:
- NSAIDs, selective COX-2 inhibitors
- Antiplatelets: Dipyridamole (Persantine®).
- Anticoagulants (e.g., warfarin)
Drugs to give on the morning of surgery: should be taken with a small sip of water only.
- Most cardiac meds (antiarrhythmics, digoxin, nitrates, beta-blockers)
- Calcium channel blockers
- Pulmonary medications (e.g., inhalers, nebulizers)
- Endocrine medications (thyroid meds and corticosteroids)
- Most GI medications (e.g., H2 blockers, PPIs)
- Seizure medications (to avoid withdrawal)
- Eye drops
- Narcotics
- Immunosuppressives
- Ask about medication allergies and intolerances.
- On the day of surgery, make sure that a red allergy identification band is applied to the patient’s wrist. Ask about non-drug allergies, too.
- Ask about illicit drug use, abuse, and addiction in the same way you asked about current medication use.
- Once you explain to patients that there are drug interactions between these drugs and anaesthetic agents, patients will usually respond honestly.
- Ask about tobacco use.
- Smokers also have a higher incidence of reactive airway disease, which may result in laryngospasm on induction.
- Encourage patients to stop smoking a minimum of 8 weeks before surgery.
- Cessation for 2 weeks will improve the level of carbon monoxide, but secretion is still a problem.
- Ask about the possibility of pregnancy, specifically to determine the date of the patient’s last menstrual period.
- This is needed to prevent unnecessary exposure of the foetus to anaesthetic agents, particularly during the first trimester of pregnancy.
- Menstruation is not a contraindication; the operation need not be postponed.
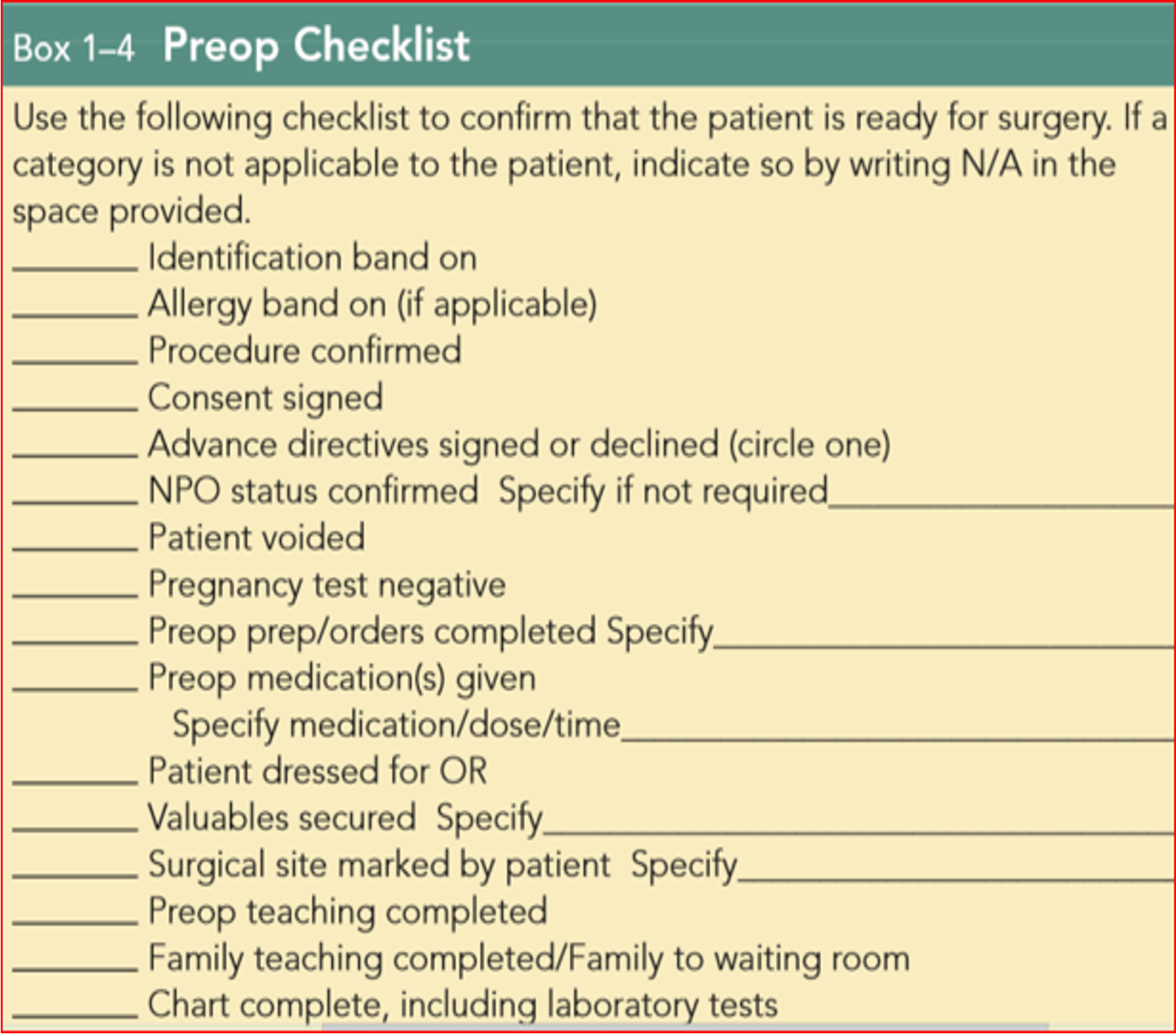
Preoperative Preparation of the Surgical Patient in Ward
-
Review the patient’s history and physical examination, and write a preoperative note assessing the patient’s overall condition and operative risk.
-
Preoperative laboratory evaluation: Electrolytes, BUN, creatinine, INR/PTT, CBC, platelet count, UA, ABG, pulmonary function test. Chest x-ray (>35 yrs old), EKG (if older than 35 yrs old or if cardiovascular disease).
-
Type and cross for an appropriate number of units of blood.
-
Frequency of vital signs; input and output recording; neurological or vascular checks. Notify physician if blood pressure <90/60, >160/110; pulse >110; pulse <60; temperature >101.5; urine output <35 cc/h for >2 hours; respiratory rate >30.
-
Skin preparation:
-
Patient to shower and scrub the operative site with germicidal soap (Hibiclens) on the night before surgery.
-
On the day of surgery, if hair must be removed, it should be clipped in the operating room.
-
-
Prophylactic antibiotics if indicated.
-
Preoperative incentive spirometry on the evening prior to surgery may be indicated for patients with pulmonary disease.
-
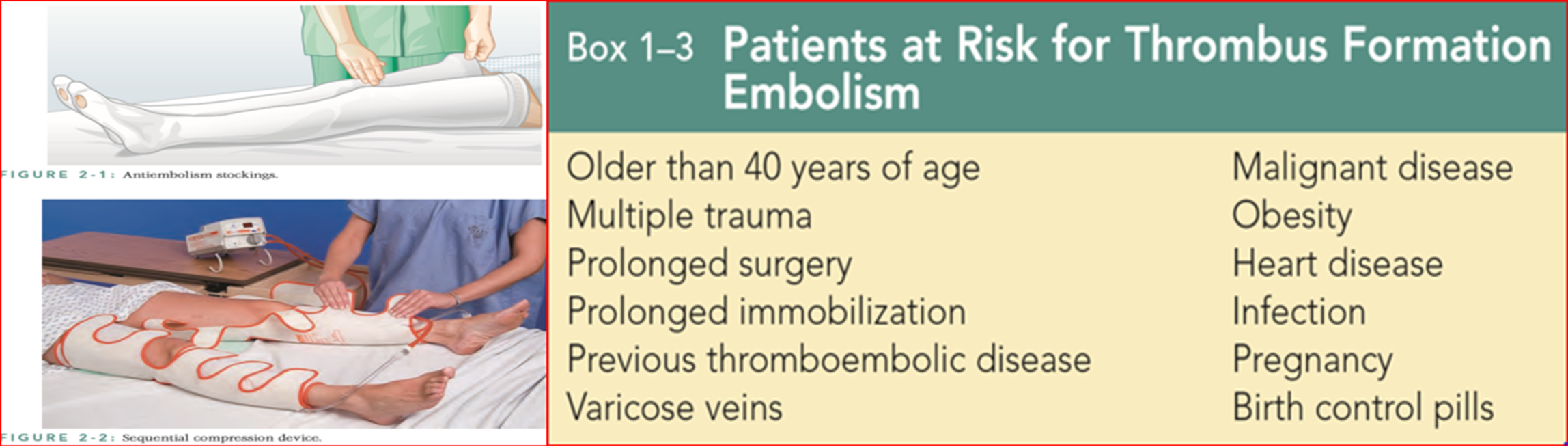
Thromboembolic prophylaxis should be provided for selected, high-risk patients.
-
Bowel preparation:
- Bowel preparation is required for upper or lower GI tract procedures.
Mechanical Prep:
- Day 1: Clear liquid diet, laxative (milk of magnesia 30 cc or magnesium citrate 250 cc), tap water or Fleet enemas until clear.
- Day 2: Clear liquid diet, NPO, laxative.
- Day 3: Operation.
Oral Antibiotic Prep:
- One day prior to surgery, after mechanical or whole gut lavage, give neomycin 1 gm and erythromycin 250 mg at 1 p.m., 2 p.m., 11 p.m.
-
Removal of cosmetics, contact lenses, dentures, etc.
-
Diet: NPO after midnight.
-
IV and monitoring lines: At least one 18-gauge IV for initiation of anaesthesia.
IV Orders: D5 1/2 NS at 100 cc/hour.
Oxygen: 6 L/min by nasal canula.
Fasting Recommendation
| Ingested material | Minimum fasting period (hr) |
|---|---|
| Clear liquids | 2 |
| Breast milk | 4 |
| Infant formula | 6 |
| Nonhuman milk | 6 |
| Light meal (toast and clear liquids) | 6 |
BEDTIME PREANESTHETIC MEDICATION: Preoperative sedation can be given as ordered by the anaesthesiologist.
SPECIAL ORDERS:
- BLOOD TRANSFUSION
- VENOUS ACCESS HEMODYNAMIC MONITORING
- NG TUBE
- BLADDER CATHETER
- PREOPERATIVE HYDRATION
Postoperative Orders
Transfer: From recovery room to surgical ward when stable.
Vital Signs: q4h, I&O q4h x 24h.
Activity: Bed rest; ambulate in 6-8 hours if appropriate. Incentive spirometer q1h while awake.
Diet: NPO x 8h, then sips of water. Advance from clear liquids to regular diet as tolerated.
IV Fluids: IV D5 LR or D5 1/2 NS at 125 cc/h (KCL, 20 mEq/L if indicated).
Medications: (Specific medications would be listed here)
Postoperative day number 1
A. Assess the patient’s level of pain, lungs, cardiac status, flatulence, and bowel movement. Examine for distension, tenderness, bowel sounds; wound drainage, bleeding from incision.
B. Discontinue IV infusion when taking adequate PO fluids. Discontinue Foley catheter, and use in-and-out catheterization for urinary retention.
C. Ambulate as tolerated; incentive spirometer.
D. Consider prophylaxis for deep vein thrombosis.
For patients with limited mobility Encourage:
- Incentive spirometry to promote deep breathing and increase lung volume.
- Coughing to clear mucus from the airway.
- Promote deep breathing by teaching the patient to “splint” the chest and abdomen with a pillow when coughing or forcibly exhaling, by squeezing the pillow tightly against the abdomen or chest as a means of decreasing pain.
- A final step in the prevention of atelectasis and pneumonia is progressive and early ambulation.
Postoperative day number 2
- If passing gas or if bowel movement, advance to regular diet unless bowel resection.
- Laxatives: Dulcolax or Glycerin suppository prn or Fleet enema prn or milk of magnesia, 30 cc PO prn constipation.

Postoperative day number 3-7
A. Check pathology report.
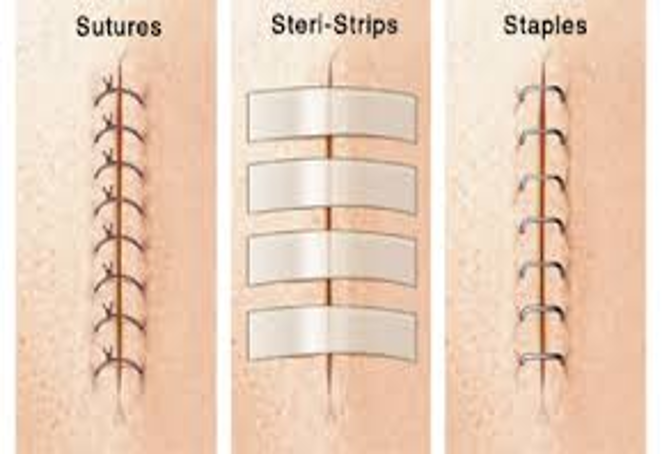
B. Remove staples and place steri-strips.
C. Consider discharge home on appropriate medications; follow up in 1-2 weeks for removal of sutures.
D. Write discharge orders (including prescriptions).
GENERAL COMPLICATIONS:
- IMPAIRED CONCIOUSNESS
- POSTOPERATIVE PYREXIA
- First 48hrs:
- Atelectasis
- Transfusion rxn
- Pre-existing infection
- 3-7 days: infections
- UTI, wound infection, pneumonia, anastomotic leakage
- 7 days onwards:
- Infections
- Abscess formation
- DVT/PE
- First 48hrs:
GASTROINTESTINAL COMPLICATION:
- POSTOPERATIVE ILEUS
- PROLONGED ILEUS AND INTESTINAL OBSTRUCTION
- GASTRIC DILATATION
- POSTOPERATIVE FECAL IMPACTION
- POSTOPERATIVE DIARRHEA
POSTOPERATION PAROTITIS: Acute bacterial suppurative parotitis is caused most commonly by Staphylococcus aureus and mixed oral aerobes and/or anaerobes. It often occurs in the setting of debilitation, dehydration, and poor oral hygiene, particularly among elderly postoperative patients.
URINARY COMPLICATIONS:
- POSTOPERATIVE URINARY RETENTION
- URINARY TRACT INFECTION
WOUND COMPLICATIONS:
- HEMATOMA
- SEROMA
- WOUND DEHISCENCE
- WOUND INFECTION

Risk factors in wound dehiscence
General
- Malnourishment
- Diabetes
- Obesity
- Renal failure
- Jaundice
- Sepsis
- Cancer
- Treatment with steroids
- Emergency surgery
Local
- Inadequate or poor closure of wound or closure of a wound under tension
- Poor local wound healing, e.g., because of infection, haematoma or seroma
- Increased intra-abdominal pressure, e.g., in postoperative patients with chronic obstructive airway disease, during excessive coughing
SURGICAL DRAINS
Passive drain
- Gauze drain
- Penrose drain
- Cigarette drain
Active suction drainZ Clinical case
- Sump drain
- Jackson Pratt drain
- Radivac drain
Corrugated Rubber Drain
Closed Suction Drain
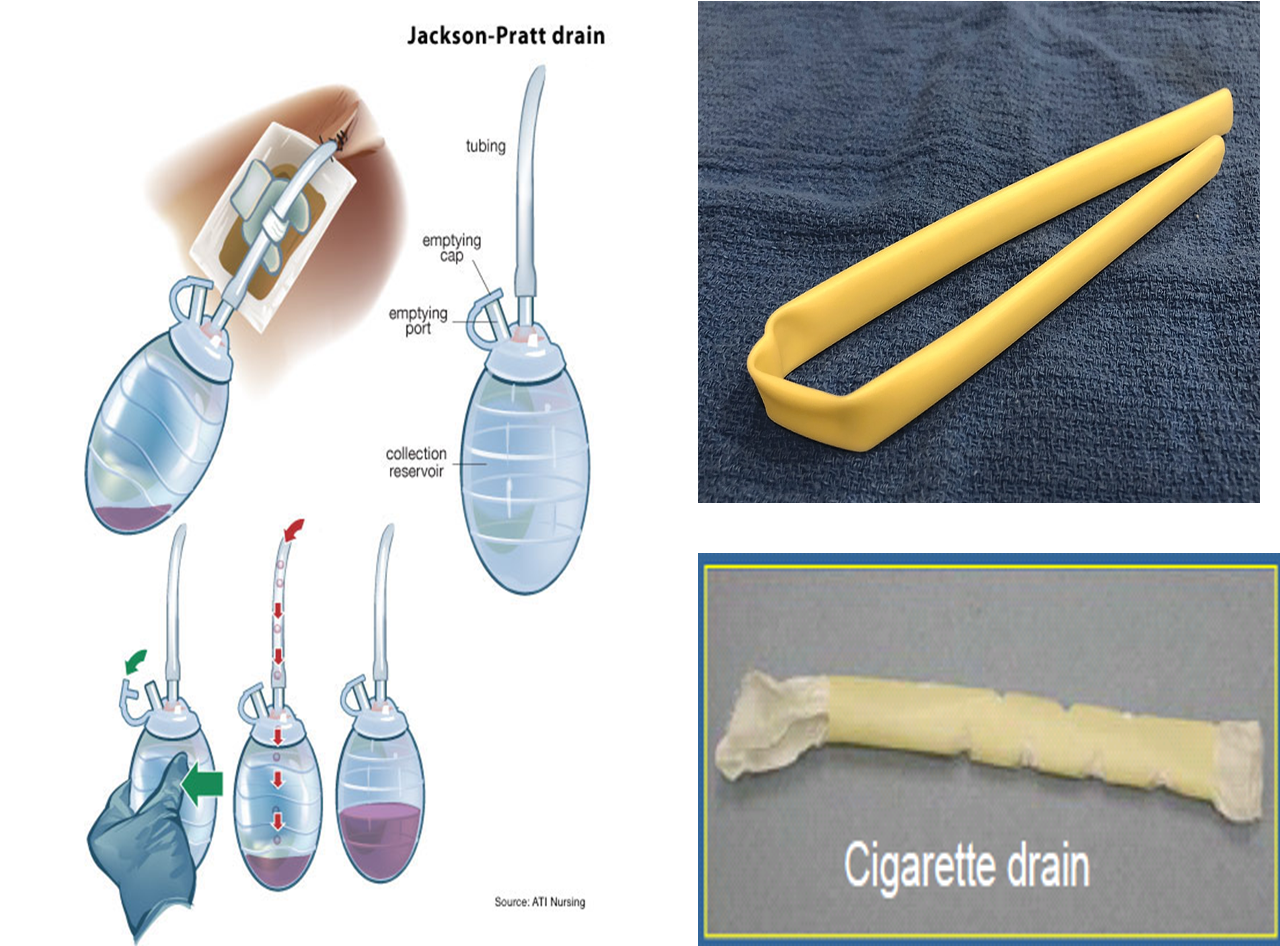
Corrugated rubber drain ospe