Scabies
Introduction
- Scabies is an intensely pruritic skin infestation
- A source of human infestation for thousands of yrs (2500 yrs, Roman times)
- The term scabies is derived from Latin word scabere (to scratch).
- Prevalence rates are higher in children and sexually active individuals than in other persons.
- Caused by the host-specific mite, Sarcoptes scabiei var hominis. Is an obligate human parasite
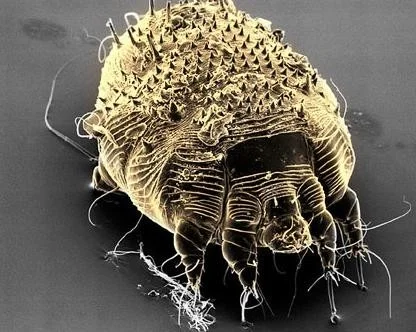
Scabies mite

Pathophysiology
- Transmission is via direct and prolonged contact with an infected individual (not via inanimate objects)
- The entire life cycle of the mite lasts 30 days and is spent within the human epidermis.
Pathophysiology
- After copulation, the male mite dies and the female mite burrows into the superficial skin layers
- Once on the skin, fertilized female mites burrow through the stratum corneum at the rate of about 2 mm per day, and produce two or three oval eggs each day (total of 60-90 eggs).
- The ova require 10 days to 3 weeks to become mature adult mites

-
Mites move through the top layers of skin by secreting proteases that degrade the stratum corneum.
-
They feed on dissolved tissue
-
Scybala (feces) are left behind as they travel through the epidermis, creating linear lesions clinically recognized as burrows.
-
Upon initial infestation, a delayed type IV hypersensitivity reaction to the mites, eggs, or scybala develops over 4-6 weeks.
-
The hypersensitivity reaction is responsible for the intense pruritus that is the clinical hallmark of the disease.
Clinical features
Distribution of the lesion differs in adults and children. Adults • Lesions manifest primarily on the flexure aspects of the wrists, the interdigital web spaces of the hands, and genitalia.
Infants and children
- Lesions can appear any where and any site may be involved.
- The diagnosis of scabies is considered in any patient presenting with a recent onset of intense itching that is accentuated at night.
- Similar symptoms in close contacts should immediately rank scabies at the top of the clinical differential diagnosis.
General Presentation
Clinical Types
- Classical
- Crusted
Crusted scabies (immunocompromised)
– Syn: Norwegian, scabies (so named because the first description was from Norway in the mid-1800s) – Is a highly contagious form of the disease. – Hundreds to millions of mites infest the host individual, – Usually immunocompromised, elderly.
Management
-
Treatment includes administration of :
- Scabicidal agents
- Antipruritic agent (e.g.sedating antihistamine)
- Antimicrobial agent if secondarily infected
-
All family members and close contacts must be evaluated and treated,
-
All clothing, bed linens, and towels used within the last week to be launder in hot water the day after treatment and again in 1 week.
-
Application of topical antiscabietic agents, with repeat application in 7 days. These include:
- Permethrin 5% cream is the drug of choice, especially for infants >2 mo and small children
- Lindane1% lotion or cream
- Sulfur 6% in petrolatum
- Crotamiton (Eurax)10% cream or lotion for treatment of scabies
-
An oral agent, ivermectin is proved to be effective
-
Dose of 200-250 mcg/kg given at diagnosis and repeated in 7-14 days.








Case Two
Case Two: History
- HPI: S is a 21-month-old boy who was referred to the dermatology clinic for a rash that has been present for two weeks. The itch has disturbed his sleep.
- PMH: no chronic illness or hospitalizations
- Allergies: no known drug allergies
- Medications: none
- Family history: noncontributory
- Social history: lives with his parents and attends day care
- ROS: negative
Case Two: Skin Exam
- Multiple erythematous papules on the trunk, extremities and genitals.
- Burrows present in the 2nd-3rd web space on the right hand.

Case Two: Question 1
- What in-office procedure would best help to confirm the diagnosis? a. KOH preparation (commonly used to diagnosis fungal infections of the skin) b. Nail clipping (commonly used to diagnosis onychomycosis) c. Skin scraping (mineral oil preparation) d. Wood’s lamp examination (commonly used to assess the degree of pigment in the skin)
Case Two: Question 2
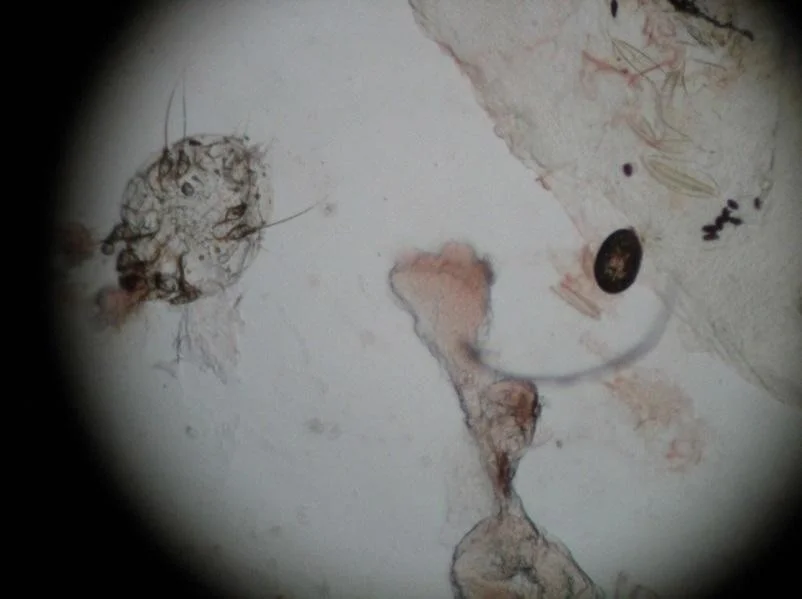
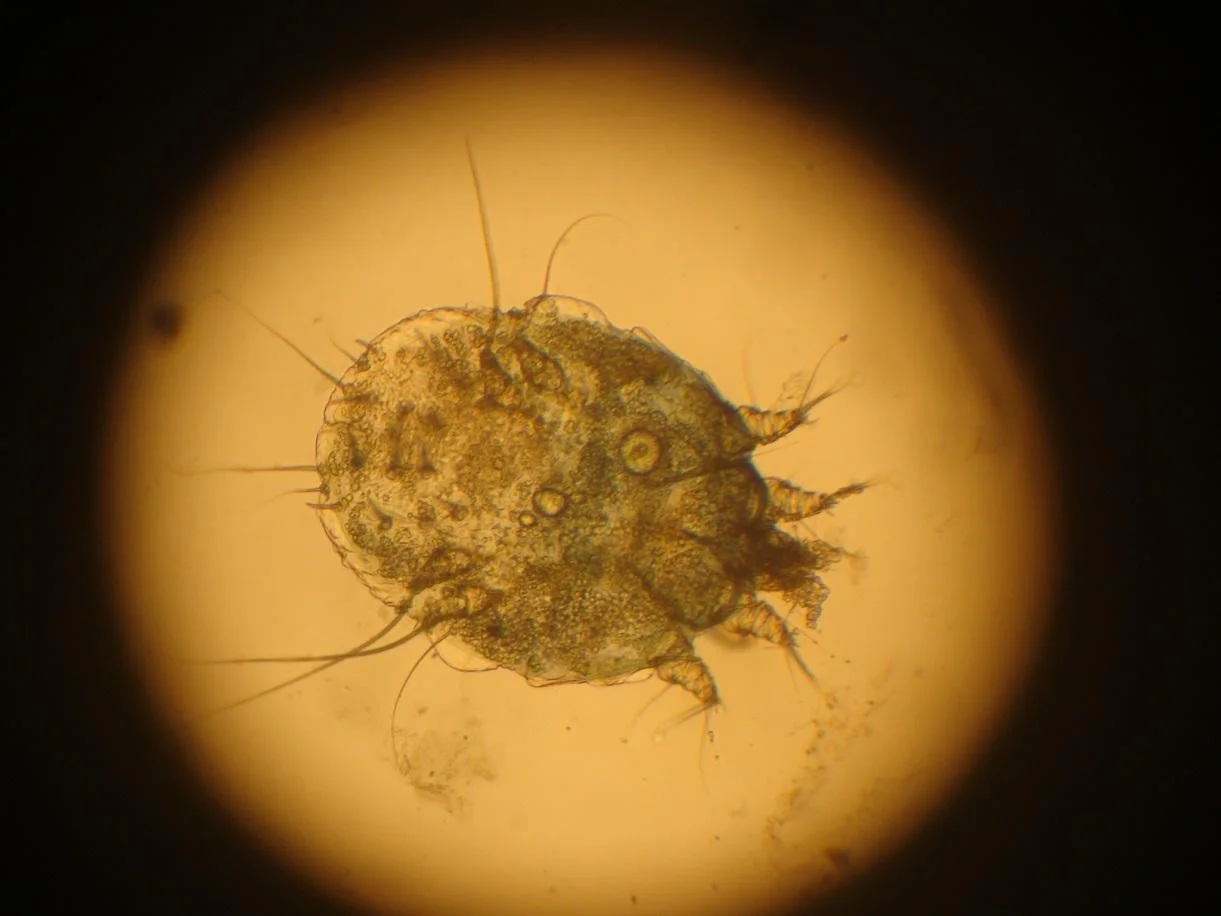
- You perform a mineral oil preparation on the patient.
- You use a 15-blade scalpel and scrape a burrow on the skin. The scraped material is placed on a slide and a drop of mineral oil is added. A cover slip is placed on top and you see the image below when you look through the microscope.
- What do you see?
- scabies mite
- egg
- scybala (feces)
Scabies
-
Sarcoptes scabiei (scabies) affects patients of all ages and all socioeconomic classes, although it is more common in women and children.
-
Immunocompromised individuals and those in congregated facilities (e.g., nursing homes) are more prone to infestation.
-
Most infections occur from direct contact with an infected individual; however, fomites can transmit infection.
Scabies: Clinical Features
-
The time from initial infestation to symptoms is typically 3-4 weeks.
- Once sensitized to the mite, re-infestation results in symptoms within 1-2 days.
-
Papules may commonly involve the axillae, breasts, umbilicus, penis, scrotum, finger webs and wrists.
-
The scalp and head are more frequently involved in infants, elderly and immunosuppressed individuals.
-
The hallmark feature is itching at night.
Scabies: Clinical Findings


Scabies Mite
- The scabies mite is 0.35 x 0.3 mm in size and too small to be seen by the naked eye.
- Females lay about three eggs per day, which hatch in four days.
- Most patients have less than 20 mites on the skin at a time.
Case Two: Question 3
- Which of the following clinical findings is considered pathognomonic for scabies? a. Burrows b. Diffuse involvement (may be diffuse, especially in infants) c. Erythematous papules (this primary morphology is not specific to scabies infestation) d. Sparing of the groin (genital involvement is common)
Burrows
- Burrows are linear markings in the skin due to the movement of the mite. They are 1-10 mm in length and are most readily found in the interdigital spaces, wrists and elbows.

Burrows
Dermoscopy helps identify the mite at the end of a burrow


Case Two: Question 4
S’s mother tells you his uncle, who is HIV+, is currently hospitalized. Why is this important? a. His uncle is unlikely to have been the source of infestation (Immunosuppressed patients are at increased risk for infestation) b. If his uncle has scabies, it could cause an institutional outbreak c. If his uncle gets scabies, it will likely be a less severe form (Immunosuppressed patients may develop crusted scabies) d. This is not relevant information
Crusted Scabies
-
Immune suppressed or neurologically impaired individuals are at increased risk of developing crusted scabies (hyperkeratotic scabies, formerly called Norwegian scabies).
- Presents with thick, scaly, white-gray plaques with minimal pruritus that is often localized to the scalp, face, back, buttocks and feet.
- Fissures provide an entry for bacteria leading to increased risk of sepsis and death.
- Immunocompetent persons who come into contact with crusted scabies develop typical scabies.
-
Crusted scabies is far more difficult to treat.
-
There is an incredibly high mite burden.
-
Refer to the HIV Dermatology module for more information on crusted scabies.

Treatment
-
Scabies treatment includes a two-pronged approach.
-
The patient and the environment must both be treated.
- Two topical treatments separated one week apart with a prescription anti-scabietic medication are recommended.
- Apply topical medication from the neck down and leave on overnight; for infants and the elderly, include the face and scalp.
-
Itch and lesions can persist for 2-4 weeks after successful treatment, referred to as “post-scabietic” pruritus or dermatitis.
- This is not a treatment failure, rather it represents the body’s response to dead mites.
-
Environmental care includes washing all clothing and linens used within the last week in hot water and drying on high heat.
-
For items that cannot be washed, seal items in bags for at least 3 days.
-
Isolation from other people is unnecessary as the causative organism cannot jump or fly, and can survive for o
First-line Treatments
- 5% permethrin cream • Topically overnight on days 0 and 7. Apply from neck down. Include scalp and face in infants and elderly.
- precipitated sulfur, 5-10% • Apply overnight for three days, then wash off
- Oral ivermectin • 200 mcg/kg by mouth, repeat dose two weeks later