Quinolones
| Drug | Uses |
|---|---|
| Naldixic | narrow |
| Cipro/Nor | - Ve; P. Aeru, E. Coli, Sal. Typhi |
| Levo | + Ve superficials CAP S. Pneu |
| Moxi | + Ve Anerobes S. Pneu |
| DNA GYRASE Supercoiling process |
- QTc, Crystal, Pseudo colitis, arthro/cns/photo toxicity
Folate Antagonists - all statics except TMP/SMX
| Drug | Uses | MOA | Side Effects |
|---|---|---|---|
| Sulphonamides lsulfasalazine Diazine/Mylon | Burn, Ocular Infections, IBD; UC | Glomerular Filteration - high binding serum albumin | Crystal, SJS, G6PD, Kernicterus |
| Trimethoprim | UTI’s ,Prostatitis, Vaginitis - though Quinolones are preffered | weak base - more potent | F.A. deficiency Teratogenic |
| Dapsone | Leprosy, Pneumocystis carinni, dermatites herpetiform | More tolerable than TMP/SMX | Hemolysis, Lepra reaction - managed by cortico & or Thalidomide |
| TMP/SMX trimethoprim & S. methoxazole | Proph & Treat UTI’s, Pneumocystitis Jirovecci; hiv aid - MRSA | increased synnergism | Crystal - True/Pseudo renal failure |
- sulfadiazine & pyrimethamine (dihydrofolate reductase inhibitor) is the preferred treatment for toxoplasmosis.
- Sulfadoxine, pyrimethamine is used as an Anti-Malarial drug. Antifolate; (pyremethamine,progunail,Sulphonamides): Treatment of acute attack of chloroquine resistant P.falciparum in combination with Quinine - Chemoprophylaxis in chloroquine resistant P.falciparum
Beta-lactams
Non- Beta-lactams
| Drug | MOA___________// | Uses | side effects |
|---|---|---|---|
| Fosfomycin | Broad - one dosage Last resort | E. coli, K spp Proteus, Pseudomonas & VRE | superinfection |
| Bacitracin | Prevent cell wall synthesis | +Ve - some -ve mixed with polymyxin-b & neomycin | Nephrotoxicity |
| Cycloserine | D-alanine Inihibt cell wall syntheesis | Coliforms/Mycobacteria 1st line anti-tuberculous | Nervous toxicity convulsions psychosis |
| Vancomycin | D-ala-D-ala - prevents elongation | +Ve only - pseudomembranous colitis, MRSA, Streptococci bacillus anthracis | - Ototoxicity -Red neck syndrome |
| Dalb & Orita vancin’s | Long action - IV-2wks | MRSA & Streptococci - skin | |
| Telavancin | V failed response - lipoglyco | MRSA - interacts w/ cell membrane | red neck ototixicity + taste disturb foamy urine |
| Daptomycin | binds cell membrane - leak ions | I.V. VRE/MRSA/STAPH ENDOCARDITIS | Renal insufficiency, CK, Eosinophilic Pneumonia |
| Fidaxomicin | ribosomal protein synthesis inhibitor that is bactericidal. It is classified as a macrolide , but unlike other macrolides, it is not absorbed in the GI tract and is able to kill susceptible organisms | Clostridium deficille spares normal flora | anemia, neutropenia, hypersensitivity macrolide sensitivity |
| Bezlotoxumab | monoclonal antibody that binds to toxin B produced by C difficile inactive, decreasing the risk of recurrent infections. | Clostridium deficille spares normal flora | |
| Mupirocin | Compete w/ isoleucine binding TRNA synthesase to stop bacterial protein | + Ve - MRSA & Impetigo cream also s.pyogen/hemolytic streptococci | |
| Polymyxins | outer membranes - leakage of content | Bladder irrigant skin/eye/ear w/ Neo & Genta micin’s | Nephro/Neuro/ Respiratory toxicity |
Anti-Ribosomal 30s - Amino glycosides
| Drug | Uses |
|---|---|
| streptomycin | TB meningitis (intrathecal) - mix Pen-G or Ampicillin - Step. Viridans Enterococcal Endocarditis with known vavular disease - Septecemia w/ Benzyl Pen. or metrondiazole if Peritonitis mainly prophylaxis |
| Neo/Gentamycin | Topical: mixture Polymixins & Bactiracin w/ cortico’s Orally: Intestine sterile bacillarry dysentery watery diarrhea hepatic coma Plaque, Tuleremia, Brucellosis |
| Tobra | Pseudomonas - genta resistance |
| Amikacin Netilmicin | Broad but less potent - genta resistence |
| Paromo | Intestinal Amoebiasis - Like neomycin |
| Spectino | N. gonorrhoea after failed penicllin |
| Plazo | If an aminoglycoside is required for treatment of tuberculosis or other mycobacteria, amikacin is now the preferred agent. |
| CMAX - MIC - PAE Effects - poor intestinal absorption - primarily kidney - can cross placenta cause congenital deafness |
Resistance to aminoglycosides occurs via:
- Efflux pumps.
- Decreased uptake, and/or
- Modification and inactivation by plasmid associated synthesis of enzymes. Each of these enzymes has its own aminoglycoside specificity; therefore, cross-resistance cannot be presumed.
Adverse Effects: (Narrow Index)
Nephrotoxicity, ototoxicity, never mix with cephalosporins, minoglycosied, penicillins for pseudomonals, Furosemide, Mannitol, histamines
Other Anti-Ribosomal 30s
| Drug | MOA | Uses | Side effect |
|---|---|---|---|
| **Tetracyclines; ** Oxy Tetra Doxy | static but broad - prevent bind trna to MRNA chelates Ca, Mg, Mn food dont impair - supplements could Bile concetration | white spots acne & CSF for Mino & Doxy Cholera 1st choice | Epithelial surface disorder due vit b12 disturbance Yellow staining teeth - bones, hepatotoxicity, phototoxicity, PSEUDOTUMOR CEREBRI |
| Glyclycyclines: Tigecycline | static & broad | It is indicated for parenteral treatment of complicated skin and soft tissue infections, complicated intra-abdominal infections in adults. MRSA, VRE, ESBL bad for proteus/ pseudomonas | pancreatitis, including fatality, has been reported with therapy - decrease the clearance of warfarin and increase prothrombin time |
Action on 50s Subunit: Macrolides & Ketolides
| drug | MOA depends on dosage | Uses | Side effects |
|---|---|---|---|
| Calithromycin | similar to eryhtromycins | Toxoplasma & H. Pylori in Peptic ulcer H. influenza | |
| Azithromycin | Concretion in Respiratory - combined with macrolide regimen such clarithro | Pelvic infection, urethritis, cervicitis, chlamydia & gonococci | |
| Telithromycin | similar to that of azithromycin | Mild-moderaite CAP chronic bronchitis acute bacterial sinusitis | possible liver damage - CYP3A enzyme not used in mysthenia gravis |
| Prevac | Clarithromycin is a key component in the treatment of H pylori– induced GI ulcer disease in combination with other drugs and acid-suppressive agents | peptic ulcer disease & H pylori In addition to clarithromycin and lansoprazole, it contains amoxicillin | Screening for both beta-lactam allergies and drug interactions is important |
| It is a second line drug for the treatment of gonorrhea and syphilis | |||
| and also Treatment of middle ear and sinus infections , since the causative agents, H. influenza and Strep. pneumonia are usually sensitive |
-
pregfnancy safe - metabolized in liver & low renal
-
Ototoxicity CYP 450 inhibition - cholestatic jaundic/hepatitis, Prolong QTc
Interactions
- Combination of the therapeutic dose of (Erythromycins) Macrolides with Penicillin antagonizes penicillin bactericidal effect.
- Erythromycin, telithromycin, and clarithromycin inhibit the hepatic metabolism of a number of drugs, which can lead to toxic accumulation of these compounds
- An interaction with digoxin may occur. In this case, the antibiotic eliminates a species of intestinal flora that ordinarily inactivates digoxin, thus leading to greater reabsorption of the drug from the enterohepatic circulation
Other Anti-Ribosomal 50s
| drug | MOA | uses | Side effects |
|---|---|---|---|
| Chloraphenicol | broad - static rapid metabolism crosses placenta and BBB Renal tubular & glomerular | H. influenzy for bone diseases - severe anearobic resistance B-fragilis can be used topically for ear nad eye used only if all failed with resistance | Marrow depression Grey baby syndrome Superinfections Optic Neuritis & encelaphopathy inhibit lvier microsomal enzyme |
| Lincosamids/ Clinda & Linda mycins | high conctreation to skin, bone - intraabdominal infections + septic tract infections | B.fragilis anerobic infection Malaria in combination to treat bacterial vaginosis and prophylaxis of bacterial endocarditis | pseudomembranous colitis |
| Quinupristene, Dalfopristin, ((Linezolid)) | inhibition 50s - cidal effect - combination | MRSA, VRE | Hyperbillirubinemia - CYP3A4 isoenzyme p450 |
| Fusidic acid | 50s | Topical - bone pus, gram + - diplococci, staphylcoccal conjunctivitis | skin eruption, jaundice, |
Important
| Antibiootic | MOA | Spectrum +++ | Uses | Side Effects |
|---|---|---|---|---|
| Bacitracin | Prevents cell wall synthesis | Gram +ve cocci Few Gram -ve | Topical combination | Nephrotoxic |
| Vancomycin | Inhibit cell wall synthesis | Gram +ve only | Drug of choice in pseudomembranous colitis (superinfection by antibiotics MRSA) | ototoxicity &Red neck syndrome: Chills, Fever, Maculopapular rash (head and upper thorax) due to histamine release. |
| POLYMYXINS | Facultative Gram -ve (P. aeruginosa and Coliform) | Combination to reduce catheter associated infection. Topical combination | Nephrotoxic Neurotoxic Neuromuscular blockade | |
| Sodium fusidate (Fucidin) | Inhibits 50s Ribosomal subunit | Gram +ve Gram -ve diplococci | Acne |
Treatments includes UTI’s
1- Antibiotics
In addition to CO-TRIMOXAZOLE and the Quinolones previously mentioned, UTIs may be treated with Penicillins as they are often listed as alternative regimens for urinary tract infections (UTIs) in pregnant women because they are pregnancy category B and eliminated renally.
However, resistance in Escherichia coli to them is very high, and susceptibility testing should be performed.
Amoxicillin/clavulanate acid is used for UTIs when resistance to other drugs is seen.
2-Urinary antiseptics
urinary tract antiseptic, including: (Methenamine, Nitrofurantoin, and nalidixic acid ) These drugs do not achieve antibacterial levels in the circulation, but because they are concentrated in the urine, microorganisms at that site can be effectively eradicated.
1. Methenamine
2. Nitrofurantoin
Beta-lactams inhibitors
All beta-lactams have a few things in common
-
All beta-lactams can cause hypersensitivity reactions, ranging from mild rashes to drug fever to acute interstitial nephritis (AIN) to anaphylaxis. There is cross-reactivity between some agents (e.g., peniciilin and cephalosporin), but it is difficult to predict exactly how often that will occur.
It seems that similarities between side chains of beta-lactams are responsible for cross-reactivity.
-
Seizures can result from very high doses of any beta-lactam, & some cause other neurologic effects. Accumulation to toxic levels can occur when the dose of a beta-lactam is not properly adjusted for a patient’s renal function
Did you check your patient’s renal function? In that case change dosage strength -
All beta-lactams share a mechanism of : Cidal
- They form complexes with (Irreversibly inhibit ) enzymes - trans- and carboxypeptidases (PCP), (i.e., penicillin binding proteins) in bacterial cell walls), which control synthesis of peptidoglycan – component of cell-wall of microorganisms (final steps of cell wall synthesis)=formation of peptide bridges between adjacent stands of peptidoglycan i.e prevents cross linking of the glycan strands leading to leading to swelling and lysis, killing the organism.
- Involves activation of autolytic enzymes in the cell wall, and results in lysis of organism.
-
All beta-lactams can be destroyed by beta-lactamases, enzymes produced by bacteria to destroy beta-lactams. Some beta-lactams such as penicillins are easily destroyed, whereas others such as carbapenems are stable against most beta-lactamases. But nature has shown us that whenever a beta-lactam is developed, a beta-lactamase capable of hydrolyzing it inevitably emerges.
-
B-Lactamase can be overcomed by :
- Give a B-Lactamase inhibitor at same time Clavulanic Acid & Sulbactam….etc EX: Augmentin
- Modify the antibiotic structure to make it more resistant EX: Amoxicillin
-
-
All beta-lactams lack activity against atypical organisms such as
Mycoplasma pneumoniae and Chlamydia pneumoniae which lacks cell wall. so Add another drug to your regimen if you are concerned about these organisms, as in cases of community-acquired pneumonia (CAP). -
All but one of the currently available beta-lactams lack activity against methicillin-resistant Staphylococcus (MRSA). So, Add vancomycin or another agent if this bacterium is suspected.
Beta lactams
Penicillins
| Drug - Benzyl’s | |
|---|---|
| Spectrum | +ve & -ve |
| Cons | Injections/narrow spectrum |
| Drugs | A.Injectable preparations: Short-acting preparation e.g. benzyl penicillin (penicillin-G): (6 hours) Its distribution is all over the body except CSF But it diffuses to CSF if meninges are inflamed (meningitis). Can be destroyed by B lactamase. B. Long-acting preparations: To overcome the drawback of the short duration of action of benzyl penicillin, which necessitates its frequent parenteral administration, long acting preparations of benzyl penicillin were prepared. These preparations are given only intramuscularly and never intravenously. The long acting penicillins include 1. Procaine penicillin-G: 12-24 hours - This is a combination of procaine & benzyl penicillin. It consists of 100.000 units of procaine penicillin + 100.000 units of benzyl penicillin. 2. Fortified procaine penicillin: 24 hours - It consists of 300.000 units of procaine penicillin + 100.000 units of benzyl penicillin-Given once daily IM. 3. Benzathine penicillin: This preparation produces low blood levels lasting from few days to 4 weeks depending on the dose. It should not be used in acute infections because the blood levels are low. So it is used in chemoprophylaxis of rheumatic fever. C. Oral preparations: These penicillins are stable in acid medium and hence escape destruction in the gastric juice. They include: Phenoxymethyl penicillin (penicillin V) & - Phenethicillin |
| Other therapeutic uses | MAINLY PROPHYLAXIS ARF - Gonorrheal Opthalmia - Subacture bacterial infective endocarditis due tocongenital vascular immunocompromized operative procedures |
| Drug - Anti-staph resistant | Desc |
|---|---|
| Drugs - Methoxonaf | Methicillin - Cloxacillin - Dicoloxicillin - Flucloxacillin - Naficillin |
| Spectrum | Staph spp only - narrow spectrum |
| Indications | B-lactamase producing staph. Beta-lactams kill staphylococci more quickly than vancomycin, so patients with MRSA infections who lack serious beta-lactam allergies should be switched to beta-lactams, such as antistaphylococcal penicillins or first-generation cephalosporins. This has been shown to be an important difference in serious infections. |
Amino penicillins
Comparison between Ampicillin and Amoxicillin:
| - Ampicillin | - Amoxicillin | |
|---|---|---|
| - Absorption | - ✓ | - ✓✓ |
| - Distribution | - ✓ | - ✓✓ |
| - Diarrhea side effects | - +++ | - + |
| - Spectrum | - Shigella, H.Infeluenza | - Salmonella, Strept.Facialis |
| Prodrugs for beta lactemeases / superinfections | Piva Tala Paca | Cluvanic Acid |
| Though the antistaphylococcal penicillins improve on the gram-positive coverage of natural penicillins, they do not add to their gram-negative coverage. Aminopenicillins are more water soluble and pass through porin channels in the cell wall of some gram-negative organisms. |
However, they are susceptible to beta-lactamases, and resistance to them is common. Aminopenicillins are rarely active against staphylococci, because these almost always produce penicillinases. These drugs also do not have useful activity against Pseudomonas aeruginosa.
- Their spectrum like penicillin G plus gram negative bacteria e.g. H. influenza, Salmonella, Proteus, and Shigella. They are B-lactamase susceptible
- They can be given orally (acid resistant) and by injection (IM and IV). They include
| Drug - Anti-pseudomonas | Desc |
|---|---|
| Drugs | Carbencillin, Ticarcillin, Azlocillin, Mezlocillin, and Piperacillin |
| Uses | They are broad-spectrum, but should only be used for pseudomonas, ampicillin resistant proteus, and anerobes. (eg. Bacteroids fragilis causing intrabdominal sepsis) |
| Cons | Beta Lactamase susceptible (can be combined with clavulanic acid) |
| Pros | Have an amazing synergetic effect when combined with Aminoglycosides |
Amidino-Penicillens Mecillinam, Pivmecillinam.
- they cross meniniges only in menigitis - none tetragenic
- Excretion mainly in renals - tubular systems
| Category | Details |
|---|---|
| Therapeutic Uses | A. Treatment of Infection: 1. Streptococcal infections 2. Staphylococcal infections of skin, mucous membrane, and bone 3. Pneumococcal infections 4. Syphilis and gonorrhoea 5. Meningococcal infections 6. Typhoid and paratyphoid fevers 7. Pseudomonas infection 8. Actinomycosis, Anthrax, H. influenza infections 9. Diphtheria, tetanus, gas gangrene 10. Peptic ulcer |
| Prophylaxis | 1. To prevent recurrence of Rheumatic Fever 2. To prevent gonorrhoeal ophthalmia in neonates 3. To prevent subacute bacterial endocarditis in specific cases from operative procedures such as dental extraction, tonsillectomy…etc. in patients with congenital or acquired valvular disease or immunocompromised patient. ((one dosage, 6 pieces for safe definite treatment)) |
| Adverse Effects | A. Hypersensitivity; epinephrine corticosterooids antihistamines B. Neurotoxicity C. Glossitis, stomatitis, and superinfection D. Cation toxicity E. Procaine penicillin effects F. Herxheimer reaction; late syphilis G. Masking of infection; syphilis, gonorrhea H. Other Adverse effects (carbenicillin, ticarcillin) |
| Types: | |
| 1-Early (Type I reaction-anaphylactic): | |
| Immediate - within 20 minutes |
-
apprehension, pruritis**, numbness**, choking,, edema, severe fall in blood pressure occurs, with bronchoconstriction, angioedema (including larynx) and sometimes death due to loss of fluid from the intravascular compartment. , loss of consciousness, death
-
Anaphylactic shock usually occurs suddenly, in less than an hour after the drug has been given orally, but within minutes if it has been given IV.
2-Accelerated - 1-72 hrs after administration: mainly hives
3**-Delayed _(Type III reaction, serum sickness):**_ it occurs after 2-12 days in the form of fever, malaise, arthralgia, skin rash and angioedema.
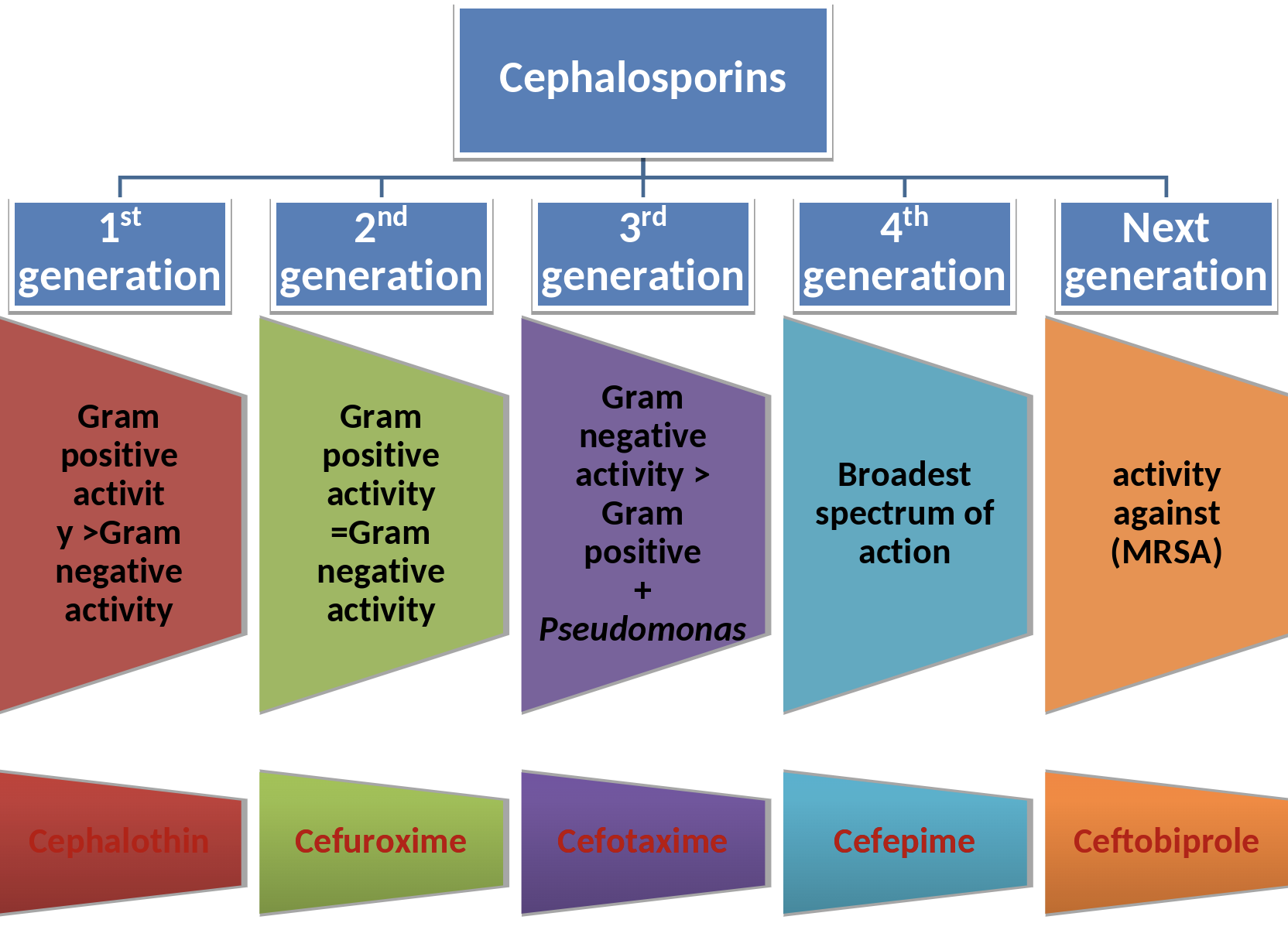
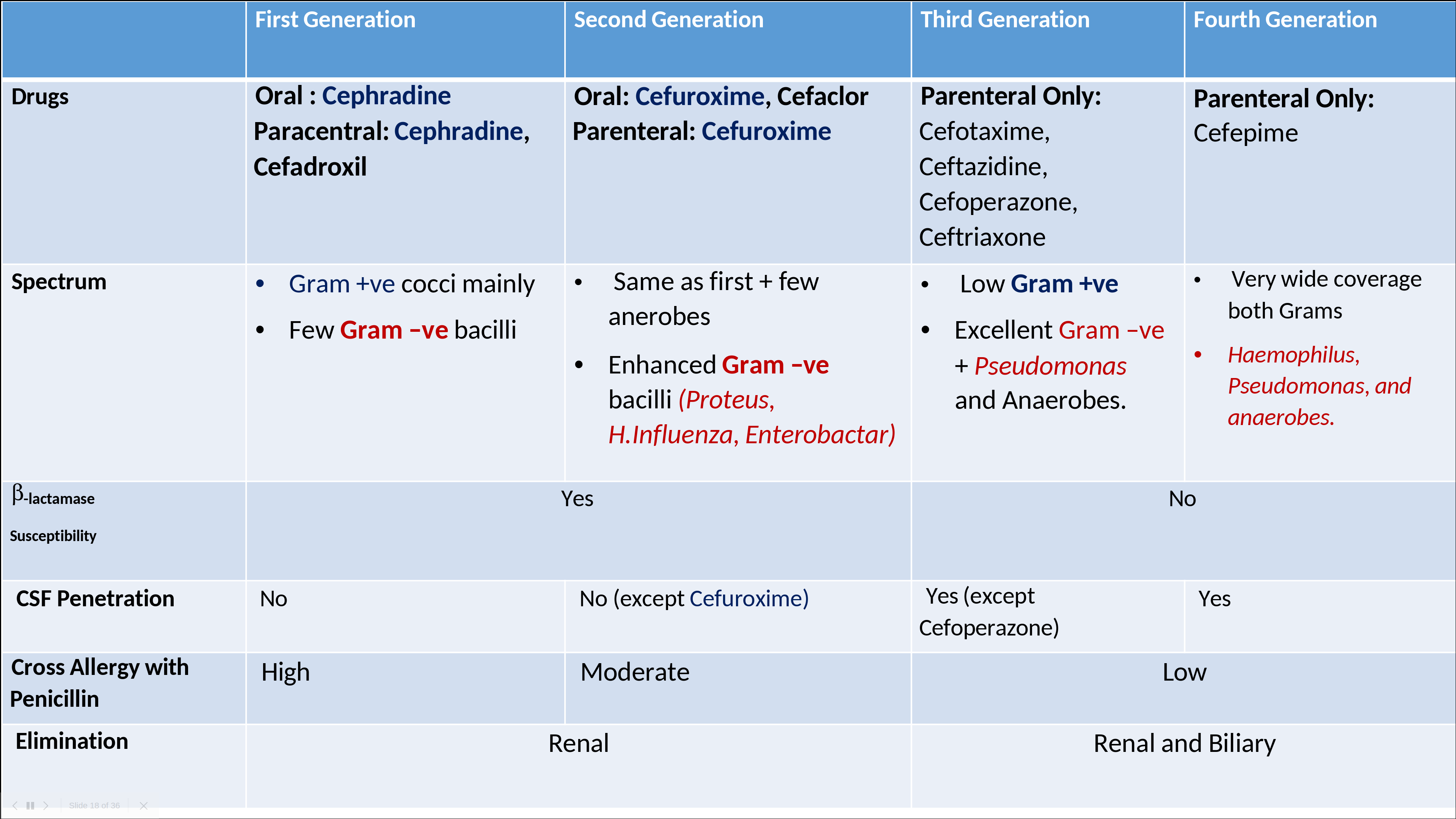
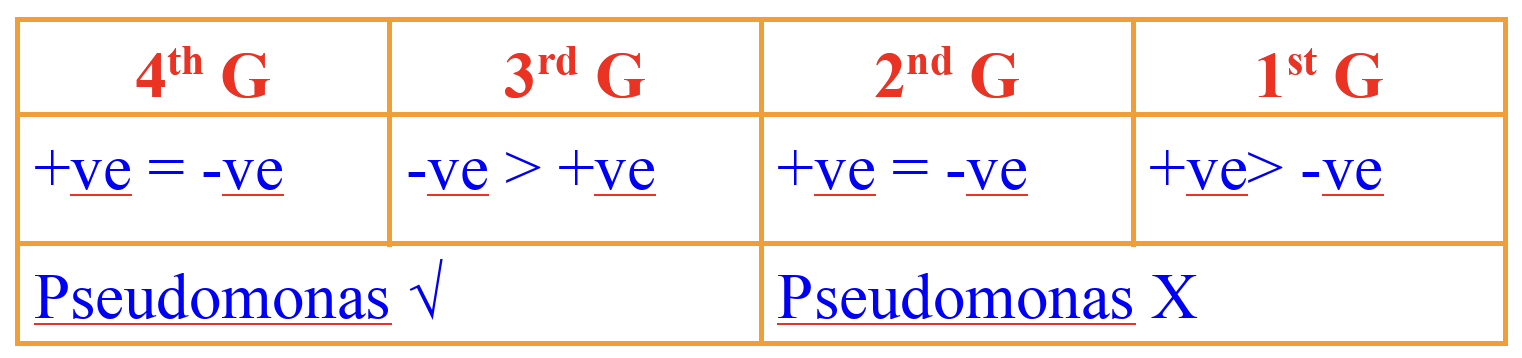
Cephalosporins
Certainly! To create a table based on the provided pharmacokinetics and antibacterial spectrum information, I’ll divide it into two main sections: Pharmacokinetics and Antibacterial Spectrum, with relevant subcategories. Here’s how the table would be structured:
| Category | Subcategory | Details |
|---|---|---|
| Pharmacokinetics | Absorption | Oral administration is better when separated from food. |
| BBB | Only new drugs (3rd generation and beyond) penetrate the blood-brain barrier. | |
| Excretion | Mainly renal for 1st and 2nd generation; biliary for 3rd and 4th generation. | |
| Antibacterial Spectrum | Generations | 1st Generation: Similar to penicillin. 2nd Generation: Expanded spectrum. 3rd Generation: Reversed spectrum of 1st + effective against Pseudomonas. 4th Generation: Effective against anaerobic bacteria. |
| Gram-positive vs. Gram-negative | Activity against gram-positive bacteria decreases from first to third generation, while activity against gram-negative organisms increases. |
| Letter | Therapeutic Use | Details |
|---|---|---|
| M | Bacterial Meningitis | 3rd Generation (Cefotaxime and Ceftriaxone) |
| O | Osteomyelitis | |
| S | Skin Infections | |
| T | Typhoid (Biliary Infection) | 3rd Generation (Cefoprazone or Ceftriaxone) |
| U | UTI (E.Coli) | 3rd/4th Generation |
| R | RTI | Respiratory Tract Infections |
| G | Gonorrhea | Penicillin Resistant, treated with IM (Intramuscular) Ceftriaxone |
| E | ENT Infections | Ear, Nose, and Throat Infections |
| N | Intestinal Infections | |
| T | Topical + Pseudomonal Infections | Used topically; also effective against Pseudomonas infections |
Side effects
(All Nephrotoxins Dislike Prothrombin)
-
ALL: 1st and 2nd do not use after failed or allergic penicillin treatment
-
Nephrotoxins: Nephrotoxic 1st & 2nd. Increased w/ diuretics or w/ nephrotoxic agents (Aminoglycosides).
-
Dislike: Disulfram like action •
-
Prothrombin: Some of the new drugs causes prothrombin/Platelet dysfunction (3rd) •
-
Superinfection (Most antibiotic causing polyps) • Treated with Metronidazole or Vancomycin
| Category | Description |
|---|---|
| Allergic Reactions | - Common reactions include rash, urticaria, fever, serum sickness, hemolytic anemia, and eosinophilia. - Cross-resistance with penicillin may occur. - Important to inquire about penicillin and cephalosporin hypersensitivity before administration. |
| Nephrotoxicity | - Nephrotoxicity is more pronounced with the 1st and 2nd generation cephalosporins. - Increased risk when used with diuretics or other nephrotoxic agents like aminoglycosides. - Less common with oral preparations. |
| Superinfections | - Caused by organisms like Pseudomonas, Klebsiella, Enterobacter, E. coli, Proteus, Serratia, and Candida. - Can lead to conditions like diarrhea. - Often treated with Metronidazole or Vancomycin. |
| Prothrombin/Platelet Dysfunction | - Notable in some new drugs (particularly 3rd generation cephalosporins). - Can lead to hypoprothrombinemia, thrombocytopenia, and/or platelet dysfunction. |
| Disulfiram-like Reaction | - Observed with certain agents like cefoperazone. - Occurs when given with alcohol, as these drugs block the second step in alcohol oxidation, leading to acetaldehyde accumulation. |
Generations cephalosoporins
Certainly! I’ll expand the table to include more detailed information for each generation of cephalosporins, focusing on their spectrum of activity, administration routes, examples, notable properties, and adverse effects.
| Generation | Spectrum & Properties | Parenteral Administration Examples | Oral Administration Examples | Notable Properties | Adverse Effects |
|---|---|---|---|---|---|
| First | Active against aerobic gram-positive cocci and some gram-negative bacilli. B-lactamase sensitive. Does not cross meninges. | Cephalothin, Cephradine | Cephalexin, Cephradine, Cefadroxil | Mainly used for skin and soft tissue infections, urinary tract infections, and respiratory tract infections. | Generally well-tolerated; allergic reactions similar to penicillins. |
| Second | Extended spectrum including anaerobes and gram-negative bacilli (Proteus, Enterobacter, H. influenza). Relatively resistant to B-lactamases. Doesn’t cross meninges. | Cefuroxime | Cefuroxime, Cefaclor | Effective against otitis media, sinusitis, respiratory tract infections, and some Lyme disease presentations. | Allergic reactions; gastrointestinal disturbances. |
| Third | Covers gram-negative organisms including Pseudomonas and anaerobic microorganisms. Diminished gram-positive activity. Highly resistant to B-lactamase & high cross to meninges. | Ceftriaxone, Cefotaxime, Ceftazidime, Cefoperazone, Cefixime | - | Broad-spectrum; used in severe infections like sepsis, pneumonia, meningitis, and gonorrhea. Ceftriaxone: used with typhoid; problematic in neonates. Cefotaxime: renal adjustment needed. | Gastrointestinal issues; hypersensitivity reactions. Ceftriaxone associated with biliary sludging and potential neonatal complications. |
| Fourth | More resistant to B-lactamases. Highly active against Haemophilus, Pseudomonas, and anaerobes. Broad spectrum. | Cefepime | - | Used for severe hospital-acquired infections, including febrile neutropenia, pneumonia, and complicated urinary tract infections. Comparable to a combination of first and third-generation drugs. | Neurotoxicity (e.g., non-convulsive status epilepticus), similar allergic reactions to other beta-lactams. |
| Fifth | Active against MRSA. Unique activity against penicillin-binding protein 2a of MRSA. | Ceftaroline | - | Utilized for serious MRSA infections as an alternative to vancomycin or daptomycin. Also effective against multi-drug resistant Streptococcus pneumoniae. | Possible higher incidence of neutropenia, allergic reactions. |
6th SIDEROPHORE CEPHALOSPORIN
Cefiderocol is a unique drug. It has the basic structure of a cephalosporin and works to prevent peptidoglycan cross-linking, as other beta-lactams do. But it has a side chain that complexes with iron and is recognized by bacteria as a siderophore, which bacteria actively uptake.
-
Bacteria need iron to grow. Siderophores are substances that many bacteria secrete into their environment to complex with free iron, then actively transport across their cell walls to the interior of the cell. When cefiderocol complexes with iron, bacteria recognize it as a siderophore and actively transport the complex into the cell, where it can work to prevent cell wall synthesis.
-
Cefiderocol’s siderophore side chain allows for active uptake into bacteria, avoiding some mechanisms of resistance, such as porin changes.
- Cefiderocol is an expensive antibiotic that has utility against many of the most resistant gram-negative organisms in practice, including those resistant to Carbapenems.
-
Cefiderocol used for treatment of complicated UTIs and hospital acquired pneumonia. However, it is used off-label for the treatment of many types of infections caused by resistant gram-negative infections.
-
Cefiderocol should be used only in patients with resistance to other antibiotics.
-
Of course, cefiderocol resistance occurs. Those bacteria never quit, so susceptibility testing still needs to be performed.
Other betalactams
| Drug | MOA | Uses | Side effects |
|---|---|---|---|
| Monobactams Aztreo_nam_ | monocyclic B-lactams Excellent Gram –ve; poor against Gram +ve & Anerobes | It has a low potential to produce hypersensitivity reactions inhalation to patients with cystic fibrosis - Pseudomonas, particularly in patients with a history of beta lactam allergy must be admitted | |
| Carbapenems imipenem/cilastatin, meropenem, ertapenem, Carbapenems | broadest-spectrum antibacterial drugs against most aerobic and anaerobic bacteria (Gram-positive and gram-negative) with the exception of occasional Pseudomonas strains. | Resistant to B lactamases OM of G-ve bacteria to access the PBPs metabolized in the kidney to a nephrotoxic product. Cilastatin | but imipenem has a higher propensity to induce seizures Allergy, Neurotoxicity |
Imipenem if given alone - combine w/ Cilastatin
is inactivated by renal dihydropeptidase so it’s combined with cilastatin which inhibits renal dihydropeptidase
CARBAPENEM / BETA-LACTAMASE INHIBITOR COMBINATIONS :
1-meropenem/vaborbactam
2- imipenem/cilastatin/relebactam
Meropenem: + vabrobactam
The other drug of this group which is currently available. It does not undergo metabolism by renal dihydropeptidase enzyme.
Adverse effects
- Allergy: Carbapenems may rarely elicit an allergic reaction in patients with a history of penicillin allergy.
- Blood disorders.
- Neurotoxic in high doses .
- G.I.T: nausea, vomiting, etc.
Anti-Tuberculosis Treatments
| Drug | MOA | Uses | Side effects |
|---|---|---|---|
| INH Isoniazid | acetylation - inhibition of mycolic acid - desaturase enzyme NAD form false NAD | Chemophoralyxis Postiive tuberculin in HIV + Close contact | Neurotoxicity managed by Vit.b6 / Hepatocellular SLE G6PD |
| Pyrazinamide | prevent the production of mycolic acids by inhibiting the enzyme fatty acid synthetase I Needs to be converted to prodrug - (Pyrazinioic acid) | Combination therapy with isoniazid & rifampin when initial intensive course resitance is suspected | Hepatotoxic DARK URINE Hyperuricemia & Artheralgia |
| Ethambutol | inhibits the enzyme arabinosyl transferase III | enhancing the activity of lipophilic drugs such as Rifampin & [ofloxacin] - may combine with isoniazid or alone during pregnancy | Optic neuropathy RED/GREEN Hyperuricemia/ Gout |
| Rifampin | CIDAL inhibiting RNA polymerase, preventing transcription by blocking the production of messenger RNA. Phase 4 INHIBITION OF ASSEMBLY OR RELEASE OF VIRAL PARTICLES | FIRST LINE Leprosy & Tuberculosis Prophylaxis against H. Influenza Meningitides - broad activity against resistant staphylcocci Chlamydia poxvirus | RED Urine/Tears Enzyme inducer Hepatotoxic |
| Dapson | STATIC related sulphonamides with action of folate synthesis inhibition | Leprosy & Pneumocystis Carinni in AIDS | Hemolysis rbcs & Lepra reaction - suppressed by corticosteroids |
| Clofazimine | bind to mycobacterial DNA and inhibit mycobacterial replication and growth | Delayed anti-leprotic effect can reach 2 months - has anti-inflammatory activity | RED BLUE BLACK skin & URINE |
| Streptomycin | Milliary & Renal TB’s | Ototoxicity | |
| Capreomycin | peptide antibiotic given by intramuscular injection. There is some cross-reaction with the aminoglycoside kanamycin. | nephrotoxic & ototoxic (tinnitus, deafness & vestibular disturbances ). | |
| Ethinamide | congener of INH. • Blocks synthesis of mycolic acid. | Hepatitis + Gynecomastia + Impotence | |
| PAS paraaaminos | compared with streptomycin and INH is less effective and more toxic. | Active only against TB bacilli. | Hepatotoxicity GIT upset Hypothyroidism |
REGIMEN OF THERAPY OF TB
The treatment has two phases of combination therapy: A) An initial intensive course for at least two months to reduce the number of bacilli as rapid as possible and avoid emergence of resistant strains. At least three drugs are used (INH; ISONIAZID + Rifampin + Pyrazinamide ), a fourth drug may be added if resistance is possible. The fourth drug may be Ethambutol or Streptomycin.
B) Continuation phase during which the number of bacilli is further reduced. ISONIAZID and Rifampin are used at least for 4 months. Ethambutol may be added if resistance is suspected.
- The previous regimen is used in uncomplicated pulmonary TB.
- Generally treatment depends on the type of the organism , site of lesion & severity of the disease.
- The course varies from 6-18 months.
- Long course is needed in cases of TB meningitis , bone , joint , kidney & some forms of lymph-adenopathy
TB and pregnancy:
The best therapeutic regimen is ISONIAZID and EthambutolZ . Rifampin is used only if TB is disseminated or very extensive. Streptomycin should not be used
Anti-Fungal
Drugs for subcutaneous and systemic mycotic infections including Opportunistic mycoses:
| Drugs | MOA | Uses | Side Effects |
|---|---|---|---|
| Amphotericin B (Ambisome) | I.V. insoluble - Binds ergosterol - Forms pore channels | used in severe systemics | Fever Chills Renal impairment - for fever corticosteroids |
| Flucytosine | allowing more 5-FC to penetrate the cell and leading to synergistic effects | Combined w/ A-B systemic mycoses and for meningitis caused by: Cryptococcus neoformans , Candida albicans.* | Marrow supression - gut microfloa hepatotoxic |
| Echinocandins caspofungin, micafungin, anidulafungin | inhibit beta-1,3-D-glucan synthase | invasive candidiasis | invision reaction Hepatotoxicity |
Opportunistic mycoses
Group of mycoses caused by saprophytic fungi in immuno- compromised individuals
Examples of immunocompromised people
- HIV infected patients.
- Pregnant women.
- Transplant persons.
- Patients receiving chemotherapy or radiotherapy.
- Certain cancers and genetic disorders.
Anti-Fungal Azoles
The azoles Inhibit the fungal cytochrome P450 3A enzyme, which is responsible for converting lanosterol to ergosterol, the main sterol in the fungal cell membrane which disrupts membrane structure and function, which, in turn, inhibits fungal cell growth. All azoles inhibit the hepatic CYP450 3A4 isoenzyme to varying degrees.
Contraindications of Azoles
Azoles are considered teratogenic, and they should be avoided in pregnancy unless the potential benefit outweighs the risk to the fetus.
| Drugs Tri - Imi | MOA | Uses | Side effects |
|---|---|---|---|
| FLUCONAZOLE | orally or intravenously | Candida and cryptococcal disease | cytochrome P450 QT interval (QTc) |
| ITRACONAZOLE | wider spectrum of activity than ketoconazole and fewer adverse effects. | with a broader spectrum than fluconazole but narrower than voriconazole, posaconazole, and isavuconazole | cytochrome P450 QT interval (QTc) negative intrope heart |
| VORICONAZOLE | broad-spectrum antifungal like itraconazole, | Candida species and many molds | seeing wavy lines or halos around bright lights sun sensitivity**, Central nervous system effects - renal dysfunction cytochrome P450 hepatotoxic |
| Posaconazole | broad spectrum azole anti-fungal analog of itraconazole | pseudohyper-aldosteronism; not in hypertension. | |
| ISAVUCONAZOLE | many ways isavuconazole is similar to posaconazole. | expanded spectrum of activity that includes Candida, Aspergillus, and Mucorales. |
Drugs for cutaneous mycotic infectionsZ
| Drugs | MOA | Uses | Side effects |
|---|---|---|---|
| Squalene epoxidase inhibitors Terbinafine, naftifine, butenafine | blocking the biosynthesis of ergosterol | Oral terbinafine fungal infections of nails also known as dermatophyte onychomycoses and tinea capitis . Topical terbinafine tinea pedis , tinea corporis , and tinea cruris | - not given to pregnancy or lactation |
| Griseofulvin | deposited in keratin precursor - interacts with the microtubules within the fungus to disrupt the mitotic spindle and inhibit mitosis. | oral Long course -dermatophytosis of the scalp and hair. | hepatic CYP450 anticoagulants pregnancy & Porphyria |
| Nystatin ORAL & TOPICAL | polyene negligibly absorbed from the gastrointestinal tract, and it is not used parenterally due to systemic toxicity (nephrotoxicity). | oropharyngeal candidiasis (thrush), vulvovaginal candidiasis cutaneous candidiasis | Topical and vaginal forms may cause skin irritation |
| Drugs Imi | MOA | Uses | Side effects |
| Clotrimazole | Topical | dermatophyte infections and treatment of vaginal candidiasis. | |
| Ketoconazole | Systemic and mucocutaneous infections Prevention of Candida infection in immune suppressed patients | Gynecomastia & hepatics | |
| Miconazole | given orally for oral and other infections of the gastrointestinal tract. |
Naftifine and Butenafine
Naftifine is Broad spectrum, fungicidal active against Trichophyton, Microsporum, and Epidermophyton.
Naftifine 1% cream and gel are used for topical treatment of tinea corporis, tinea cruris, and tinea pedis. Duration of treatment is usually 2 weeks.
Butenafine like naftifine, is used for topical treatment of tinea infections.
Anti-helmintic
| Drugs for Nematodes | MOA | Uses | Side effects |
|---|---|---|---|
| Albendazole Mebendazole, Thiabendazole | Blocks glucose uptake | roundworm, pinworm, hookworm infection, threadworm, filariasis 1. hydatid disease & cysticercosis - dog & pork worms; cestodes | |
| Diethylcarbamazine (systemic) tissue | tissue nematodes - ilarial infection of the eye (loa loa) & elephantiasis | Reaction to dying filaria includes: fever, rash, ocular damage, joint pain and lymphangitis - Mazzotti reactions; occular damage / fever | |
| Ivermectin | GABA mediated neurotransmission in nematodes causing immobilization | onchocercosis, and threadworm infection | Mazzotti reactions; occular damage |
| Drugs for Cestodes | MOA | Uses | Side effects |
| Niclosamide | activating ATPases; = energy depletion & lysis | 1 of 2 drugs of choice ( with praziquantel) in ttt of fish,pork,and beef tapeworms infection | Mild GIT upset, rash headache |
| Drugs for Trematodes | MOA | Uses | Side effects |
| Praziquantel | calcium paralysis leading to vacuolization and death of the parasite. | all trematodes & cestodes infection | intracranial hypertension and convulsion if used in ttt of neurocysticercosis |
| Bithionol | Drug of choice in ttt of fascioliasis ( sheep liver fluke) | 1. common: N/V ,headache, phototoxcity 2. less common: protenuria,leucopenia |
leishmaniasis
- Sodium stibogluconate
Alternate drugs:
-
Fluconazole; Azole; Anti-Fungal or metronidazole; anti-ameobic for cutaneous lesions
-
Amphotericin B; Anti-Fungal for mucocutaneous lesions
-
Pentamidine for visceral leishmaniasis
Intestinal nematodes includes:
-
enterobius vermicularis (pinworm)
-
ascaris lumbricoides (roundworm)
-
ancyclostoma & necator species (hookworm)
-
strongyloides stercoralis (threadworm)
Tissue nematodes:
-
filariasis; Diethylcarbamazine
-
The 4 important cestodes are:
-
taenia saginata ( beef tapeworm) Niclosamide
-
taenia solium (pork tapeworm; causes cysticerci in brain & eye) Albendazole
-
diphyllobothrium latum ( fish tapeworm) Niclosamide
-
echinococcus granulosus (dog tapeworm that cause hydatid cysts in lung,liver,and brain) Albendazole
Medically important trematodes are:
- schistosoma species (blood fluke)
- clonorchis sinesis (liver flukes in southeast Asia)
- paragonimus westermani ( lung fluke in Asia,India)
Anti-Ameobic & Anti-Malarial
| Drugs for Tissue Ambeocidial | MOA | Uses | Side effects |
|---|---|---|---|
| Metronidazole | Ferrodoxine Oxidoreductase enzyme ⇒ DNA BREAKS | Tissue Ameobicidal; Giardiasis; Trichomaniasis; B. Fragilis Decubitus lesion | DARK RED URINE DISULFIRAM Tetra |
| Emetine & Dihydroemetine | requires hospital admission - inhibit protein synthesis by preventing translocation | intestinal or hepatic amoebiasis | Cardiotoxic: hypotension and ECG changes - |
| Luminal amebicidal | MOA | Uses | Side effects |
| Diloxinade Furpate etofamide | ***can be given with Metronidazole for eradication of the amoeba *** | eradicate amoebae present in intestinal lumen | contraindicated in pregnancy and in children below 2years of age - generally safe therapeutic index |
| Iodoquinol clioquinol | Thyroid enlargement due to high iodine content of the drug | ||
| Paromomycin & Tetracyclines | |||
| Anti-Malarial & Ambeocidil | MOA | Uses | Side effects |
| Chloroquine HYDROXY-CHLOROQUINE:rheumatoid artharitis. AMODIAQUINE: Can cause agranulocytosis. - Recommended for chloroquine resistant malaria. | concentration in RBCs, liver | hepatic amoebiasis Prevention of amoebic liver abscess - Following Metronidazole for ttt of amoebic hepatitis amoebic liver abscess in case of failure or contraindication to flagyl Rhemautoid arthritis SLE P. Vivax ovale Malairi non resistance - take before flight one dose weekly | Cardiac depression, vasodilation & Hypotension. *Give slow IV infusion & monitor cardiac functions. * Cautions/ Contraindications: Visual defects, epilepsy, heart failure. |
| Anti-Malarial Resistance | MOA | Uses | Side effects |
| Quinine | acute severe chloroquine resistant P.falciparum | Cinnchonism Black water fever due to excessive haemolysis/ renal failure | |
| Mefloquine | acute attack of chloroquine resistant P.falciparum especially mild and moderate cases | psychosis - vertigo - visual | |
| antirelapse therapy Prevention of transmission | MOA | Uses | Side effects |
| Primaquine | - It has no effect on erythrocytic stage (not used in acute attack) n | prevention of relapse in P.vivax and ovale Prevent transmission of infection from human to mosquito by killing the gametocytes | Haemolysis in G6PD deficiency ; test for G6PD & - methaemo-globinemia manifested by cyanosis |
| ** |
Fansidar = *sulphadoxine + [pyremethamine](Folate%20Antagonists.md)*
Fansimaf = *sulphadoxine + [pyremethamine](Folate%20Antagonists.md) + mefloquine*
Common symptoms
Recurrent fever and chills, splenomegaly
II) chemoprophylaxis:
-
clinical prophylaxis: Chloroquine, proguanil, & fansidar = sulphadoxine + pyremethamine suppress the clinical manifestation of malaria by killing parasite as soon as they reach the RBCs .
-
antirelapse therapy: Primaquine in P.vivax and ovale only by killing the dormant stage in liver;
-
prevent transmission: Primaquine + folate antagonists; progunail ,pyremethamine by killing the gametocytes:
H. Pylori medications **Clarithromycins, Ampicillin & Amoxicillin, Tetracyclines & Metrondiazole
Other Anti-Virals
| Class of Anti-Viral Agents | Agents |
|---|---|
| Anti-Influenza Agents | - Amantadine (Inhibition of Viral Uncoating) - Rimantadine - Zanamivir - Oseltamivir |
| Antiherpes Agents | - Acyclovir (Prototype, Inhibition of Synthesis of Viral Components, Phase 3) - Valacyclovir - Famciclovir - Penciclovir - Trifluridine - Vidarabine |
| Anti-Cytomegalovirus Agents | - Gancyclovir (Same effects as Acyclovir) - Valgancyclovir - Cidofovir - Foscarnet - Fomivirsen |
| Anti-Hepatitis Agents | - Lamivudine (Nucleoside Reverse Transcriptase Inhibitor, NRTI) - Adefovir (Nucleotide Inhibitor) - Interferon Alfa - Pegylated Interferon Alfa - Ribavirin (Same as Acyclovir, Inhibition of Synthesis of Viral Components, Phase 3) |
Anti HIV
Replication of HIV
- Virion binding - CD4, chemokines
- Reverse transcriptase- RNA to DNA
- Integration of viral DNA
- Replication of viral RNA
- Protease
- Assembly of virions
- Release
| Type | Drugs… |
|---|---|
| 1. attachment - Fusion Inhibitors interfere with receptors | - Enfuvirtide - Maraviroc |
| 2. Nucleoside analogue reverse transcriptase inhibitors PH3 | - ZIDOVUDINE first drug created for HIV - Lamivudine; used also for hepatitis - Emcitrabine - Entecavir |
| 3. Integrase inhibitors: | - Raltegravir |
| 4. Protease Inhibitors | - Indinavir - Ritonavir - Saquinavir |
| Non-nucleoside; Direct reverse transcriptase inhibitors | - Nevirapine - Efavirenz |
| Nucleotide | - Tenofovir |
Why Does Treatment Fail?
- NON-ADHERENCE
- Intolerance
- Infection with a resistant virus
steps of antiviral drug on replication process
| hase | Description | Anti-Viral Agents |
|---|---|---|
| Phase 1 | INHIBITION OF ATTACHMENT TO OR PENETRATION OF HOST CELL: Attachment and Penetration: Viruses attach and bind to the host cell membrane. Specific receptor sites on the host cell are recognized by corresponding areas on the virus. The receptor-virus complex penetrates the cell. | Gamma Globulins (Immuno Globulins), Enfuvirtide, Maraviroc |
| Phase 2 | INHIBITION OF VIRAL UNCOATING: Uncoating: The protein coat of the virus is dissolved, liberating free DNA or RNA, i.e., the viral genome. | Amantadine (also included in Phase 1) |
| Phase 3 | INHIBITION OF SYNTHESIS OF VIRAL COMPONENTS (Non-structural protein, DNA and RNA) Synthesis of Viral Components: The virus’s genome is duplicated and viral proteins are synthesized. Host synthesis of nucleic acid and/or protein is inhibited as host cell processes are directed towards synthesis of viral components. | Ribavirin, Acyclovir, Ganciclovir, Idoxuridine, Vidarabine, Zidovudine, Interferons |
| Phase 4 | INHIBITION OF ASSEMBLY OR RELEASE OF VIRAL PARTICLES: Assembly and Release of Viral Particles: The viral genome is encapsulated by viral protein. The mature virus is then released from the cell. | Rifampin (anti-TB drug) |
Anti cancers
| Drug | MOA | Uses | Side effect |
|---|---|---|---|
| Alkylating agents nitrogen mustard; cyclophosphamide. | bind irreversibly to macromolecules in the cell as DNA, RNA and proteins. - alkylation process The nitrogen mustards were observed to inhibit cell growth, especially of bone marrow. Shortly after the war, these compounds were investigated and shown to inhibit the growth of cancer cells. | leukemia, lymphoma | haematuria, cystitis = urinary incontinence |
| Anti-metabolites: (Folic Acid Antagonist) - Methotrexate (MTX) | is actively transported into mammalian cells and inhibits dihydrofolate reductase, the enzyme that normally converts dietary folate to the tetrahydrofolate form required for thymidine and purine synthesis. | marrow suppression, megaloblastic anaemia. | |
| Anti-metabolites: mercaptopurine | inhibit ==DNA synthesis. | marrow suppression, megaloblastic anaemia. | |
| - Natural products Vincristine | mitosis inhibitors A wide range of drugs has been developed from plants, bacteria, yeasts and fungi. also Antibiotics: as actinomycin D. | peripheral neuropathy. | |
| tamoxifen | Estrogen antagonists are primarily used in the treatment of breast cance | estrogen receptor-positive tumors Tamoxifen is the drug of choice in postmenopausal women with or recovering from metastatic breast cancer. It is most effective in patients who have estrogen receptor-positive tumors. adjunvctive therapy to oophorectomy to leuprolide or goserelin in premenopausal women with estrogen receptor-positive tumors. *if positive estrogen 1st degree family as prophylaxis * | |
| cyproterone acetate | androgen antagonists | prostate cancer | |
| Glucocorticoids | Glucocorticoids have essential roles in the prevention of allergic reaction, vomiting control, relief of intracranial hypertension or spinal cord compression in neurologic complications, and pain relief. | They are integral components of curative therapy for acute lymphoblastic leukemia, non-Hodgkin’s lymphoma, and Hodgkin’s disease. | |
| Estrogens | Estrogens inhibit the effects of endogenous androgens and androgen-dependent metastatic prostatic carcinoma. | Cardiac and cerebrovascular complications and carcinoma of the male breast are potential adverse effects. | |
| Progenstins | endometrial carcinoma and back-up therapy for metastatic hormone-dependent breast cancer | ||
| Drug Manage | MOA | Uses | Side effect |
| Corticosteroids | (predinsolone) are among regiment particularly useful in treating lymphocytic leukemias and lymphomas. | ||
| Metoclopramide | (antiemetics) and the cannabinoid nabilone can be used to control nausea and vomiting. | ||
| Allopurinol | xanthine oxidase inhibitor | may be used to prevent gout. in hyperuricemia side effects of anti cancers - Very high levels of plasma uric acid with precipitation of clinical gout or renal failure may complicate treatment of leukaemias and Iymphomas. |
- OthersY: Several drugs have been identified, Mechanism of action is not fully established but are thought to interact with DNA synthesis or replication. They include , dacarbazine, and cis-platinum.
Biological therapy
These agents specifically target molecular anomalies in signal transduction pathways that exist in tumor cells.
As biological agents target pathways which are more critical to cancer cells than normal cells they are generally less toxic than chemotherapy and in some cases are more effective.
Example: monoclonal antibodies
other side effects
- Doxorubicin : cardiotoxic, alopecia.
- Bleomycin : pulmonary fibrosis.
- Cisplatinum: Renal damage.