Ophthalmology
Diabetes Mellitus
-
Most common cause of blindness amongst individuals of working-age (20-65 years).
-
The prevalence of blindness due to DR in Western Communities is estimated as between 1.6-1.9/100,000
Types of Diabetes
Type I Diabetes
- (eventual loss of insulin secretion, mostly in young)
- Diabetic retinopathy appears about 5 years after onset. Z should examine for first time within 5 years
Type II Diabetes
-
They usually have some insulin secretion remaining but develop resistance to insulin. It occurs in an older age group and has several years prior to diagnosis.
- Retinopathy may be present at presentation
Pathology of Diabetic Retinopathy
- Hyperglycaemia causes:
- Basement Membrane thickening
- non-enzymatic glycosylation
- increased free radical activity
- increased flux through the polyol pathway
- osmotic damage
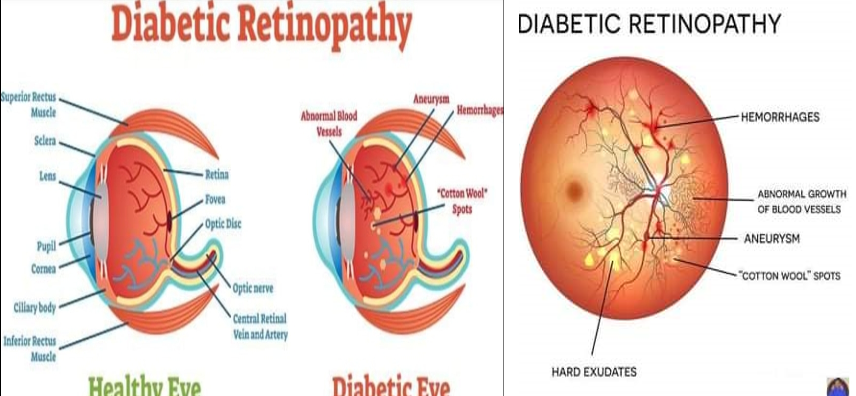
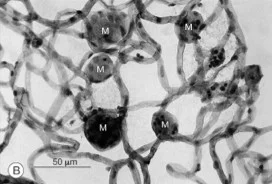
Microscopic Anatomical Changes
Microaneurysms Z
- Pericytes which surround the retinal capillaries are damaged
- Damage to endothelial cells leads to dilated capillaries and venules
- These altered vessels allow serum and blood to leak into the retina
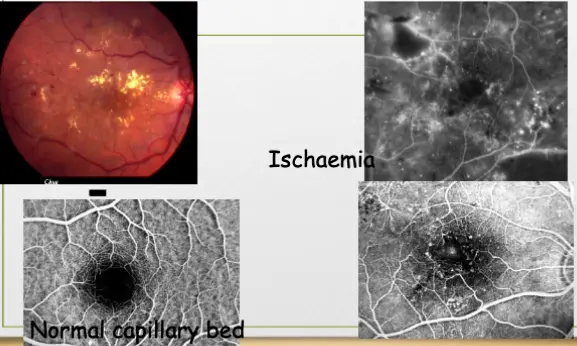
Ischaemia
- Direct effect on Rods and Cones
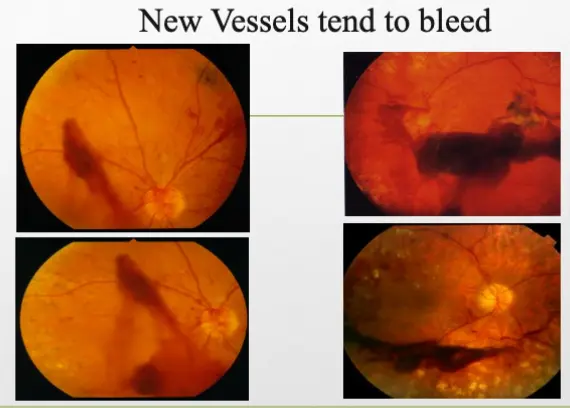
- VEGF release causes new blood vessel formation which bleed and fibrose
- Leakage exudative process damages retinal layers
Retinal Vascular Disease
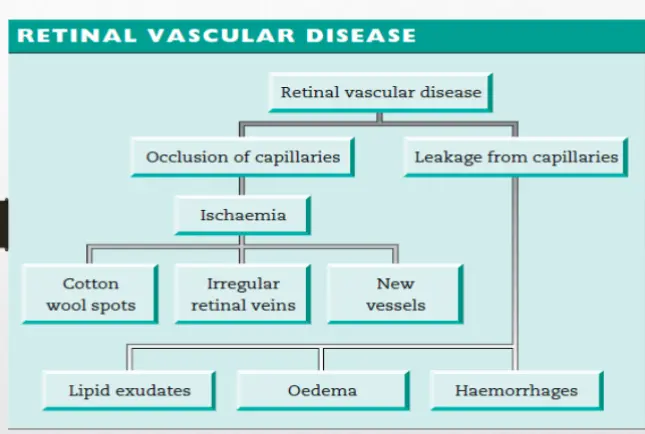
- Retinal vascular disease
- Occlusion of capillaries
- Ischaemia
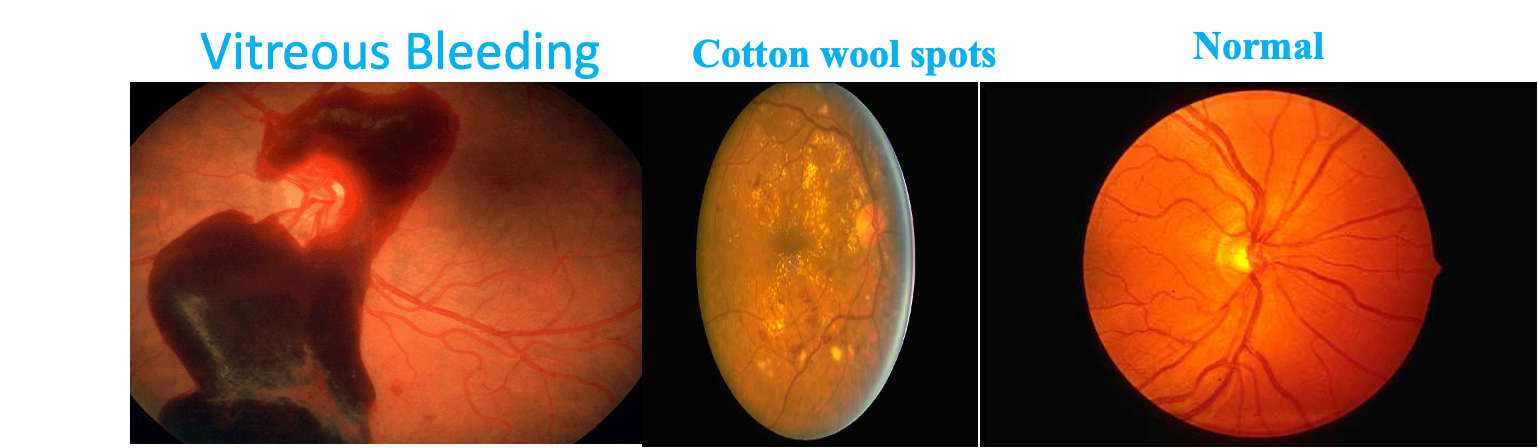
- Cotton wool spots
- Irregular retinal veins
- New vessels
- Ischaemia
- Leakage from capillaries
- Lipid exudates
- Oedema
- Haemorrhages
- Occlusion of capillaries
Eye & Diabetes
-
Visual loss may occur through
- Diabetic retinopathy
- Cataract (complicated or pre-senile)
- Glaucoma
- Ischaemic Optic Neuropathy
- Retinal vein and artery occlusions
- IIIrd, IVth and VIth nerve palsies
History
- Visual acuity may be reduced gradually by a maculopathy and suddenly from a vitreous haemorrhage
- All diabetics should have fundoscopy performed at least yearly.
- Screening for retinopathy (maculopathy and proliferative retinopathy) should begin by 5 years after diagnosis in patients with type I disease, and from the time of presentation in type II disease.
Symptoms & Diagnosis of DR
- No symptoms, so early detection is key
- Gradual visual loss
- Sudden visual loss
Diagnosi
- Fundoscope: Dilated Retinal Eye Exam. Dilation – best way to see clearly into eye
- Fluorescein angiogram performed to determine source of leakage
- OCT
Fluorescein Angiography
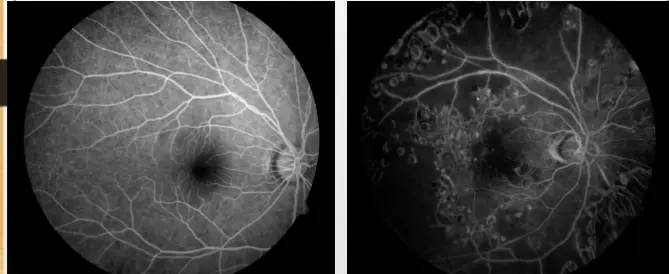
- The left image shows a relatively normal retinal blood vessel structure.
- The right image shows significant abnormalities, including leakage and possible neovascularization, indicative of a pathological condition such as diabetic retinopathy or age-related macular degeneration.
Eye & Diabetes
Stages of Diabetic Retinopathy
- Background (non-Proliferative)
- Preproliferative
- Proliferative
- Maculopathy
Diabetic Retinopathy
NPDR - Background /
Microinfracts of nerve layer
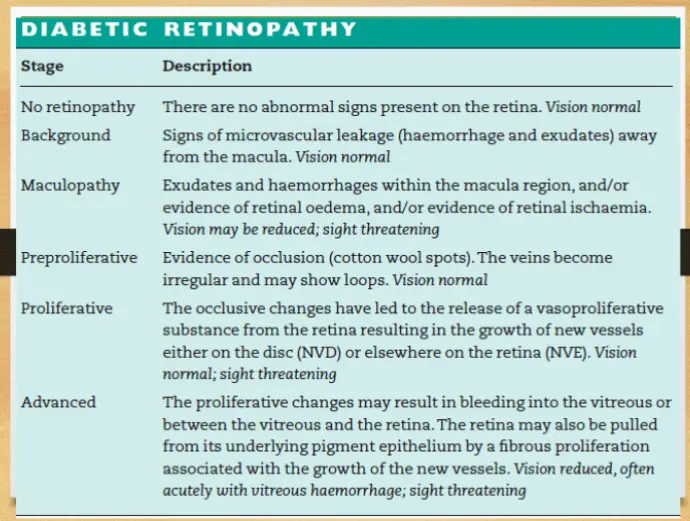
DIABETIC RETINOPATHY
| Stage | Description |
|---|---|
| No retinopathy | There are no abnormal signs present on the retina. Vision normal |
| Background | Signs of microvascular leakage (haemorrhage and exudates) away from the macula. Vision normal |
| Maculopathy | Exudates and haemorrhages within the macula region, and/or evidence of retinal oedema, and/or evidence of retinal ischaemia. Vision may be reduced; sight threatening |
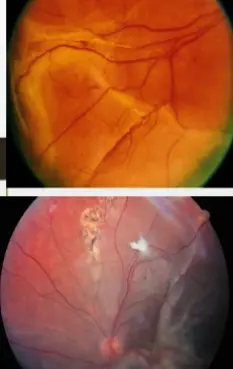
| Preproliferative | Evidence of occlusion (cotton wool spots). The veins become irregular and may show loops. Vision normal |
| Proliferative | The occlusive changes have led to the release of a vasoproliferative substance from the retina resulting in the growth of new vessels either on the disc (NVD) or elsewhere on the retina (NVE). Vision normal; sight threatening |
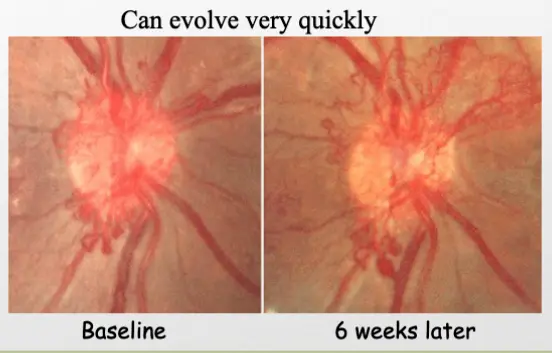
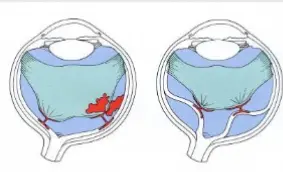
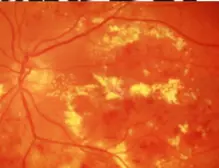
| Advanced | The proliferative changes may result in bleeding into the vitreous or between the vitreous and the retina. The retina may also be pulled from its underlying pigment epithelium by a fibrous proliferation associated with the growth of the new vessels. Vision reduced, often acutely with vitreous haemorrhage; sight threatening |
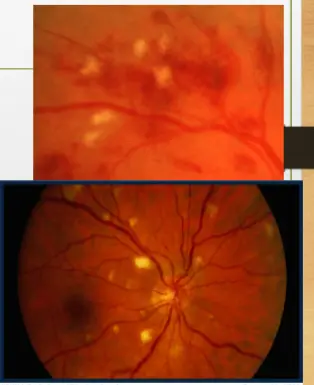
Background / non proliferative DR
Characterised by Mild Haems / Microaneurysm and hard exaudates
no more severe than in this standard photo

Preproliferative retinopathy
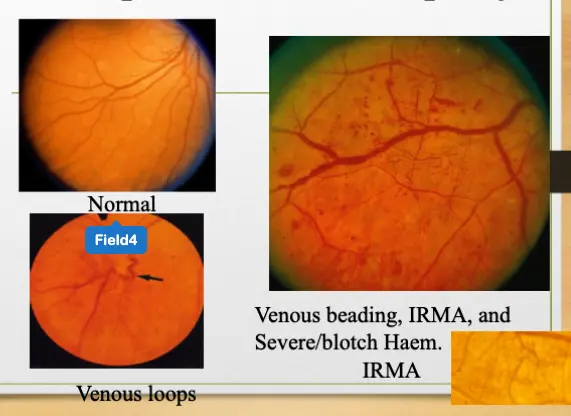
Cotton Wool Spots
- Microinfarcts of nerve fiber layer
- Often associated with other preprolif. DR signs
- If isolated CWS (no other preprolif DR) may be caused by HTN
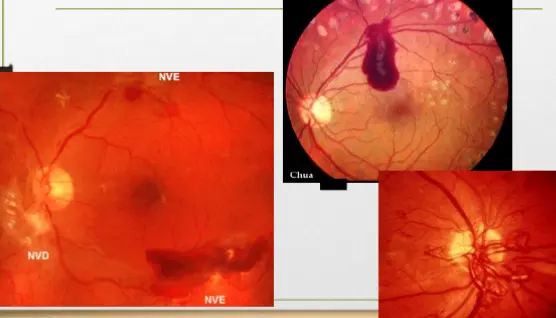
- New vessels grow on the disc (NVD), or elsewhere on the retinal surface (NVE)
Last stage NVD new vessels on disc
NVE elsewhere
Can evolve very quickly
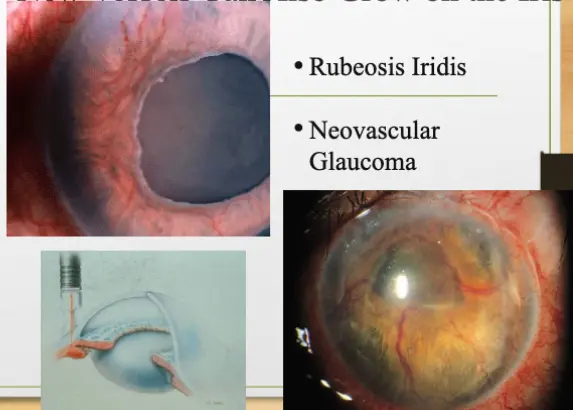
New Vessels Can Also Grow on the Iris
- Rubeosis Iridis
- Neovascular Glaucoma
Rubeoisis iridis, vascular demarcation appearing around cornea
how to treat neovascular glaucoma
- Like treatment of PDR
Late Complications of Proliferative DR
Tractional Retinal Detachment
Diabetic maculopathy
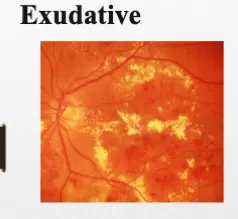
Exudative
-
Exudates: intraretinal accumulations of lipids leaking from abnormal retinal capillaries and microaneuryisms
-
Leakage of fluid that distorts the retinal architecture
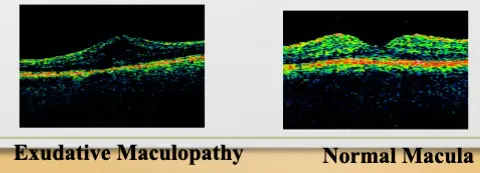
Ischaemic + Mixed exudative/ischaemic
Z diabetic maculopathy
Exudative microanureysms, spots instrumentall oct - ocular ct
OCT findings Green - normal, Yellow- border line, Red - Abnormal
Maculopathy black spots with no details ischemic demarcations - blackout
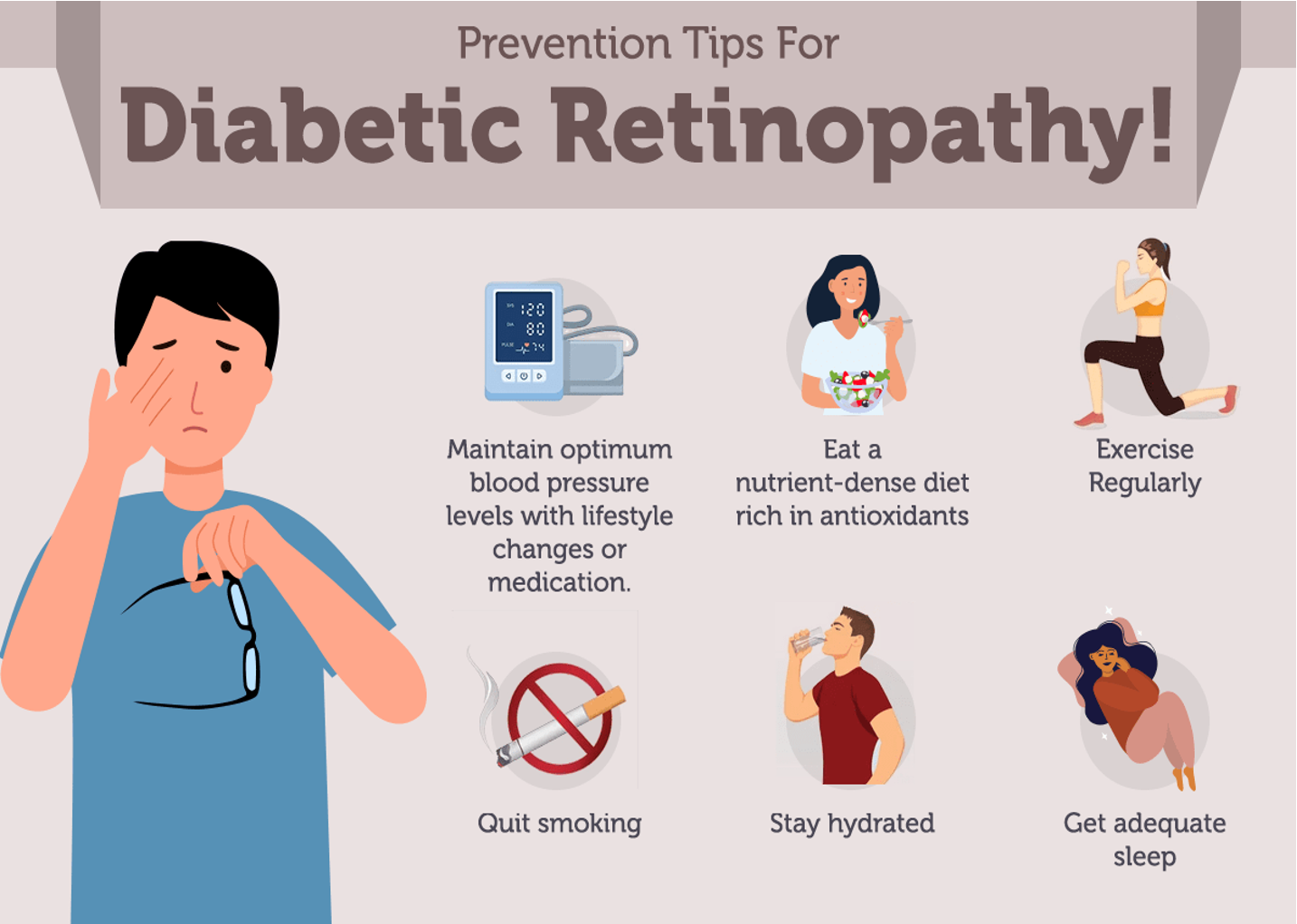
Treatment of Diabetic Retinopathy
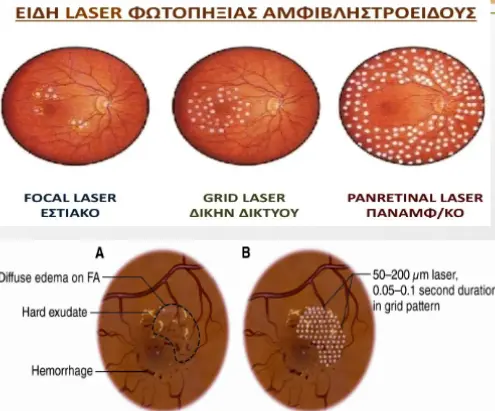
- Focal laser/laser grid for exudative maculopathy.
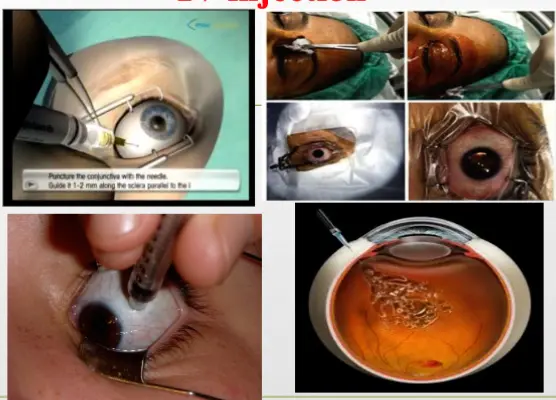
- Intravitreal injection of steroid or AVEGF.
- Scattered laser pan retinal photocoagulation (PRP) for PDR
- Optic disc and retinal new vessels are treated with scattered laser (PRP) preventing the release of vasoproliferative factors. This results in the regression of the new vessels and prevents the development of advanced retinopathy.
Focus on treating the following
- Diet and exercise - lipidemia, hyperglycemia
- Sit with patient explain the disease for adherence
Treatment of Diabetic Retinopathy
- Ischaemic Maculopathy NOT treatable
- Surgical treatment( vitrectomy): of complicated cases as vitreous Hge and retinal detachement
C Z is it nonproliferative or not, differentiates treatment option
if non - Argon laser photocoagulation (grade pattern), antiivgf, surgery…??
Abnormal - (PrP), surgery refractive cases
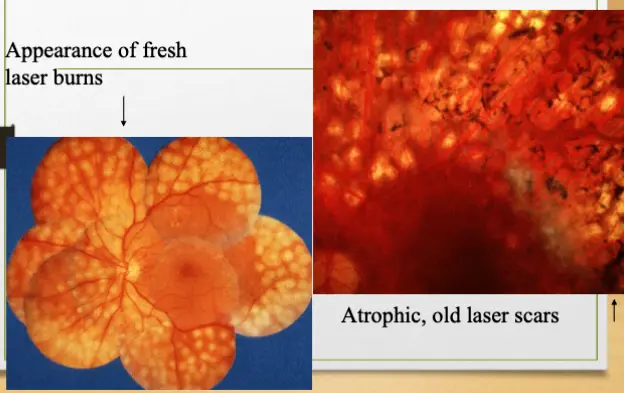
PRP
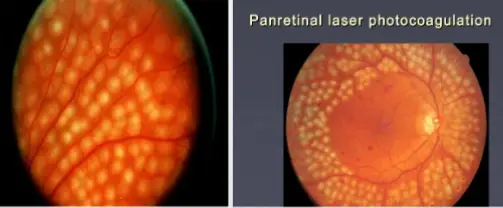
Panretinal laser photocoagulation (PRP) for proliferative DR
- Appearance of fresh laser burns
- Atrophic, old laser scars
IV injection
Systemic Risk Factors and DR
-
Blood sugar and BP control are as good as laser treatment for reducing the risk of retinopathy progression and loss of vision
-
Nephropathy is a risk factor for DR
Hyperlipidaemia and diabetic maculopathy
There is evidence that diabetics who have exudative maculopathy with extensive lipid exudates benefit from active treatment of hyperlipidaemia
Therapeutics
it is 3 stages
I. Stage of Diabetes without retinopathy:
II. Stage of non proliferative retinopathy( Background retinopathy):
III. Stage of Proliferative retinopathy : due to damage of retinal capillaries leading to ischemia which stimulate release of VEGF and formation of new capillaries
Clinical presentation:
- Asymptomatic
- Blurred vision,floaters,blindness
pathological lesions:
- Microaneurysm - earliest sign.
- Hemorrhage. Dot’s (microaneurysm) and blot’s (hemorrhages)
- Macular edema.
- Vascular occlusion leads to large ischaemic areas producing infarcted areas (cotton-wool spots).
Other Eye Complications:
- Cataracts,glaucoma at earlier age than non diabetic persons.
- Vitreous Bleeding.
Management of Diabetic retinopathy
I. Asymptomatic patients :
-blood glucose regulation
-yearly eye examination
II- Symptomatic patients
-
Metabolic control: A- glycemic control HBA1C ﹤7% B- Blood pressure ﹤130/80mmHg
-
Antiangiogenic factor: using monoclonal antibodies that bind to vascular endothelial growth factor(VEGF).
-
Retinal laser photocoagulation with local anathesia: specialy in patients with proliferative retinopathy stage.
-
surgery: e.g vitrectomy specialy if there is hemorrhage interfere with vision