IM
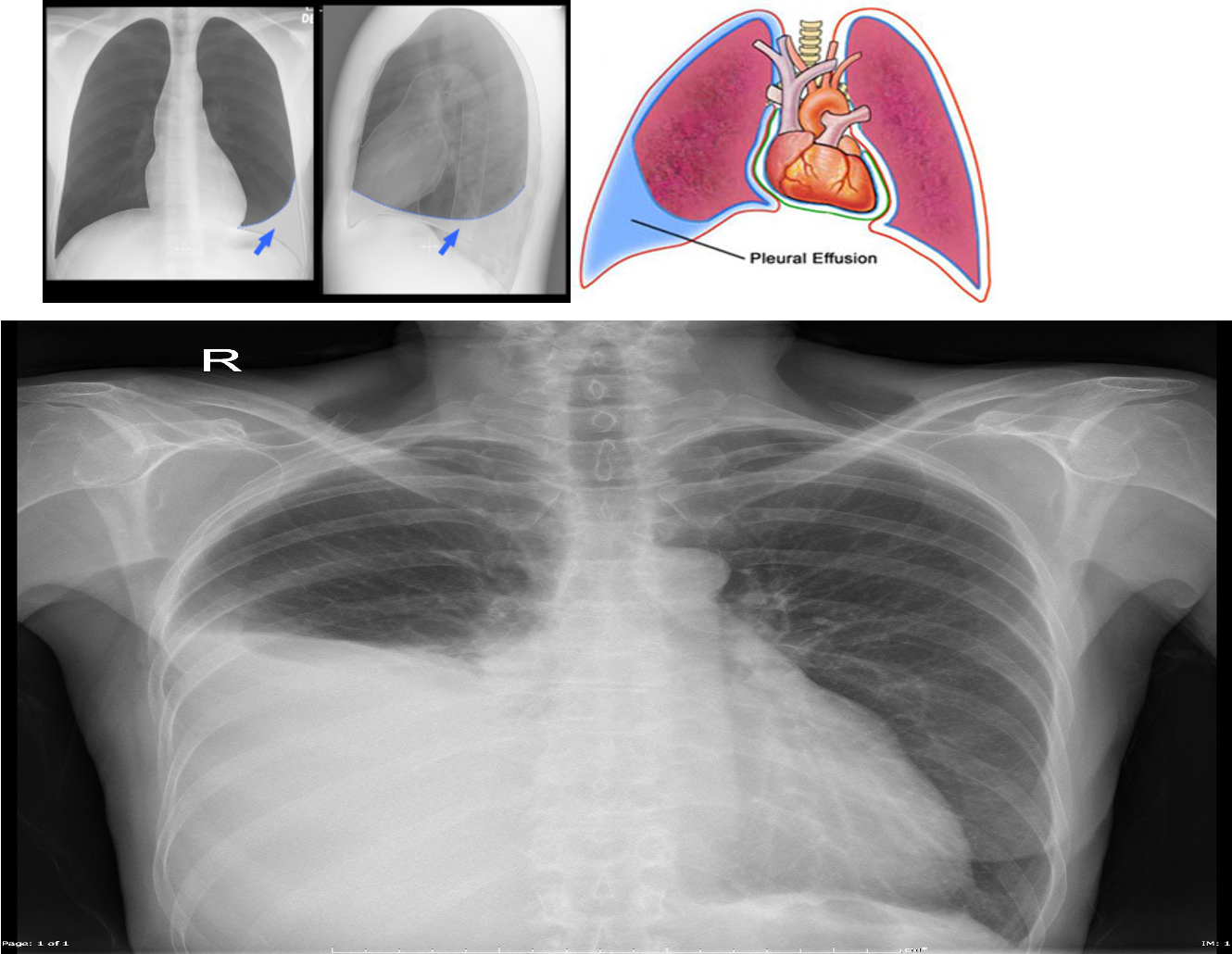
An imbalance between the oncotic and hydrostatic forces that govern pleural fluid formation and lymphatic drainage can result in excessive fluid accumulation.
Pleural Effusion: Clinical Features
- Asymptomatic: Small pleural effusion (< 300 mL).
- Characteristic symptoms:
- Dyspnea
- Pleuritic chest pain (sharp retrosternal pain)
- Dry, nonproductive cough.
- Symptoms of hypoxia
- Symptoms of the underlying disease:
- Fever in empyema
- Cachexia in cases of malignancy
- Symptoms of left-sided heart failure; back pressure
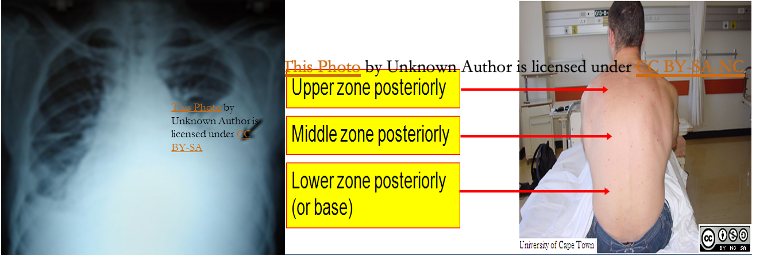
- Physical exam findings: Clinically detected if > 500 ml.
- Inspection and palpation (affected side):
- Asymmetric expansion (↓Chest movement)
- Mediastinal displacement (Trachea shifted away from the side of the lesion in massive effusion).
- Reduced tactile fremitus.
- Percussion: Stony dullness
- Auscultation:
- Faint or absent breath sounds over the area of effusion
- Vocal resonance - reduced or absent
- Inspection and palpation (affected side):
Pleural Effusion: Diagnostics
Imaging to confirm the diagnosis:
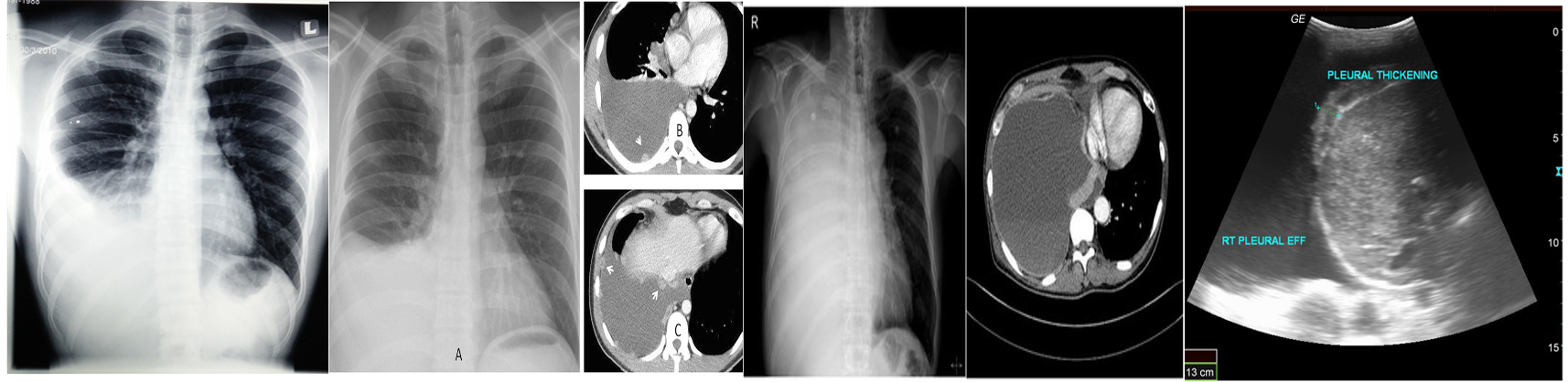
Chest X-ray: Lateral decubitus view (most sensitive): > 200 ml.
- Unilateral blunting of the costophrenic angle
- Homogeneous density with a meniscus-shaped margin (meniscus sign)
- Complete opacification of the lung (Large effusion) and Mediastinal shift and tracheal deviation.
Ultrasound: Quick, bedside assessment, if planning thoracentesis.
- Very sensitive: 20 ml. Hypoechoic collection.
- Detection of pleural thickening and pleural nodules.
CT: Gold standard for small effusions.
- Guiding placement of indwelling pleural catheters.
- Directed thoracentesis of a loculated effusion.
- Suspected parenchymal or pleural pathology. contrast CT is now increasingly performed to investigate the underlying cause, particularly for exudative effusions
Thoracentesis:
- 21G needle, 20 ml syringe under aseptic condition through intercostal space towards the top area of dullness.
- Contrast CT is now increasingly performed to investigate the underlying cause, particularly for exudative effusions.
Diagnostic Thoracentesis
For diagnostic and/or therapeutic purposes.
- Indications:
- New unilateral effusion
- Hx malignant tumor with effusion
- Pneumonia with parapneumonic effusion
- Heart failure with atypical findings (e.g., pleuritic chest pain, fever, unilateral effusion).
- Contraindications: Local infection, bleeding risk.
- Studies (5 Cs):
- Color
- Cytology
- Culture
- Cell count
- Chemistry
- TB testing: Adenosine deaminase, AFB smear microscopy
Transudate vs Exudate
Transudate: Fluid permeates into the pleural cavity through intact pulmonary vessels (e.g., in congestive heart failure).
Clear, extravascular fluid caused by:
- Increased capillary hydrostatic pressure (CHF)
- Decreased capillary oncotic pressure (hypoalbuminemia).
- Low in protein and cells.
Common causes
- Congestive heart failure
- Hepatic cirrhosis
- Nephrotic syndrome
- Protein-losing enteropathy
- Hypo-albuminemia
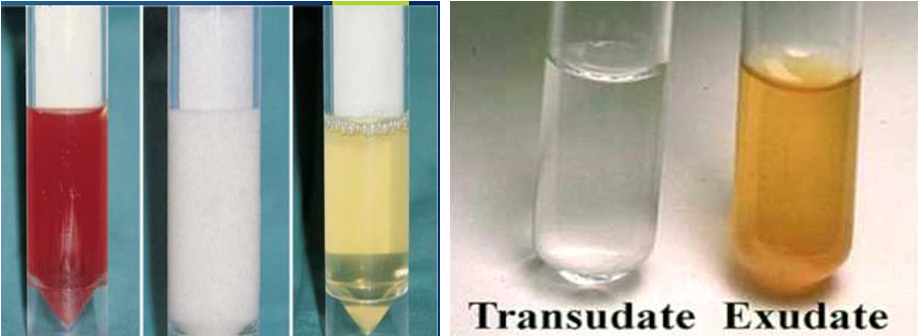
Exudate: *Fluid escapes into the pleural cavity through lesions in blood and lymph vessels (e.g., due to inflammation or tumors). Yellow/cloudy extravascular fluid caused by:
-
Increased capillary permeability (inflammation or malignancy).
-
High in protein and cells.
-
Common:
- Bacterial pneumonia (parapneumonic), empyema, TB
- Carcinoma of the bronchus, lymphoma
- Pulmonary infarction
-
Rare:
- Post-MI
- Acute pancreatitis (↑amylase)
- SLE, Rheumatoid arthritis (Connective tissue disorders)
- Mesothelioma (Asbestosis)
-
Very rare causes:
- Sarcoidosis
- Yellow nail syndrome (lymph oedema)
- Familial Mediterranean fever
- Parasitic illness (amebiasis, echinococcal disease)
- Trauma (high vascular permeability)
-
Differential Diagnosis of Exudative Effusions
| Pleural Fluid Parameter | Associated Conditions |
|---|---|
| WBC count > 10,000 cells/mm3 | Parapneumonic effusion, Pancreatitis, Pulmonary embolism |
| Neutrophils > 50% of total leukocytes | Acute infection, Pulmonary infarct |
| Lymphocytes > 50% of total leukocytes | Tuberculous infection, Malignant effusion, Chylothorax |
| RBC count > 5,000 cells/μL | Hemothorax, Malignant effusion, Pulmonary embolism/infarct |
| pH < 7.2 | Complicated parapneumonic effusion, Empyema, Malignant effusion, Esophageal perforation |
| Positive Gram stain or culture | Parapneumonic effusion, Empyema |
| Adenosine deaminase > 50 mcg/L | Tuberculous effusion |
| Positive AFB smear microscopy | Tuberculous effusion |
| Abnormal cytology | Malignant effusion |
| Amylase > 200 mcg/dL | Pancreatitis, Esophageal perforation, Ruptured ectopic pregnancy, Pleural infection |
All patients with a pleural effusion in association with sepsis or a pneumonic illness require diagnostic pleural fluid sampling.
- If the fluid is purulent or turbid/cloudy, a chest tube should be placed to allow drainage.
- If the fluid is clear but the pH is less than 7.2 in patients with suspected pleural infection, a chest tube should be placed.
Pleural Fluid Analysis: Light Criteria - Differentiating Transudates from Exudates
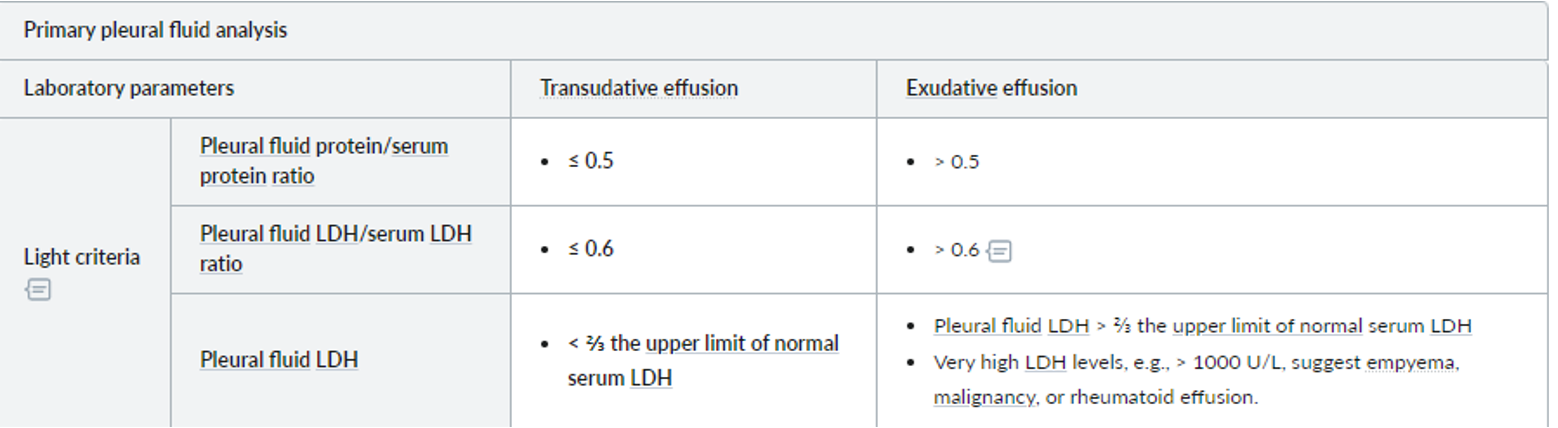
- MEAT has low glucose: Malignancy, Empyema, Arthritis (rheumatoid pleurisy), and Tuberculosis are causes of pulmonary effusion associated with low glucose levels.
- Criteria for borderline cases:
- Exudates have a protein level of >30 g/L, transudates have a protein level of <30 g/L
- If the protein level is between 25 and 35 g/L, Light’s criteria should be applied.
The BTS recommend using the criteria for borderline cases:
exudates have a protein level of >30 g/L, transudates have a protein level of <30 g/L
if the protein level is between 25-35 g/L, Light’s criteria should be applied. An exudate is likely if at least one of the following criteria are met:
Pleural Effusion: Management
- Treat the underlying condition.
- Large effusion: Drainage. Maximum aspiration of pleural fluid at one time is 1000 ml.
- Malignant pleural effusion: Symptomatic and reaccumulate - aspirated to dryness followed by PLEURODESIS. Instillation of a sclerosing agent such as tetracycline or talc (Magnesium silicate).
Flash pulmonary edema
Pediatrics
Pleural effusion or empyema
-
Persistent or recurrent fever after 48 h treatment for pneumonia should raise suspicion of a parapneumonic effusion or empyema.
-
An AP or PA CXR and ultrasound should allow diagnosis and evaluation of the nature of pleural fluid.
-
A small unloculated effusion may resolve with IV antibiotics alone. A diagnostic pleural tap is usually unnecessary.
-
A large loculated empyema with obvious pus and thickened pleura will require drainage.
-
Options include a pigtail chest drain with intrapleural fibrinolytics, video-assisted thoracoscopic surgery (VATs), or early minithoracotomy following chest CT scan.