Case Station 1
A 35-year-old man with a known smoker presented with breathlessness on minimal exertion despite being prescribed inhaled salbutamol as required.
ILOs of station:
- Obtain an accurate focused medical history.
- Critically analyze clinical data obtained through history.
- Formulate and prioritize a differential diagnosis using reasoning skills
- Plan and approach management of different cases of asthma, COPD.
Student instruction:
please take a focused history from this patient.
Case scenario summary:
A 35-year-old man known case of chronic respiratory disease, presented with SOB.
Types of presentations
- Asthma,
- COVID,
- intestitial lung disseases; coal workers disease; long term disease -
- Even with salbutamol usage not helping, could be incorrect usage
Questions to ask
- Any past allergic reaction from specific food or compound?
- Cough?, Sputum?
- patient may complain of cough; cough variant cough asthma
- Sitting cough
- ask about common allergens in patients home; dust-carpets, mites, cats, birds, dogs
- if the attack perticipates in home/office ask about it, probe for cause
- Does anyone at home smoke?
- Some disease causes ILD; undigest fume compounds
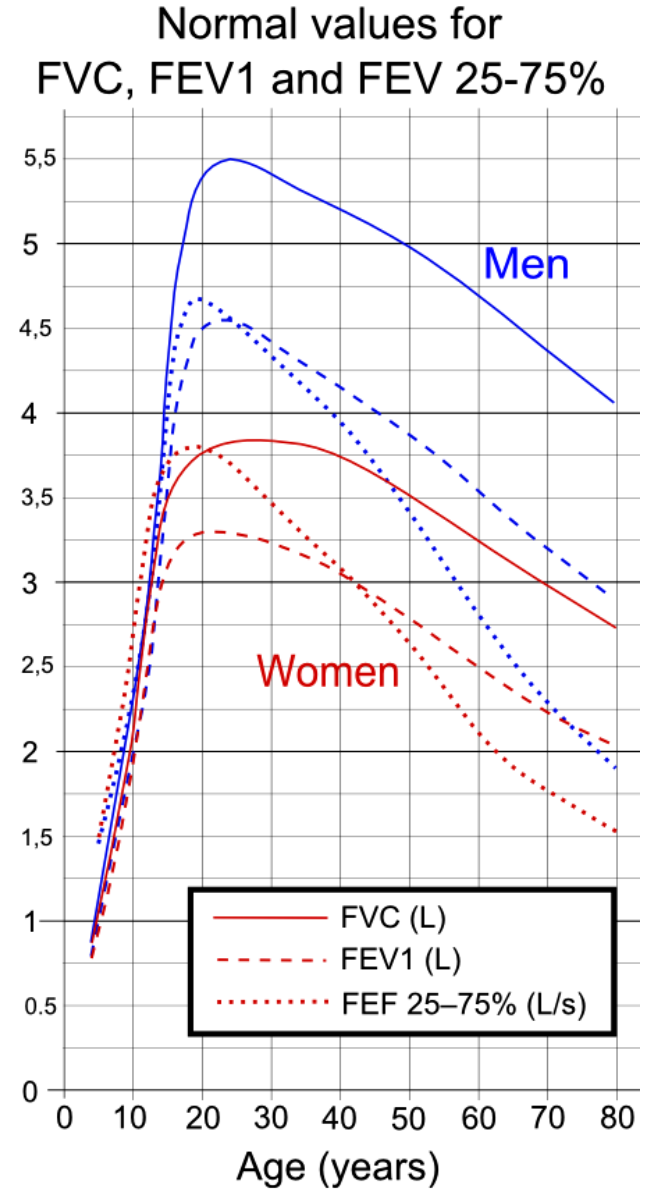
- Confusion could be make between asthma and copd in spirometry and cause of allergens outside factors that may mimics COPD in smokers
Treatment
- remove participating factors ⇒
- Beta-Agonist (more likely improvement in asthma rather COPD) ⇒
- corticosteroids (moderate to chronic asthma; wash to avoid oral candiasis)
- Epinephrine (Severe Asthma) ? cc
Auscultation
Usually Asthma; wheezing-constriction - in COPD; Crackles-air through liquid
Consultation
Ventilator Inflation = when pressed breath at same time with complete closure
Reference:
- Talley NJ. Clinical Examination: A Systematic Guide to Physical Diagnosis. 8th ed. New York: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2018. Page: 363-369.
- Kumar P, Clark M. Clinical Medicine. 10th ed. Philadelphia, PA: Elsevier; 2021. 412-413; 505-509
- Current Medical Diagnosis & Treatment 60th ed McGraw Hill, 2024 page 259-264
- https://youtu.be/XBq6hxGgyS4
- https://youtu.be/8MWwwNMn6dEA
Case Station 2
Physical examination station
Station title: Respiratory sounds
ILOs of the station: · Perform an accurate chest auscultation. · Critically analyze clinical data obtained through physical examination. · Formulate and prioritize a differential diagnosis using reasoning skills**.** · Formulate appropriate evidence-based patient, patient-centred management strategies.
Student instruction: please perform an appropriate chest auscultation.
Case Summary: Examination: Inspiratory crepitations and wheezes.
HPI
35 years old dm sob coughing weight loss for 3m
Inspection:
- Hand: clubbing, peripheral cyanosis, Palmar Erythema, Warm hands; carbon dioxide retention
- Chest: scars lobectomy-sternotomy, deformities; pectus excavitum/paricitum/pigion, movement of chest from depression, accessory muscles, CA Bronchus.
| Category | Finding | Possible Causes |
|---|---|---|
| Palpation | Tactile Fremitus | Increased: Consolidation (e.g., pneumonia) Decreased: Pleural effusion, pneumothorax, COPD |
| Expansion | Reduced on one side: Pneumothorax, pleural effusion, atelectasis, lung fibrosis | |
| Tracheal Deviation | Toward lesion: Atelectasis, lung collapse Away from lesion: Tension pneumothorax, large pleural effusion | |
| Percussion | Hyperresonance | Pneumothorax, emphysema, asthma |
| Resonance | Normal lung sound | |
| Dull | Consolidation (e.g., pneumonia), atelectasis, tumor | |
| Stony Dull | Large pleural effusion | |
| Auscultation | Wheeze | Asthma, COPD, bronchitis, foreign body obstruction |
| Stridor | Pediatric: Croup, epiglottitis, foreign body aspiration | |
| Pleural Rub | Pleuritis, pulmonary embolism, pneumonia |
Palpation
- tactitle fremitus
- expansion
- tracheal deviation
Percussion
- Hyperressonance
- Ressonance
- Dull
- Stony Dull
Auscultation
Wheeze - Stridor - pediatric patient , epiglottitis pleural rub -
Case Station 3
Procedural Skills/Communication Skills Station: Peak Flow Meter
Learning Objectives (ILOs) of the station:
By the end of this session, the student should be able to:
-
Set up and advise the patient on using a peak flow meter.
-
Communicate effectively with the patient while performing the procedure.
The student should cover:
-
Elicit the patient’s understanding of asthma and peak flow measurement.
-
Explain in clear and simple terms what the peak flow is measuring.
-
Perform accurately the peak flow meter technique.
-
Check whether the patient understood the process and ask him to demonstrate.
-
Interpret the results of the peak flow meter against the chart and advise the patient accordingly.
Student Instruction:
Please perform an accurate peak flow meter reading for a patient.
Case Summary:
Mr. Ahmed has presented to you with symptoms of daily nocturnal cough and a wheeze. He is a known asthmatic for the last 10 years on medication. He has frequent exacerbations and wishes to follow his asthma more closely at home. You suggest the use of a peak flow meter and want to advise him on it.
Peak flow meter
Used for monitoring
- Obstructive; partial obstruction of airway
put meter at zero hold from sides take full inspiration, seal fully, then forceful expiration in one blow use three times, then at maximum reading
if suspected attack, you should use it??
if less than 80% for step up management medication is done
Case
peak flowmeter, symptomps noctural cough and wheezing - known asthmatic 10 years medication
exarcbeate, wishes to follow asthma closer at home, suggested to peakflowmeter
References:
-
Medical Student Survival Skills: Procedural Skills, First Edition. Philip Jevon and Ruchi Joshi. Page 17-20. Companion website: www.wiley.com/go/jevon/medicalstudent
-
Medical Student Survival Skills: History Taking and Communication Skills, First Edition. Philip Jevon and Steve Odogwu. Companion website: www.wiley.com/go/jevon/medicalstudent