Pediatrics
Approach to Hemolytic Anemia
CLASSIFICATION OF HEMOLYTIC ANEMIAS
| Intra Corpuscular Defects | Extra Corpuscular Factors | |
|---|---|---|
| Hereditary | • Hemoglobinopathies • Enzymopathies • Membrane-cytoskeletal defects | • Familial hemolytic uremic syndrome |
| Acquired | • Paroxysmal nocturnal hemoglobinuria | • Mechanical destruction (microangiopathic) • Toxic agents • Drugs • Infectious • Autoimmune |
classification of haemolytic disorders
Inherited hemolytic disorders
-
Defects in the structure of the red cell membrane:
- Hereditary spherocytosis
- Hereditary elliptocytosis
- Hereditary stomatocytosis
-
Defects of erythrocyte metabolism:
- G6PD deficiency
- Pyruvate kinase deficiency
- Other enzyme disorders
-
Qualitative haemoglobin disorders:
- Stable variants, such as sickle cell disease
- Unstable variants
-
Quantitative haemoglobin disorders:
- Impaired globin chain synthesis
- Thalassaemias
Hemolytic Anemia Diagnosis
Two main principles:
- Confirm hemolysis
- Determine the etiology
The Key To The Etiology Of Hemolytic Anemia
- The history
- The peripheral blood film
How to diagnose hemolytic anemia
- New onset pallor or anemia
- Jaundice
- Splenomegaly
- Gall stones - Calciumbilirubinate stones
- Dark colored urine (hemoglobinuria)
- Leg ulcers (poor circulation and microinfarcts, healing is delayed and infection becomes established).
Patient History
- Acute or chronic
- Medication/Drug precipitants
- G6PD
- AIHA
- Family history
- Concomitant medical illnesses
- Clinical presentation
GENERAL FEATURES OF HEMOLYTIC DISORDERS
- General Examination: Jaundice, Pallor, Bossing Of Skull
- Physical Findings: Enlarged Spleen
- Hemoglobin: From Normal To Severely Reduced
- MCV: Usually Increased
- Reticulocytes: Increased
- Bilirubin: Increased [mostly Unconjugated]
- LDH: Increased
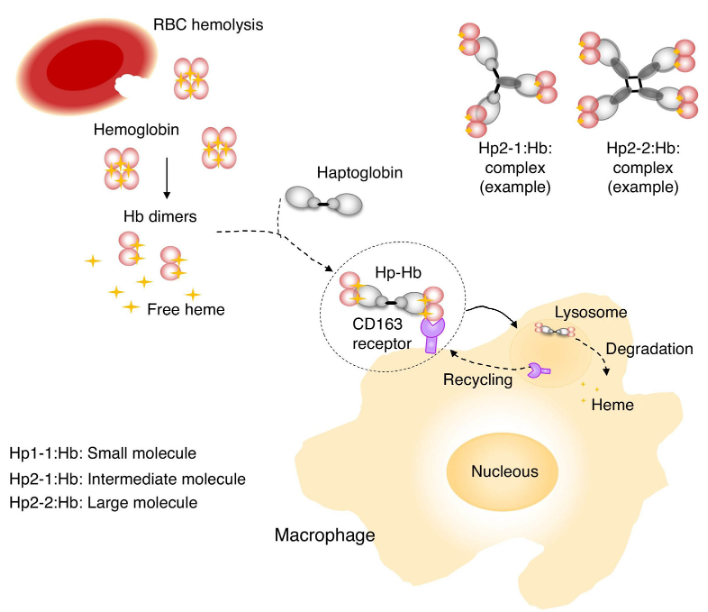
- Haptoglobulin: Reduced To Absent
Laboratory Diagnosis of Hemolytic Anemia:
Evidence for Red cell Destruction
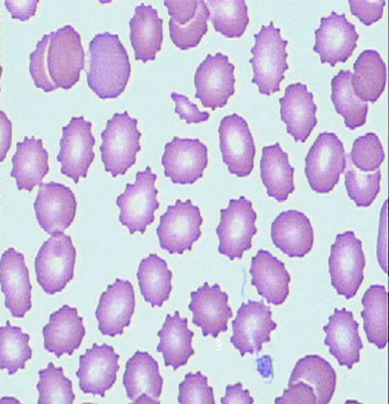
- i) PERIPHERAL BLOOD SMEAR → - Burr Cell - Tear drop cell (Intravascular Hemolysis) - Fragmented cell ⇒ Spherocytes - Spherocytes → H. spherocytosis - Malaria → Malaria parasite - Sickle cells → Sickle cell anemia
- ii) Plasma haptoglobin & Plasma hemopexin → ↓
- iii) Plasma Hb ↑
- iv) Serum LDH & Serum Carboxy Hb → ↑
- v) Indirect bilirubin & urobilinogin → ↑
- vi) Red cell survival → ↓ Using Chromium 52
Evidence of Red cell Generation:
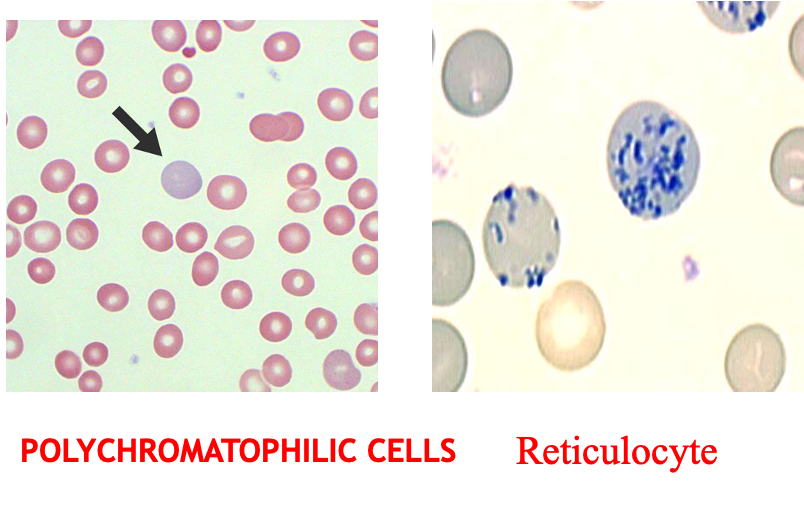
- Peripheral blood smear
- Polychromasia
- Nucleated red cells
- Reticulocyte count → ↑
Laboratory Evaluation of Hemolysis
| Laboratory Evaluation of Hemolysis | Extravascular | Intravascular |
|---|---|---|
| HEMATOLOGIC | ||
| Routine blood film | Polychromatophilia | Polychromatophilia |
| Reticulocyte count | ↑ | ↑ |
| Bone marrow examination | Erythroid hyperplasia | Erythroid hyperplasia |
| PLASMA OR SERUM | ||
| Bilirubin | Unconjugated ↑ | Unconjugated |
| Haptoglobin | ↓, Absent | Absent |
| Plasma hemoglobin | N/↑ | ↑↑ |
| Lactate dehydrogenase | ↑ (Variable) | ↑↑ (Variable) |
| URINE | ||
| Bilirubin | + | + |
| Hemosiderin | 0 | + |
| Hemoglobin | 0 | + → severe cases |
FM
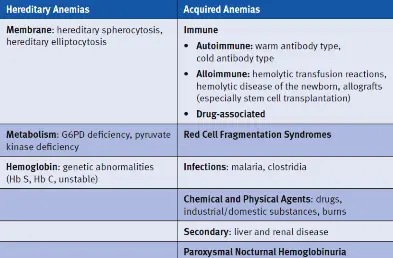
Hemolytic Anemia
Hereditary Anemias
- Membrane: hereditary spherocytosis, hereditary elliptocytosis
- Metabolism: G6PD deficiency, pyruvate kinase deficiency
- Hemoglobin: genetic abnormalities (Hb S, Hb C, unstable)
Acquired Anemias
-
Immune:
- Autoimmune: warm antibody type, cold antibody type
- Alloimmune: hemolytic transfusion reactions, hemolytic disease of the newborn, allografts (especially stem cell transplantation)
- Drug-associated
-
Red Cell Fragmentation Syndromes
-
Infections: malaria, clostridia
-
Chemical and Physical Agents: drugs, industrial/domestic substances, burns
-
Secondary: liver and renal disease
-
Paroxysmal Nocturnal Hemoglobinuria
Definition
-
A group of disorders leading to anemia caused by a reduction in red cell life span.
-
RBC’s normally survive 100 - 120 days.
-
Bone marrow has the capacity to increase erythropoiesis 6 - 8 times than normal.
-
Anemia is the result of premature destruction of red cells exceeding the erythropoietic capacity of the bone marrow.
Clinical Manifestations of Hemolytic Anemia
-
Onset may be acute or insidious
-
Symptoms and signs of anemia
-
Jaundice
-
Symptoms and signs specific to the type of hemolytic anemia
-
Symptoms related to the underlying disease
-
Splenomegaly
-
Cholelithiasis (gall stones) symptoms
-
Leg ulcers (sickle cell, spherocytosis)
-
Skeletal abnormalities (thalassemia)
-
Crises (chronic hemolytic disease)
- Aplastic crises
- Hemolytic
- Megaloblastic
-
Changes in urine color
Laboratory Findings
I- Increased RBC Destruction
- Decreased RBC life span
- Increased haem(heme) catabolism
- Increased serum LDH
- Absence or decrease of serum haptoglobin
- > 1 g /dl /week fall in blood Hb level
- Reduced glycosylated Hb
- Signs of intravascular hemolysis
- Hemoglobinemia
- Hemoglobinuria
Treatment
-
The principal form of treatment is splenectomy although this should not be performed unless clinically indicated because of anemia.
-
Splenectomy lengthens the life span of red cells, corrects anemia, prevents haemochromatosis, but does not affect the character of red cells.