Definition
Diarrhea is defined as the passage of three or more loose or liquid stools per day (or more frequent passage than is normal for the individual). Frequent passing of formed stools is not diarrhea, nor is the passing of loose, “pasty” stools by breastfed babies. Acute diarrhea lasts less than 14 days.
Causes of Diarrhea Deaths
Diarrheal disease is the second leading cause of death in children under five years old. Causes of death include:
- Severe dehydration and fluid loss.
- Septic bacterial infections.
Children who are malnourished or have impaired immunity, as well as people living with HIV, are most at risk of life-threatening diarrhea.
Complications of Acute Diarrhea
- Dehydration and electrolyte imbalance.
- Persistent diarrhea.
- Lactose intolerance.
- Malnutrition.
Clinical Types of Diarrhea
- Acute watery diarrhea – lasts several hours or days, and includes cholera.
- Acute bloody diarrhea – also called dysentery.
- Persistent diarrhea – lasts 14 days or longer.
Causes of Diarrhea Z
Infection in the Intestinal Tract
- Rotavirus is the most common cause of acute childhood diarrhea, usually resolves in 3-9 days.
- Other common viruses: Adenovirus, norovirus, and astroviruses.
- Bacteria: Campylobacter, salmonella, shigella, and E. coli.
- Parasites: Giardia and entamoeba histolytica cause chronic diarrhea and less commonly acute diarrhea.
Malnutrition
- Makes children more vulnerable to diarrhea.
- Each diarrheal episode worsens malnutrition.
- Children who die from diarrhea often suffer from underlying malnutrition.
- Diarrhea is a leading cause of malnutrition in children under five years old.
Other Causes
- Person-to-person spread, aggravated by poor personal hygiene.
- Food prepared or stored in unhygienic conditions.
- Unsafe domestic water storage and handling.
- Fish and seafood from polluted water.
- A significant proportion of diarrheal disease can be prevented through safe drinking-water and adequate sanitation and hygiene.
Classification According to Mechanism of Diarrhea
-
Osmotic Diarrhea:
-
Due to non-absorbable solutes in the gut, e.g., lactose intolerance.
-
Caused by excessive sugar or salt solutions drawing water into the bowel.
-
Result of maldigestion (e.g., pancreatic disease or celiac disease).
-
Caused by osmotic laxatives.
-
In healthy children, too much magnesium, vitamin C, undigested lactose can cause osmotic diarrhea.
-
Lactose intolerance, fructose malabsorption cause osmotic diarrhea.
-
Osmotic diarrhea will stop when the offending agent (e.g., milk or sorbitol) is discontinued.
-
-
Secretory Diarrhea:
-
Activation of intracellular mediators (cAMP, cGMP, and calcium), e.g., Cholera & E. coli enterotoxins.
-
Congenital defects of Na-H exchange, Cl-HCO3 exchange, and Na-bile acid transport proteins (secretory diarrhea presenting at birth), e.g., Congenital chloride diarrhea.
-
Increase in active secretion or inhibition of absorption.
-
Little to no structural damage.
-
Most common cause is cholera toxin stimulating secretion of anions, especially chloride ions.
-
Intestinal fluid secretion is isotonic with plasma even during fasting.
-
Continues even when there is no oral food intake.
-
-
Inflammatory (Mucosal Damage) Diarrhea:
-
Bacterial, viral, parasitic infections.
-
Damage to the mucosal lining or brush border leads to passive loss of protein-rich fluids and decreased ability to absorb these lost fluids.
-
Features of other types of diarrhea can be found in this type.
-
Caused by bacterial, viral, parasitic infections, or autoimmune inflammatory bowel disease.
-
Other causes include tuberculosis, colon cancer, and enteritis.
-
- Exudative Diarrhea
- Occurs with the presence of blood and pus in the stool, e.g., Crohn’s disease or Ulcerative colitis and other severe infections such as E. coli.
- Dysentery
- Shigella is the most common cause of dysentery (gross blood in the stool is the hallmark of dysentery and may be accompanied by abdominal cramps and fever).
- Other causes include Entamoeba Histolytica and salmonella.
| Type of Diarrhea | Mechanism | Causes | Characteristics | Resolution |
|---|---|---|---|---|
| Osmotic Diarrhea | Due to non-absorbable solutes in the gut. | - Lactose intolerance, fructose malabsorption - Excessive sugar or salt solutions - Maldigestion (e.g., pancreatic disease, celiac disease) - Osmotic laxatives - Excess magnesium, vitamin C | - Water drawn into bowel - Stops when offending agent is removed - Common in healthy children | Stops when the offending agent (e.g., milk, sorbitol) is discontinued. |
| Secretory Diarrhea | Activation of intracellular mediators (cAMP, cGMP, calcium). | - Cholera & E. coli enterotoxins - Congenital defects (e.g., Na-H exchange, Cl-HCO3 exchange) - Congenital chloride diarrhea | - Increase in secretion or inhibition of absorption - Isotonic fluid secretion - Continues fasting | Continues even when there is no oral food intake. |
| Inflammatory Diarrhea | Damage to mucosal lining or brush border. | - Bacterial, viral, parasitic infections - Autoimmune inflammatory bowel disease - Tuberculosis - Colon cancer - Enteritis | - Passive loss of protein-rich fluids - Decreased absorption ability - Features of other diarrhea types | Depends on treatment of underlying infection or condition (e.g., antibiotics, anti-inflammatory drugs). |
Classification According to Age of Onset
At Birth or in 1st 24 Hours of Life After the First Feeding
- Congenital chloride diarrhea (history of polyhydramnios).
- Congenital lactase deficiency.
Early Onset (Before 3 Months of Age)
- Cow’s/soy milk allergy (blood streaks & emesis, +ve WBC in stool).
- Malrotation/volvulus (emesis + diarrhea, malabsorption/protein loss).
- Secondary lactase deficiency: watery, acidic (fermentation), sugar-containing stools.
- Infectious (rotavirus, salmonella) manifested with fever, crampy abdominal pain, blood/mucous in stool.
Onset by 3 Months to Preschool Age
- Toddler’s diarrhea (normal growth, no malnutrition, no dehydration).
- Celiac Disease.
- Cystic Fibrosis.
Onset in Later Childhood & Adolescence
- Infections and post-infections.
- Juices.
- Crohn disease and ulcerative colitis.
| Age of Onset | Condition | Symptoms/Characteristics |
|---|---|---|
| At Birth or in 1st 24 Hours | Congenital chloride diarrhea | History of polyhydramnios. |
| Congenital lactase deficiency | Symptoms appear after the first feeding. | |
| Early Onset (Before 3 Months) | Cow’s/soy milk allergy | Blood streaks & emesis, positive WBC in stool. |
| Malrotation/volvulus | Emesis + diarrhea, malabsorption/protein loss. | |
| Secondary lactase deficiency | Watery, acidic (fermentation), sugar-containing stools. | |
| Infectious (rotavirus, salmonella) | Fever, crampy abdominal pain, blood/mucous in stool. | |
| Onset by 3 Months to Preschool Age | Toddler’s diarrhea | Normal growth, no malnutrition, no dehydration. |
| Celiac disease | Symptoms may include malabsorption and growth issues. | |
| Cystic fibrosis | May present with malabsorption and respiratory symptoms. | |
| Onset in Later Childhood & Adolescence | Infections and post-infections | Various gastrointestinal symptoms depending on the infection. |
| Juices | Can cause diarrhea due to high sugar content. | |
| Crohn disease and ulcerative colitis | Chronic inflammation, abdominal pain, diarrhea, possible blood in stool. |
Diagnosis
History
- Age of onset: e.g., early onset suggests congenital/genetic disorders.
- Relationship to dietary changes: e.g., Secretory will not stop if NPO.
- Nature of stool: e.g., foul smell, greasy in fat malabsorption.
- Associated symptoms: e.g., arthritis/skin lesion in IBD.
- Exposure: e.g., family, daycare, or travel in infection by Giardia.
- Past health: e.g., antibiotic, surgery of bowel.
- Family history: e.g., protein intolerance, CF, Celiac disease, IBD.
Physical Examination
- General nutrition & growth: poor growth.
- Vital signs: Hypertension (tumor secretory catecholamines; pheochromocytoma), fever, hydration.
- Abdominal exam: Abd. Mass, Abd. Distension, Organomegaly, Abnormal Genitalia, (Perianal tags/fistulae; crohns), (Rectal prolapse; cystic fibrosis).
- Additional findings: edema, Pallor, jaundice, rash, wheezing, clubbing, Iritis, and arthritis.
- Neurological exam: Ataxia, hyporeflexia.
Investigations for Acute Diarrhea
-
Blood tests: CBC, ESR, Electrolytes, BUN, and creatinine.
- LFT.
-
Stool exam: pH, Reducing substances (disaccharide) , Smear for WBC, fat, ova & parasites, Occult blood.
- Stool cultures.
Diagnostic Approach
The following types of diarrhea may indicate further investigations:
- Diarrhea since birth.
- Moderate or severe diarrhea in infants or young children.
- Associated with blood.
- Continues for more than 3 days.
- Associated with non-cramping abdominal pain, fever, weight loss.
- In travelers.
- In food handlers (the potential to infect others).
- In institutions (hospitals, childcare centers).
- Suspected celiac disease or inflammatory bowel disease.
- Failure to thrive.
Management
- In many cases, replacing lost fluid and salts is the only treatment needed (Oral rehydration therapy or intravenously). - simple gastroenteritis, dont give anti diarrhea emetics
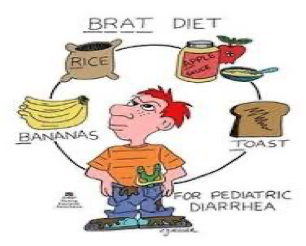
- Diet restrictions such as the BRAT diet (for 2 days only). (bananas,toasts,rice,apple)
- Research does not support the limiting of milk to children (no effect on the duration of diarrhea).
Treatment
- Zinc supplements for 10-14 days reduce the duration of a diarrhea episode by 25% and are associated with a 30% reduction in stool volume.
- Nutrient-rich foods: the vicious circle of malnutrition and diarrhea can be broken by continuing to give nutrient-rich foods – including breast milk – during an episode and by giving a nutritious diet to children when they are well.
- Management of persistent diarrhea or when there is blood in stool.
Prevention
- Safe drinking-water.
- Use of improved sanitation.
- Hand washing with soap can reduce disease risk.
- Exclusive breastfeeding for the first six months of life.
- Good personal and food hygiene.
- Health education about how infections spread.
- Rotavirus and Cholera vaccination.
- Probiotics decrease the risk of diarrhea in those taking antibiotics.