Neonate with Respiratory Distress
Case-Based Discussion
Dr. Faten Zaidan
Case 1
A 35-week gestational age infant is born by cesarean delivery to a mother with placenta previa. The infant girl is vigorous after delivery with an APGAR score of 8 at 5 minutes. Fifteen minutes later, she started to experience worsening respiratory distress with tachypnea, retractions, and mild grunting. CPAP at 40% FiO2 was started, and she was admitted to the NICU.
- Questions:
-
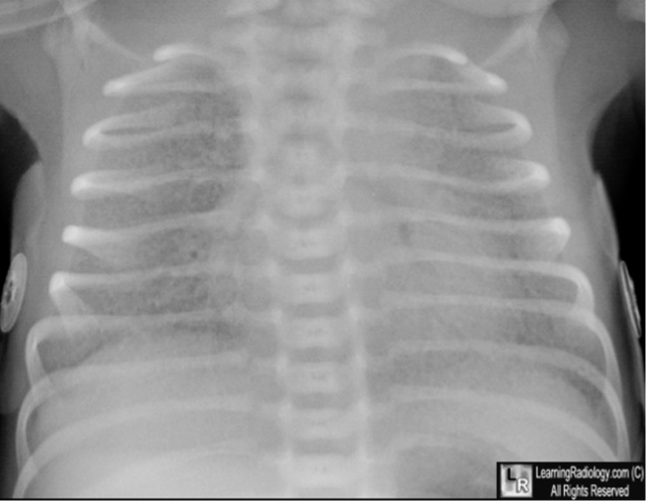
Xray findings
- Prominent perihilar streaking reflecting fluid in the interstitium
- Patchy infiltrates
- Fluids in the horizontal fissure on fifth right costal
- Hyperinflated lung
-
What is your diagnosis? Transient Tachypnea of the Newborn (TTN)
-
What is the definite treatment? *Supportive as it is self-limited; oxygen (nasal cannula) if needed.
-
- Chest X-ray Findings:
Case 2
A 39-week gestational age infant is born after prolonged rupture of membranes. The mother presented with a fever of 39°C, foul-smelling amniotic fluid, and severe abdominal pain. She was started on antibiotics shortly before delivery. The infant is born by CS due to consistent fetal tachycardia and transferred to the NICU. The infant started to have respiratory distress, apneic episodes, mild retractions, and grunting.
- Questions:
- What is your diagnosis? neonatal pneuomonia/sepsis?
- What is your course of treatment?
- antibiotic, oxygen supplementation, suctioning, admission to icu, DO NOT ELECTIVELY INTUBATE
 Early BPD changes in Ureaplasma urealyticum pneumonia on day 18 of life
Early BPD changes in Ureaplasma urealyticum pneumonia on day 18 of life
Case 3
A postterm 42 3/7 week gestational age infant is born after induced vaginal delivery. Meconium-stained fluid was noted after rupture of membranes approximately 6 hours before delivery. The infant’s head was delivered easily; however, the infant’s body was delivered 4 minutes after the delivery of the head, causing shoulder dystocia. The infant at 5 minutes was cyanosed, had a weak cry, mild flexion of the limbs, no spontaneous movements, with a heart rate of 160.
-
Question:
-
Calculate his APGAR score. 4 - bad score, need to admitted to icu
-
What do you expect the cause of respiratory distress to be?
- Meconium aspiration syndrome
-
Name two possible complications:
- Chemical pneumonitis (antibiotic = ampicillin and gentamicin)
- Pneumothorax
- Respiratory distress syndrome (RDS)
-
-
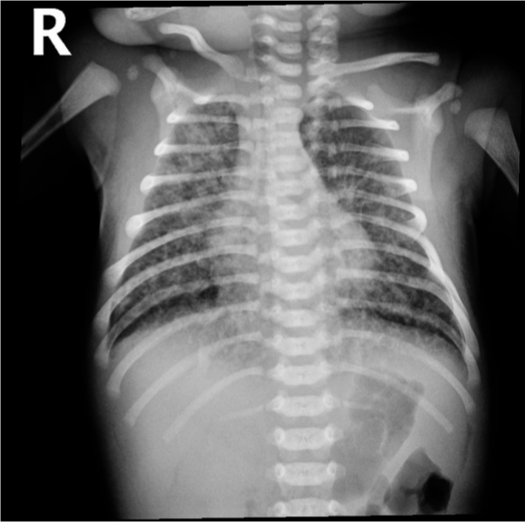
Xray findings
- Hyperinflation,
- Consolidation,
- Patchy infiltrates
- If severe, air leak and pneumomediastinum may occur
- Lines going from inside to outside
The infant has been on a ventilator for about 6 hours when you are called to the bedside for sudden decompensation with decreased saturations as low as 30%, bradycardia, and absent breath sounds on the right.
- Questions:
- What do you expect happened? pneumothorax
- What is your immediate action? right needle decompression 2nd intercostal mid clavical
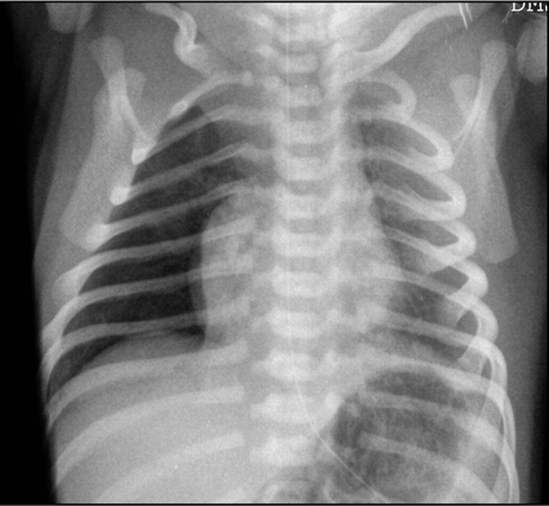 well demarcated right lung pnumothorax - pushed
well demarcated right lung pnumothorax - pushed
effusion pulls
Case 4
A preterm infant born at 25 weeks gestation is now 6 weeks old. The infant has been stable for the past few weeks, breathing in room air, and receiving full enteral feedings that consist of fortified maternal breast milk and some formula supplementation. Yesterday, the infant had a few large gastric residuals with feeding but was otherwise well. Today, you were called for a new onset of apneic spells, increased abdominal distension, poor urine output, lethargy, and hypothermia.
- Questions:
-
What is your spot diagnosis? necrotizing enterocolitis
-
What labs will you ask for?
- Hyponatremia
- Metabolic acidosis
- Thrombocytopenia
- Leukopenia or leukocytosis
- Prolonged PT and aPTT
- Decreasing fibrinogen
-
What is your action?
- NPO; bowel rest
- Nasogastric tube for continous suctioning
- IV Antibiotic
- Call surgery
- Abdominal x-ray
-

- Dilated loops,
- thickened bowel walls,
- pneumatosis intestinalis (air in intestinal walls),
- pneumoperitoneum; indicate perforation (emergency requiring surgical intervention),
- portal gas (present in the portal venous system,
- considered to be a poor prognostic sign).
Further Deterioration
Despite your treatment, the patient deteriorated and was admitted to the NICU.
- Question:
- What is your action? immediate surgery
 inflamed, necrosis ⇒ Perforation everywhere
dark circles air in intestinal wall
inflamed, necrosis ⇒ Perforation everywhere
dark circles air in intestinal wall
Air in portal gas
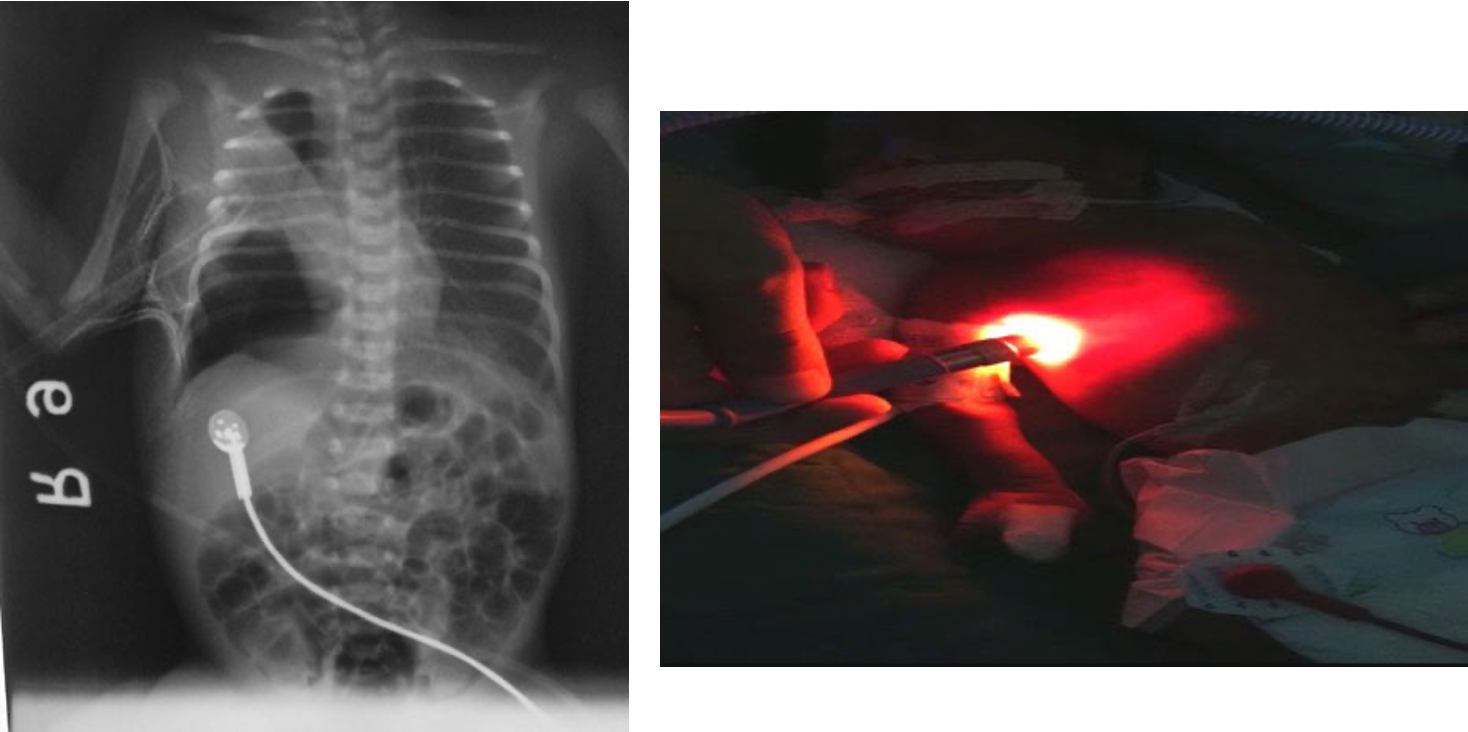 if light goes throughout lung theres pneumothoraxm if localized, its not pneumothorax.
if light goes throughout lung theres pneumothoraxm if localized, its not pneumothorax.
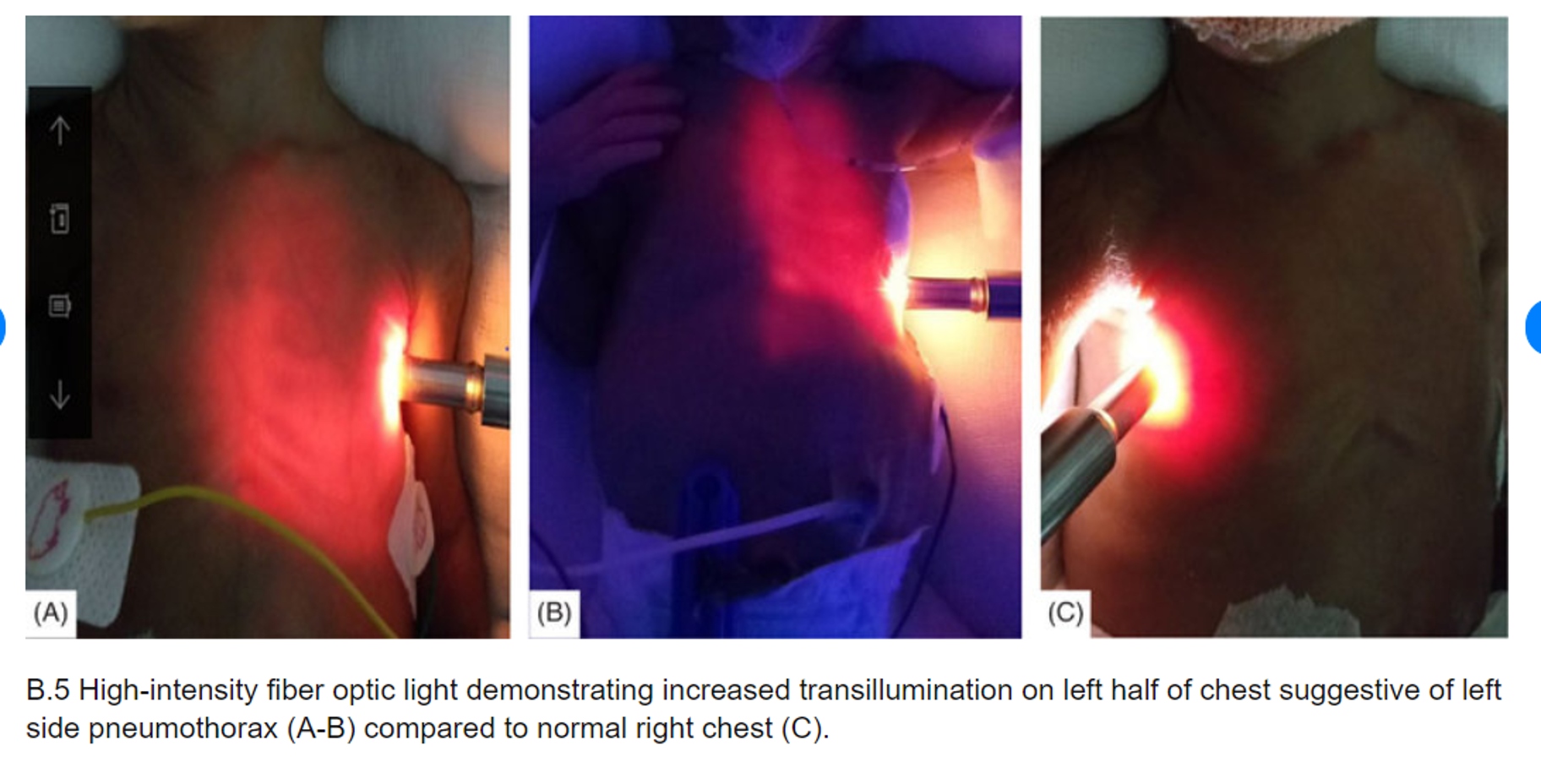 High-intensity fiber optic light demonstrating increased transillumination on the left half of the chest suggestive of left-side pneumothorax compared to the normal right chest.
High-intensity fiber optic light demonstrating increased transillumination on the left half of the chest suggestive of left-side pneumothorax compared to the normal right chest.
Deep Sulcus Line
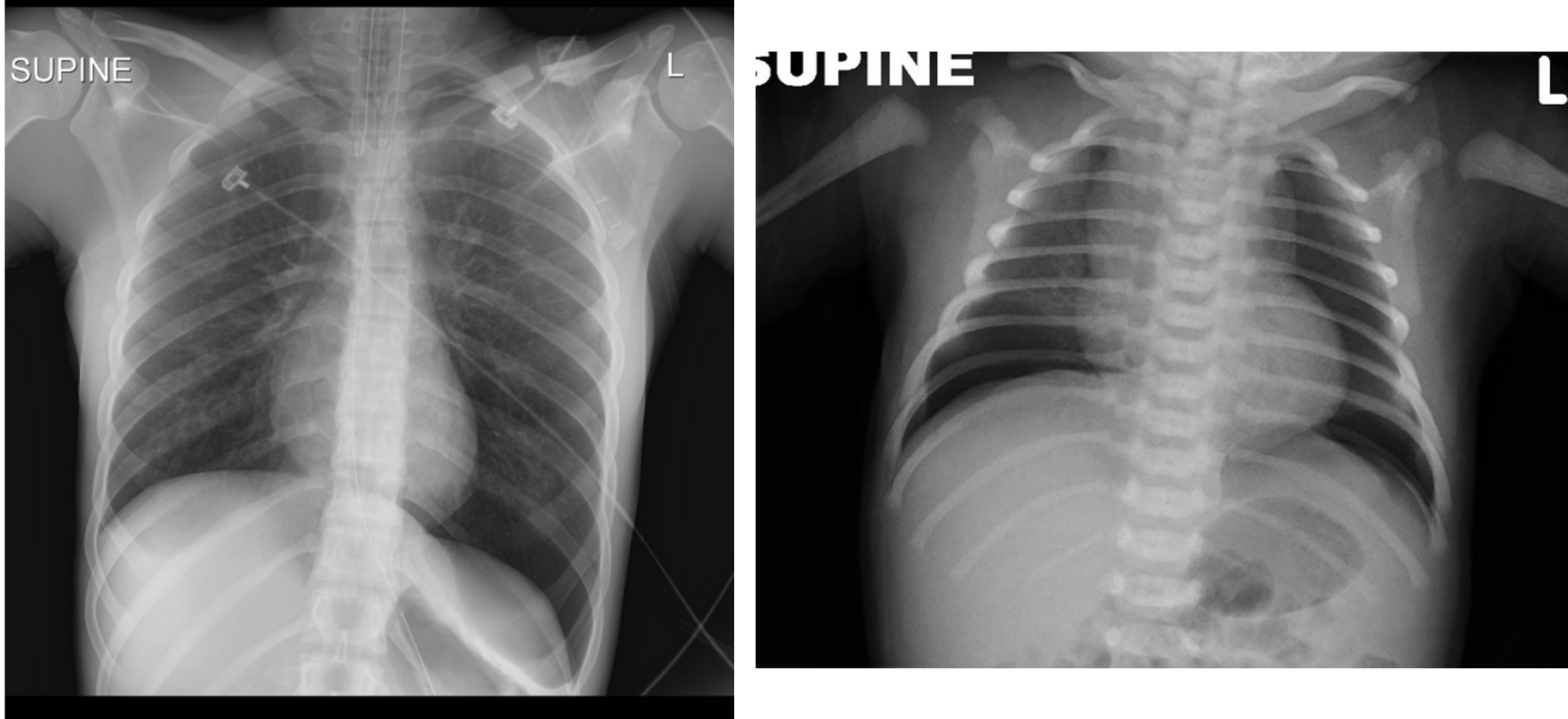
- Notice:
“Deep sulcus line” indicating pneumothorax.
Continuous Diaphragm Sign

- Description:
The blue arrow points to the “continuous diaphragm sign.” The entire diaphragm is visualized from one side to the other because air in the mediastinum outlines the central portion, which is usually obscured by the heart and mediastinal soft tissue structures that are in contact with the diaphragm. The red arrow points to the air beneath and posterior to the heart. Pneumomediastinum elevating the thymus causing the “spinnaker sail” sign. Notice also the “continuous diaphragm line.”
Pneumoperitoneum

- Notice:
Pneumoperitoneum. - due perforations